- Department of Ortho-Spine Surgery, Sir Ganga Ram Hospital, New Delhi, Delhi, India.
DOI:10.25259/SNI_50_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prem Bahadur Shahi, Vishnuprasad Panigrahi, Nitin Adsul, Manoj Kumar, Shankar Acharya, K. L. Kalra, R. S. Chahal. Mycobacterium abscessus mimicking tubercular spondylodiscitis following ozone therapy: A case report and review of literature. Surg Neurol Int 04-Apr-2020;11:63
How to cite this URL: Prem Bahadur Shahi, Vishnuprasad Panigrahi, Nitin Adsul, Manoj Kumar, Shankar Acharya, K. L. Kalra, R. S. Chahal. Mycobacterium abscessus mimicking tubercular spondylodiscitis following ozone therapy: A case report and review of literature. Surg Neurol Int 04-Apr-2020;11:63. Available from: https://surgicalneurologyint.com/surgicalint-articles/9950/
Abstract
Background: The incidence of Mycobacterium abscessus (MA), a rapidly growing species of nontuberculous mycobacteria (NTM)-related infections, has been steadily rising over the past decade. Despite the increased prevalence of NTM-related infections, it is largely underreported from TB-endemic countries due to lack of awareness and limited laboratory facilities. Here, we report a rare case of L4–L5 spondylodiscitis caused by MA following ozone therapy (a noncondoned method of lumbar disc management).
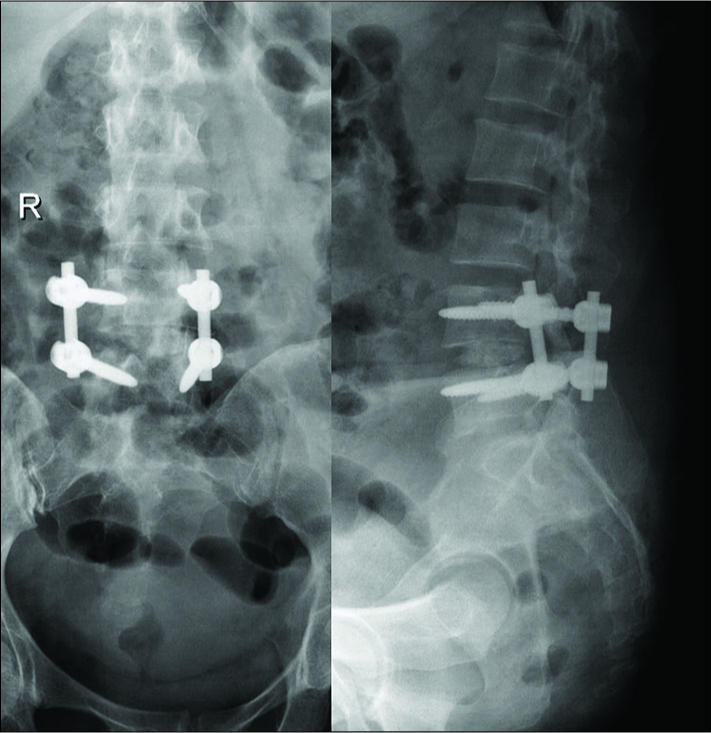
Case Description: A healthy, nonimmunocompromised 43-year-old female presented with bilateral lower extremity radiculopathy. She underwent a fluoroscopically guided percutaneous ozone treatment for degenerated disc disease at the L4–L5 level. She was symptom free for 3 months duration. She then presented with severe low back pain, bilateral lower extremity radiculopathy, and spondylodiscitis at the L4–L5 level. This was treated with a L4–L5 transforaminal lumbar interbody fusion. MA was cultured from the epidural purulent material collected during the surgery. The patient was discharged on oral clarithromycin 500 mg twice daily and intravenous amikacin 500 mg twice daily for 6 weeks. The plan was to then continue oral clarithromycin for another 6 weeks till resolution of primary infection.
Conclusion: Early diagnosis and appropriate therapy is required to treat NTM which is more prevalent in epidemic/endemic regions.
Keywords: Mycobacterium abscessus, Ozone therapy, Spondylodiscitis
INTRODUCTION
Nontuberculous mycobacteria (NTM) have over 170 different species that are correlated with different degrees of virulence.[
CASE REPORT
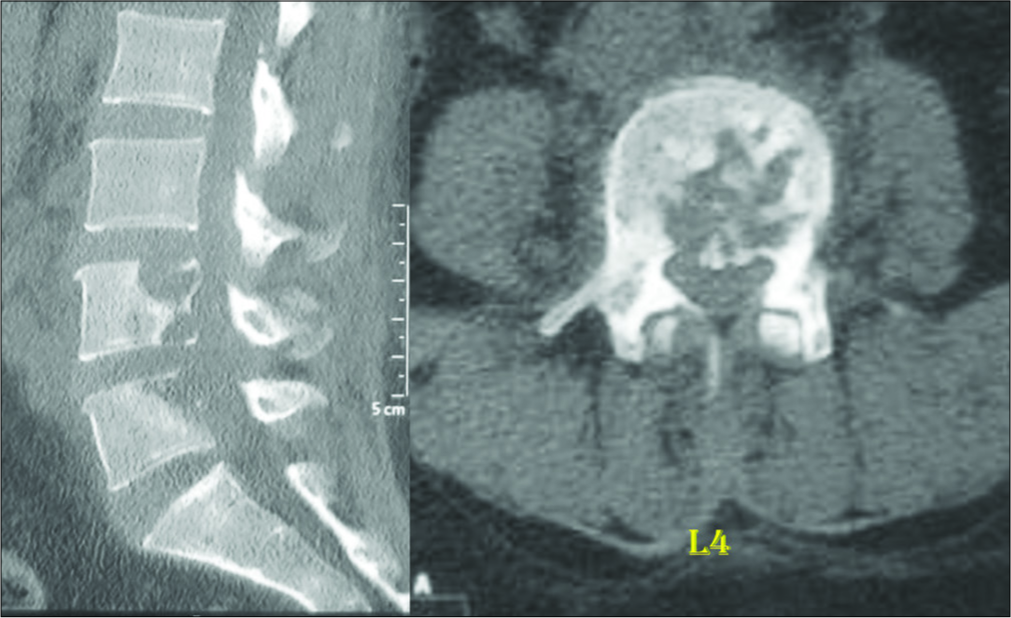
A healthy, nonimmunocompromised 43-year-old female with bilateral lower extremity radiculopathy had a fluoroscopically guided percutaneous ozone treatment for degenerative lumbar disc disease [
Diagnostic studies
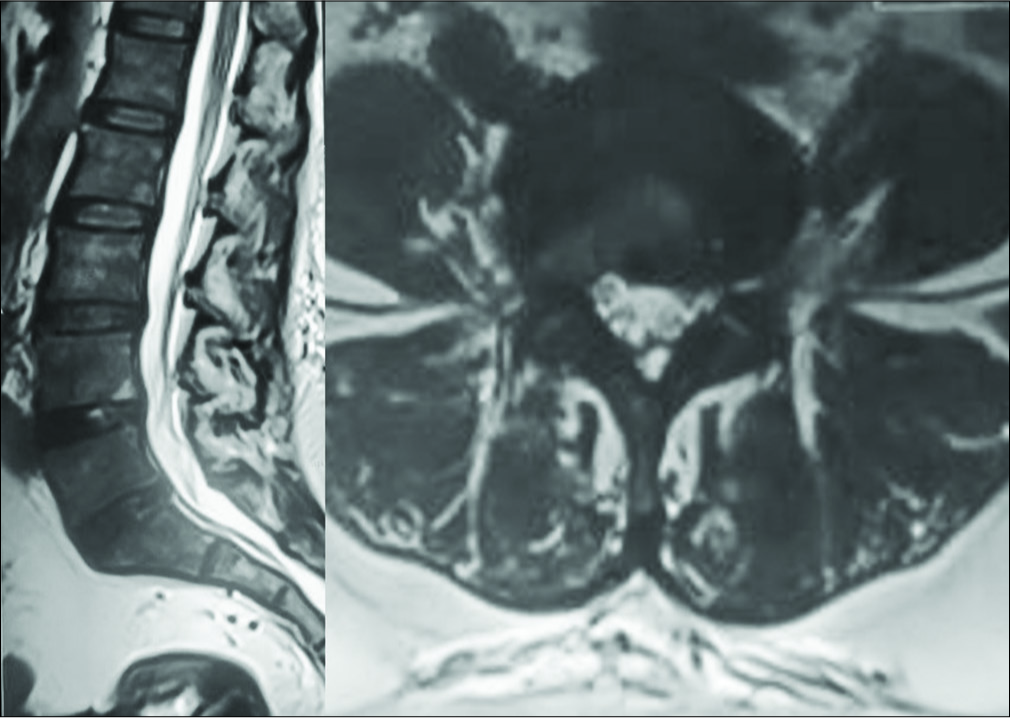
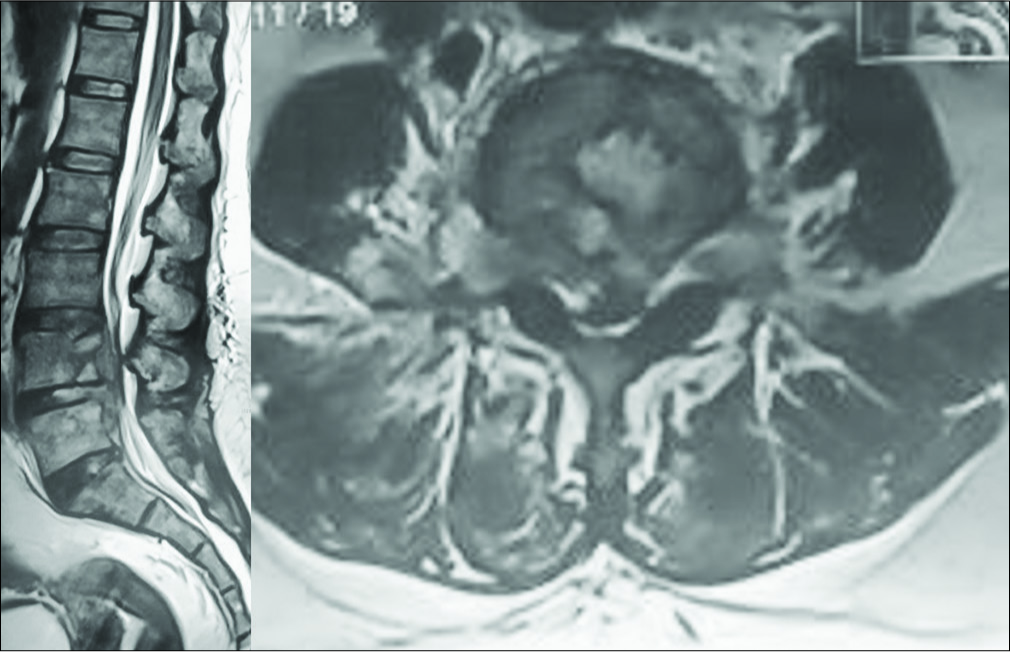
The repeat MR of the lumbar spine demonstrated L4–L5 spondylodiscitis [
Treatment
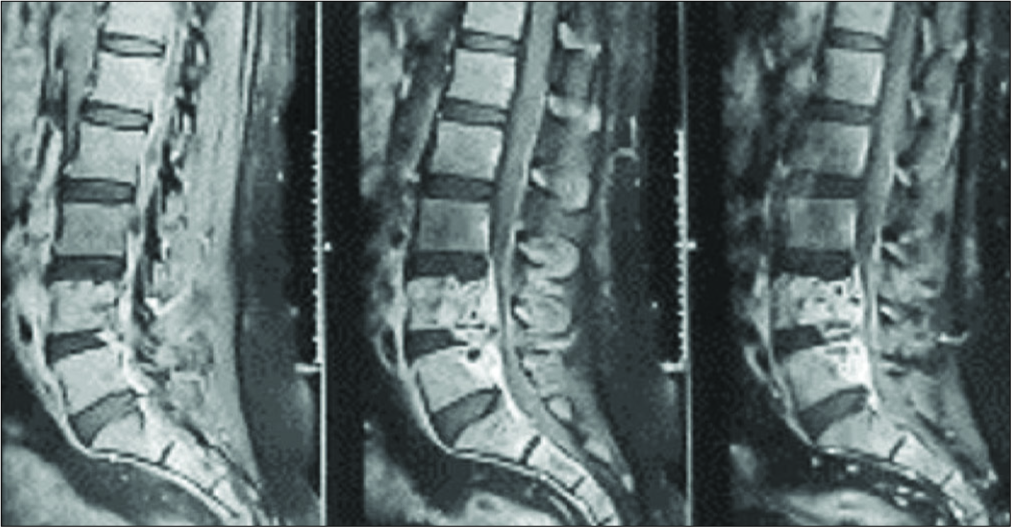
The patient was discharged on intravenous cefoperazone- sulbactam 1.5 g twice daily. She, however, returned after 6 weeks with a fluid collection in the wound, and the CRP and ESR studies remained elevated. The wound was debrided and then she was discharged on intravenous amikacin 500 mg (intravenously) twice daily for 6 weeks, supplemented with oral clarithromycin 500 mg twice daily. Subsequently, she was continued on oral clarithromycin for another 6 weeks following resolution of the primary infection.
DISCUSSION
Ozone therapy is not a condoned treatment for lumbar disc disease within or outside of the US. Here, we report a rare case of spondylodiscitis attributed to MA following percutaneous ozone treatment for a lumbar disc herniation.
What is MA
MA is a rapidly growing mycobacterium that is ubiquitous in the soil and aqueous environments and has the potential to colonize human epithelia. MA has a bimodal age distribution (age: 0–4 years and >65 years) and has become more prevalent but less adequately recognized in regions previously impacted by TB.
Antibiotic Therapy for MA
Spinal infections due to MA require 2–3 antibiotics for treatment as monotherapy usually fails. The antibiotics of choice include clarithromycin, while imipenem, cefoxitin, and amikacin also play a role. Further, dual therapy should be continued for a minimum of 6 weeks after the initial diagnosis/treatment/surgery; once the infection has “resolved,” an additional 6 weeks of “suppressive” oral clarithromycin therapy should considered.[
Surgery
Surgical decompression may be warranted to both diagnose and treat pyogenic osteomyelitis, i.e., epidural or paravertebral abscess formation, threatened/actual cord compression due to vertebral collapse, epidural compression, and/or spinal instability.
Reduction of morbidity/mortality
The best way to reduce the morbidity and mortality associated with MA is to shorten the time between the onset of symptoms, the time it takes to establish the diagnosis, when appropriate therapy is initiated.
CONCLUSION
The symptoms/signs of spinal NTM are typically underappreciated/underreported from TB-endemic countries. Since early diagnosis and appropriate therapy yield the best clinical outcomes, one should exercise great vigilance looking for MA in TB/NTM epidemic/endemic regions.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Andrés-Cano P, Vela T, Cano C, García G, Vera JC, Andrés-García JA. Cervical spondylodiscitis after oxygen-ozone therapy for treatment of a cervical disc herniation: A case report and review of the literature. HSS J. 2016. 12: 278-83
2. Baldwin SL, Larsen SE, Ordway D, Cassell G, Coler RN. The complexities and challenges of preventing and treating nontuberculous mycobacterial diseases. PLoS Negl Trop Dis. 2019. 13: e0007083-
3. Jeong SH, Kim SY, Huh HJ, Ki CS, Lee NY, Kang CI. Mycobacteriological characteristics and treatment outcomes in extrapulmonary Mycobacterium abscessus complex infections. Int J Infect Dis. 2017. 60: 49-56
4. Kadota N, Shinohara T, Hino H, Goda Y, Murase Y, Mitarai S. Mycobacterium abscessus ssp. abscessus infection progressing to empyema from vertebral osteomyelitis in an immunocompetent patient without pulmonary disease: A case report. BMC Pulm Med. 2019. 19: 100-
5. Moral MZ, Desai K, Arain AR, O’Leary RE, Haddad SF, Lawrence JP. Mycobacterium abscessus associated vertebral osteomyelitis in an immunocompetent patient: a rare case report and literature review. Spinal Cord Ser Cases. 2019. 5: 53-
6. Petrini B. Mycobacterium abscessus An emerging rapid-growing potential pathogen. APMIS. 2006. 114: 319-28