- Department of Neurosurgery, Yale University School of Medicine, 20 York Street, LCI 8, New Haven, Connecticut, United States.
DOI:10.25259/SNI_125_2019
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Christopher S. Hong, E. Zeynep Erson-Omay, Jennifer Moliterno. Multiple meningiomas arising within the same hemisphere associated with Li-Fraumeni syndrome. 17-Mar-2021;12:99
How to cite this URL: Christopher S. Hong, E. Zeynep Erson-Omay, Jennifer Moliterno. Multiple meningiomas arising within the same hemisphere associated with Li-Fraumeni syndrome. 17-Mar-2021;12:99. Available from: https://surgicalneurologyint.com/surgicalint-articles/10652/
Abstract
Background: While meningiomas are some of the most common intracranial tumors, the presence of multiple ones at the time of presentation is rare and can most commonly be observed in patients with well-described syndromes (i.e., neurofibromatosis type 2) or those with prior cranial radiation history. In others, however, the pathophysiology remains unclear.
Case Description: A 49-year-old female with no significant personal or familial oncologic medical history presented with a generalized seizure and was found to have ten meningiomas arising within the right hemisphere. She underwent a two-staged resection of all tumors, with pathology revealing the World Health Organization Grade I meningioma. Whole-exome sequencing revealed somatic NF2 mutations and heterozygous deletion of chromosome 22 overlapping with NF2, and analysis of the germline uncovered mutations of TP53, rendering a diagnosis of Li-Fraumeni Syndrome.
Conclusions: This case represents a novel presentation of multiple meningiomas in a patient with newly diagnosed Li-Fraumeni syndrome, suggesting meningioma may be considered as part of this tumor-predisposed patient population.
Keywords: Li-Fraumeni, Meningioma, TP53
INTRODUCTION
While meningioma is one of the most common types of intracranial tumor, the presence of multiple meningiomas occurs in approximately 10% of these patients at the time of diagnosis.[
CASE DESCRIPTION
A 49-year-old female presented with a new-onset generalized seizure and was found to have multiple hyperdense masses with calcifications in the right hemisphere on computed tomography. A brain magnetic resonance imaging with and without contrast demonstrated ten distinct dural-based, homogeneously enhancing lesions within the right hemisphere (
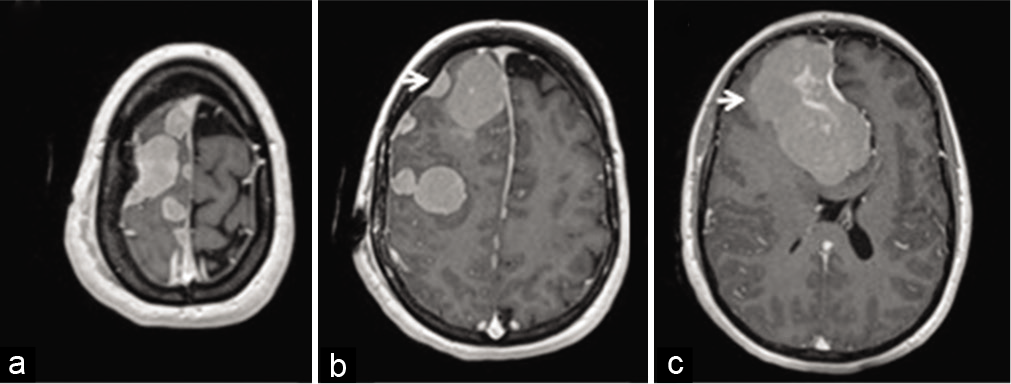
Figure 1:
Magnetic resonance imaging of multiple meningiomas arising within the same hemisphere. (a-c) Representative axial slices of T1-weighted magnetic resonance images after gadolinium contrast administration are shown. The arrows point to the (b) smaller frontal convexity tumor (c) and dominant parafalcine tumor, targeted through surgical resection.
She was taken to the operating room for resection of the dominant right parafalcine mass (arrow,
WES of all tumors revealed the same somatic NF2 nonsense mutation and chromosome 22 deletions with otherwise normal copy numbers of all other chromosomes. Additional somatic mutations unique to each sample were discovered, but likely non-pathogenic as none were previously characterized as oncogenic [Supplementary Table]. Together, these findings suggested that all tumors originated from the same founding clone.
DISCUSSION
The differential diagnosis for multiple dural-based lesions includes meningioma and metastasis, but the appearance and lack of vasogenic edema typically favors the former. Among the approximate 10% of meningioma patients harboring multiple tumors at the time of diagnosis,[
The pathogenesis of multiple meningioma formation remains poorly understood. Early theories hypothesized spread of original clonal tumor cells through the cerebrospinal fluid.[
In the patient presented, the relevance of the germline TP53 mutations remains unclear. While TP53 mutations have been frequently described in other brain tumors, such as gliomas, there have been more limited reports in meningioma. They have typically been reported in higher grade meningiomas[
Management of multiple meningiomas, such as solitary tumors, remains maximal surgical resection when tumors become symptomatic or reach significant size with associated mass effect. While there is currently no effective chemotherapy for meningiomas, adjuvant radiotherapy can often times be used in patients with multiple meningiomas, particularly for residual tumors or those with growing tumors that may pose a high surgical risk due to wound considerations.[
CONCLUSION
Although the role of germline TP53 mutations in the formation of multiple meningiomas remains unclear, this case is a novel presentation of multiple meningiomas in a patient with newly-diagnosed Li-Fraumeni syndrome, in the absence of more common predisposing risk factors. Multiple meningiomas may be considered as part of the spectrum of tumors that can develop in patients with Li-Fraumeni syndrome and given its implications in the overall treatment, seemingly important to recognize and consider.