- Department of Neurologic Surgery Mayo Clinic, Rochester, Minnesota, United States.
- Department of Radiation Oncology, Mayo Clinic, Rochester, Minnesota, United States.
Correspondence Address:
Ahmed Helal, Departments of Neurologic Surgery, Mayo Clinic, Rochester, Minnesota, United States.
DOI:10.25259/SNI_590_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Helal1, Anthony L. Mikula1, Nadia N. Laack2, William E. Krauss1, Michelle J. Clarke1. Myxopapillary ependymomas; proximity to the conus and its effect on presentation and outcomes. 30-Aug-2021;12:429
How to cite this URL: Ahmed Helal1, Anthony L. Mikula1, Nadia N. Laack2, William E. Krauss1, Michelle J. Clarke1. Myxopapillary ependymomas; proximity to the conus and its effect on presentation and outcomes. 30-Aug-2021;12:429. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11080
Abstract
Background: Myxopapillary ependymomas (MPE) are intradural spinal tumors with a predilection to the filum terminale. Damage to conus medullaris during surgery can result in sphincteric and sexual dysfunction. The purpose of this study is to determine how myxopapillary ependymoma proximity to the conus impacts patient presentation, extent of resection, and clinical outcomes.
Methods: Fifty-one patients who underwent surgical resection of pathologically confirmed myxopapillary ependymoma with at least 1 year of follow-up were included in the study. We collected initial presenting symptoms, distance of the tumor from the conus, extent of resection, and postoperative clinical outcomes including bladder dysfunction.
Results: Average age was 38 years (range 7–75 years) with a male to female ratio of 1.43:1. Patients most commonly presented with pain symptoms (88%), and 12 patients (23.5%) had urologic symptoms on presentation. The mean tumor distance from the tip of the conus was 1.60 cm (10 cm above to 21 cm below the tip of the conus). Patients with tumors in contact with the conus had a significantly higher rate of preoperative urinary symptoms and were more likely (32% vs. 14%) to suffer postoperative urinary sphincteric disturbances. Tumors with direct invasion of the conus medullaris were more likely to require intralesional resection and fail to achieve a gross total resection (GTR).
Conclusion: Patients with MPE in close proximity to the conus were more likely to suffer from long-term morbidity related to urologic issues following surgical resection. Adjuvant radiotherapy may be a viable option for patients who fail to achieve GTR.
Keywords: Conus, Ependymoma, Myxopapillary, Outcome, Predictors
INTRODUCTION
Spinal cord ependymomas comprise 35–40% of all primary spinal cord tumors and can be classified into a number of different subtypes, including myxopapillary ependymomas (MPE).[
MATERIALS AND METHODS
This study was approved by the Mayo Clinic institutional review board (IRB); all patients provided informed consent for using clinical data for research purposes. A retrospective chart review was performed from 1995 to 2019 to identify patients with pathologically proven MPE. Patients without a preoperative MRI, sufficient operative detail, or <12 months of follow-up were excluded from the study. Baseline demographic data including age, gender, and clinical presentation details were collected. Preoperative MRI was used to determine tumor location, tumor size, distance between the superior- and inferior-most poles of the tumor, presence or absence of CSF metastases, and proximity to the conus. Proximity the conus was defined on MRI as the distance between the superior pole of the tumor and the inferior tip of the conus. Tumors in which the superior pole of the tumor was at or above the tip of the conus were considered to be in contact with the conus and were further subdivided depending on whether they appeared to be invading or displacing the conus on imaging.
Operative notes were used to determine extent of resection, whether an en bloc resection, piece meal GTR, in which a complete resection was performed with violation of tumor capsule, or a sub-total resection (STR). In lesions involving the conus, drop metastases of the cul-de-sac were considered separately with regard to technique and extent of resection. Postoperative MRI was evaluated to confirm extent of resection. There was no discrepancy between intra-operative findings and postoperative MRI in our series. Follow-up data included any adjuvant therapy, clinical performance at last follow-up, and details regarding recurrence. Preoperative and postoperative urinary disturbances were collected including retention, urgency, hesitancy, as well as any form of incontinence.
Statistical analysis was performed using JMP software version 14 (SAS Institute Inc., Cary, North Carolina, USA). Chi-square test and Fischer exact test compared preoperative, intra-operative, and postoperative variables and outcomes including urinary sphincteric disturbances, technique of resection, extent of resection, and recurrence rates.
RESULTS
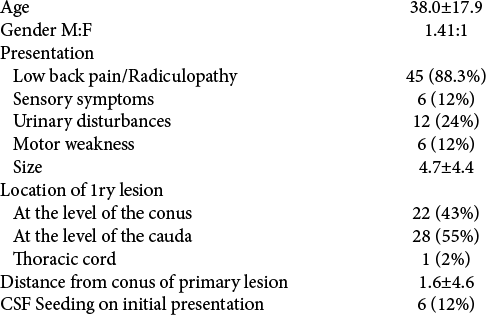
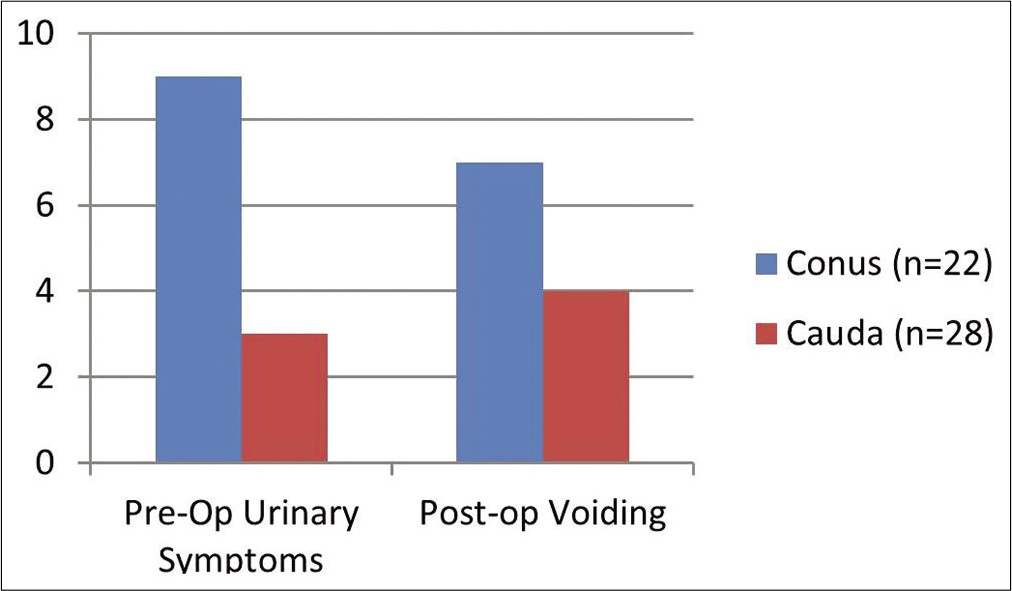
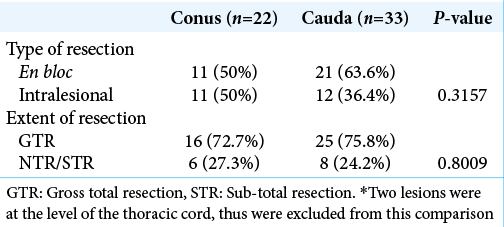
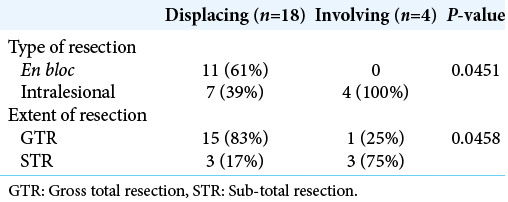
We identified 51 patients who met all inclusion criteria for our study. Average patient age at time of surgery was 38 ± 17.9 years with a male to female ratio of 1.4:1. Initial presenting symptoms included low back pain or radiculopathy (88%), urinary sphincteric disturbances (24%), lower extremity paresthesias (12%), and lower extremity weakness (12%). Average tumor size was 4.7 ± 4.4 cm and was located at the level of the conus in 22 (43%) patients, cauda equina in 28 (55%) patients and at the level of the thoracic cord in one patient (2%). The average distance from the superior portion of the tumor and the inferior tip of the conus was 1.6 ± 4.6 cm. CSF seeding was evident in 6 (12%) patients at the time of diagnosis, equally distributed between the two groups. The one patient with a tumor involving the thoracic cord had a drop metastasis at the level of S1. Of the 22 patients with lesions in contact with the conus, 18 were found to be displacing and four were invading the conus as seen on preoperative MRI and confirmed intraoperatively [
Fifty-seven tumors were surgically resected from the 51 patients in this study. En bloc resection was achieved in 32 lesions (56%), intralesional GTR in 11 lesions (19.3%), and partial resection of 14 lesions (25%). Of the 51 patients, GTR of all lesions, present at time of diagnosis, was possible in 39 (76.5%) patients. Pathologically, 46 (90.2%) tumors had classical features of MPE, 4 (7.8%) showed signs of atypia, and 1 (2%) tumor was extensively calcified. Adjuvant postoperative radiation therapy was given to six patients, all of which had partial resections. In all six patients radiation therapy was administered to the surgical bed with adequate margins, using intensity modulated radiotherapy techniques when available [
Average follow-up was 57 months with a range of 12– 165 months. Only 2 (4%) patients in our cohort developed new postoperative lower extremity weakness. A good outcome, defined by an mRs score of 0–2, was achieved in all but one patient who died after multiple systemic metastases. Eight patients developed tumor recurrence at an average of 18.1 ± 12.8 months from surgery. There were four patients with isolated local recurrence, three with concomitant spread along the craniospinal axis, and one patient with associated extra-neural metastasis. One of six patients who received postoperative radiation therapy after partial resection developed recurrence at 9 month postradiation therapy. In comparison, four recurrences, at a mean 20.8 ± 18.1 months from surgery, occurred in the remaining six patients who underwent partial resection but did not undergo postoperative radiation therapy. Of the eight patients who developed recurrence, five went on to receive local radiation therapy after first recurrence. Of these, two patients developed recurrence at 41 and 48 months postradiation therapy, two were stable at last follow-up, and one was lost to follow-up.
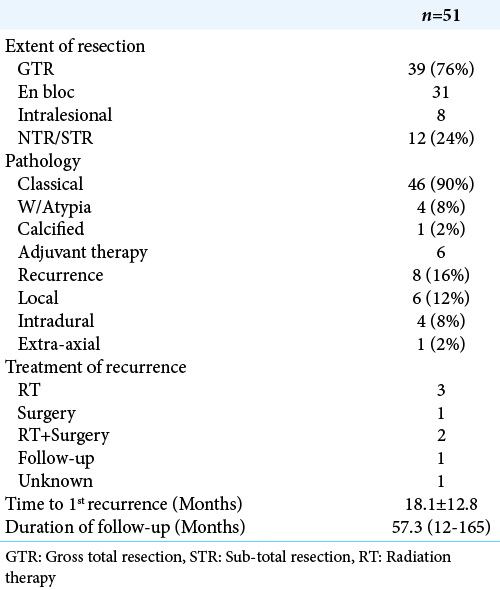
After excluding tumors with pathological features of atypia, there was a statistically significant difference in recurrence rate between en bloc GTR and intralesional GTR, P = 0.0444, with no recurrences occurring in the en bloc resection group with MPE with classic pathological features. When comparing clinical presentation and outcome of patients with MPE in contact with the conus versus those not in direct contact to the conus, there was a statistically significant difference in rate of urinary symptoms at presentation (40.9% vs. 10.7%, respectively, P = 0.0123). Preoperative urinary symptoms improved in six patients (five in the conus group and one in the nonconus group) after surgical resection. Patients with tumors contacting the conus had more than twice the incidence of postoperative long-term urinary disturbances compared to patients with MPE not contacting the conus (32% vs. 14%) but the difference did not reach statistical significance, this difference was evident even after excluding patients with urinary disturbances at baseline [
DISCUSSION
Myxopapillary ependymoma proximity to the conus medullaris is associated with higher rates of preoperative and postoperative urinary dysfunction compared to MPE that does not directly contact the conus. Invasion of the conus is an important preoperative predictor of technique and extent of resection. Patients who had an en bloc GTR were less likely to develop a recurrence than those with intralesional GTR.
There is limited literature assessing the role of anatomical location in prediction of surgical outcomes of MPE.[
While many prior studies assessing MPE outcomes have failed to distinguish en bloc GTR versus intralesional GTR, our study demonstrates the importance of maintaining tumor capsule integrity in lowering recurrence rate. We found zero recurrences in patients who underwent en bloc GTR versus 25% for patients with intralesional GTR. Similar results have been published in prior studies.[
The role of postoperative radiation therapy in patients with partially resected MPE has not been fully established in the literature. While many authors believe that adjuvant therapy is warranted to decrease the risk of cranio-spinal axis and extra-axial spread, others believe that close follow-up should suffice given the benign nature of these tumors.[
Our study is limited by its retrospective nature. Furthermore, given the rare nature of these tumors, outcomes such as recurrence were of limited numbers and thus the study is underpowered for more detailed analysis. This study was performed at a single institution, which may limit its application across other practices.
CONCLUSION
Patients with MPE in contact with the conus are more likely to suffer from urinary sphincteric disturbances both in the pre and postoperative setting. Regardless of tumor location en bloc resection is feasible and should be attempted given the lower risk of recurrence achieved. En bloc GTR is less feasible and urinary morbidity is higher when tumors invade the conus medullaris. Our data support the utility of postoperative adjuvant radiotherapy in patient who fail to attain a GTR. For tumors invading the conus, efforts to minimize morbidity, such as more conservative resection followed by adjuvant radiation therapy, are worthy of further evaluation.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdulaziz M, Mallory GW, Bydon M, De la Garza Ramos R, Ellis JA, Laack NN. Outcomes following myxopapillary ependymoma resection: The importance of capsule integrity. Neurosurg Focus. 2015. 39: E8
2. Akyurek S, Chang EL, Yu TK, Little D, Allen PK, McCutcheon I. Spinal myxopapillary ependymoma outcomes in patients treated with surgery and radiotherapy at M.D. Anderson cancer center. J Neurooncol. 2006. 80: 177-83
3. Al-Habib A, Al-Radi OO, Shannon P, Al-Ahmadi H, Petrenko Y, Fehlings MG. Myxopapillary ependymoma: Correlation of clinical and imaging features with surgical resectability in a series with long-term follow-up. Spinal Cord. 2011. 49: 1073-8
4. Bagley CA, Wilson S, Kothbauer KF, Bookland MJ, Epstein F, Jallo GI. Long term outcomes following surgical resection of myxopapillary ependymomas. Neurosurg Rev. 2009. 32: 321-34
5. Bates JE, Choi G, Milano MT. Myxopapillary ependymoma: A SEER analysis of epidemiology and outcomes. J Neurooncol. 2016. 129: 251-8
6. Feldman WB, Clark AJ, Safaee M, Ames CP, Parsa AT. Tumor control after surgery for spinal myxopapillary ependymomas: Distinct outcomes in adults versus children. J Neurosurg Spine. 2013. 19: 471-6
7. Gilbert MR, Ruda R, Soffietti R. Ependymomas in adults. Curr Neurol Neurosci Rep. 2010. 10: 240-7
8. Khalatbari MR, Jalaeikhoo H, Hamidi M, Moharamzad Y. Craniospinal dissemination of filum myxopapillary ependymoma following spinal trauma: Case report and literature review. Childs Nerv Syst. 2013. 29: 149-52
9. Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC.editors. The WHO Classification of Tumors of the Nervous System. Oxford: Oxford Academic; 2002. p.
10. Kotecha R, Tom MC, Naik M, Angelov L, Benzel EC, Reddy CA. Analyzing the role of adjuvant or salvage radiotherapy for spinal myxopapillary ependymomas. J Neurosurg Spine. 2020. 2020: 1-6
11. Kukreja S, Ambekar S, Sharma M, Sin AH, Nanda A. Outcome predictors in the management of spinal myxopapillary ependymoma: An integrative survival analysis. World Neurosurg. 2015. 83: 852-9
12. Kusters JM, Louwe RJ, Van Kollenburg PG, Kunze-Busch MC, Gidding CE, Van Lindert EJ. Optimal normal tissue sparing in craniospinal axis irradiation using IMRT with daily intrafractionally modulated junction(s). Int J Radiat Oncol Biol Phys. 2011. 81: 1405-14
13. Montero AS, Tran S, Amelot A, Berriat F, Lot G, Gaillard S. Clinical characteristics and long-term surgical outcome of spinal myxopapillary ependymoma: A French cohort of 101 patients. J Neurooncol. 2021. 152: 491-9
14. Nakamura M, Ishii K, Watanabe K, Tsuji T, Matsumoto M, Toyama Y. Long-term surgical outcomes for myxopapillary ependymomas of the Cauda equina. Spine (Phila Pa 1976). 2009. 34: E756-60
15. Pica A, Miller R, VillÀ S, Kadish SP, Anacak Y, Abusaris H. The results of surgery, with or without radiotherapy, for primary spinal myxopapillary ependymoma: A retrospective study from the rare cancer network. Int J Radiat Oncol Biol Phys. 2009. 74: 1114-20
16. Wang H, Zhang S, Rehman SK, Zhang Z, Li W, Makki MS. Clinicopathological features of myxopapillary ependymoma. J Clin Neurosci. 2014. 21: 569-73
17. Woesler B, Moskopp D, Kuchelmeister K, Schul C, Wassmann H. Intracranial metastasis of a spinal myxopapillary ependymoma. A case report. Neurosurg Rev. 1998. 21: 62-5