- Department of Neurosurgical, Spine Unit, Hospital Italiano de Buenos Aires,
- Department of Orthopedic, Oncology Unit, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina,
- Department of Orthopedic, Spine Surgery Division, Instituto do Câncer do Estado de São Paulo, Sao Paulo, Brazil,
- Department of Health Informatics, Virtual Planning and Navigation Unit, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina.
Correspondence Address:
Federico Landriel, Department of Neurosurgical, Spine Unit, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina.
DOI:10.25259/SNI_1232_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Federico Landriel1, José Ignacio Albergo2, Germán Farfalli2, Claudio Yampolsky1, Miguel Ayerza2, Luis Aponte-Tinao2, William Teixeira3, Lucas Ritacco4, Santiago Hem1. Navigated multiplanar osteotomies for spinal primary bone tumors. 18-Feb-2022;13:58
How to cite this URL: Federico Landriel1, José Ignacio Albergo2, Germán Farfalli2, Claudio Yampolsky1, Miguel Ayerza2, Luis Aponte-Tinao2, William Teixeira3, Lucas Ritacco4, Santiago Hem1. Navigated multiplanar osteotomies for spinal primary bone tumors. 18-Feb-2022;13:58. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11401
Abstract
Background: Establishing the proper diagnosis and rendering appropriate treatment of spinal primary bone tumors (SPBT) can result in definitive cures. Notably, malignant, or benign SPBT (i.e., with aggressive local behavior) generally require en bloc resection. Osteotomies of the vertebral body in more than 1 plane may avoid critical structures, preserve nerve functions, and reduce the volume of healthy bone resected. Here, our objective was to report how we planned and performed navigated multiplanar osteotomies for en bloc resection of 14 SPBT.
Methods: We performed a retrospective analysis of 14 patients with malignant or locally aggressive benign SPBT operated on consecutively between 2014 and 2019 utilizing preoperative 3D planning/navigation. Tumors were resected in an en bloc fashion utilizing multiplanar osteotomies. Patients were followed for a minimum of 12 postoperative months.
Results: Diagnoses included three benign but locally aggressive bone tumors (i.e., all osteoblastomas) and 11 primary sarcomas (i.e., six chordomas and five chondrosarcomas). Eleven tumors involved the sacrum and the other three, the thoracic spine. In 12 patients, the en bloc margins were classified as marginal (1 cm). Intraoperative navigation facilitated the performance of 40 osteotomies in 14 patients (median = 2.9, range = 2–6).
Conclusion: Navigated multiplanar osteotomies increased the precision and safety of en bloc resections for 14 primary spinal bone tumors SPBT that included 11 malignant and three benign/locally aggressive lesions.
Keywords: En bloc resection, Multiplanar osteotomies, Navigated osteotomies, Spinal primary bone tumors, Spine navigation
INTRODUCTION
Malignant or benign spinal primary bone tumors (SPBTs) with aggressive local behavior generally require en bloc resection. This entails removing the entire, intact tumor surrounded by a margin of healthy tissue. The challenge is to preserve as much surrounding normal tissue/ structures as possible and avoid damaging contiguous spinal cord/nerves, and other vital structures.[
MATERIALS AND METHODS
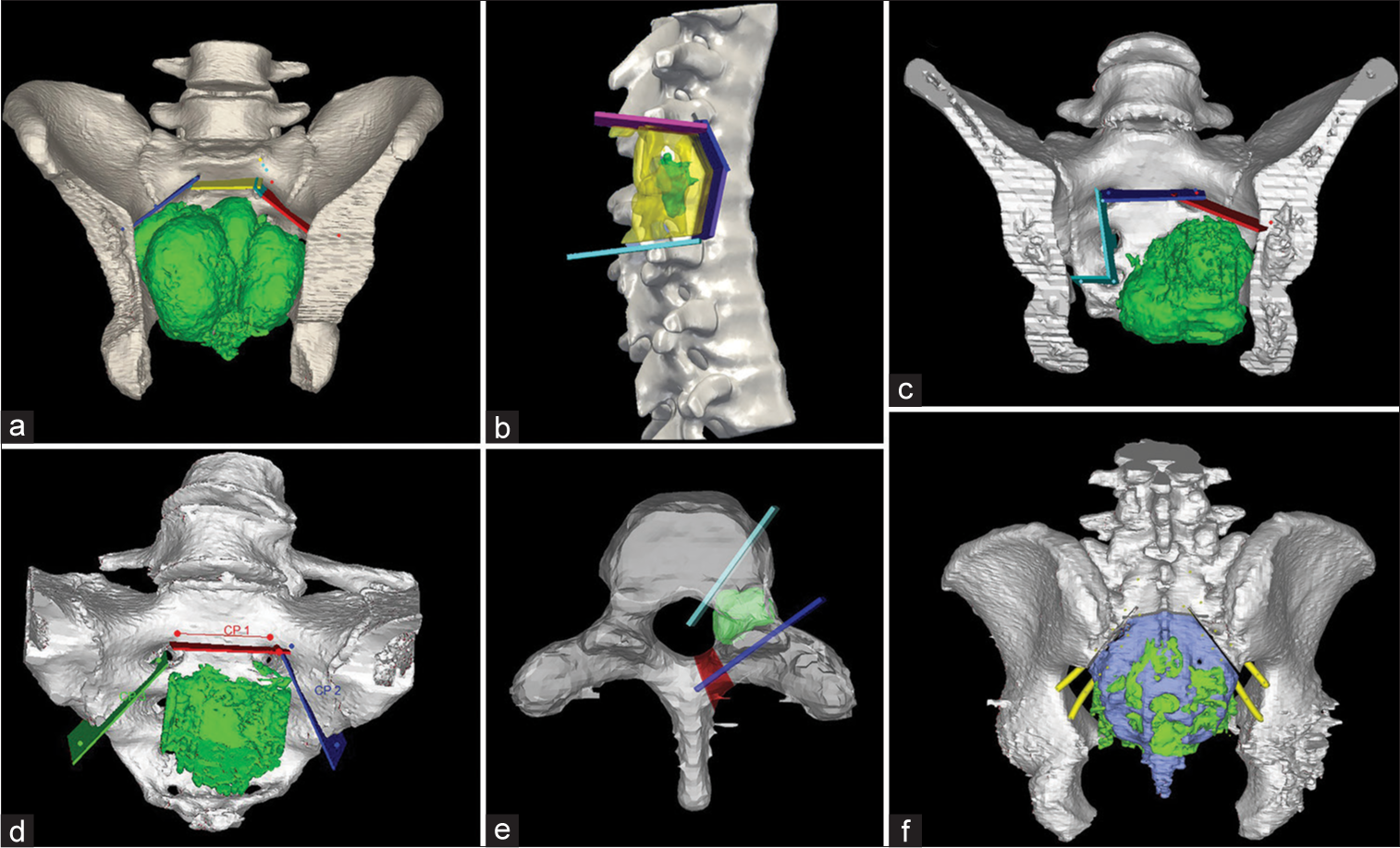
This was a retrospective analysis of 14 patients with SPBT; there were 11 malignant tumors (i.e., six chordomas and five chondrosarcomas) and three locally aggressive benign SPBT (i.e., osteoblastomas). These patients were operated on consecutively at a single center between 2014 and 2019. Eleven tumors (78.5%) were in the sacrum, while the three remaining were in the thoracic spine. The eight males and six females averaged 41.4 years of age [
Surgery
In all cases, a preoperative biopsy was performed under CT guidance, pathologists confirmed the histological diagnoses in all cases. All 14 tumor en bloc resections (i.e., employing 40 planned osteotomies’) used the same navigation system. Registration used at least four reference points from the exposed bone surface and were then refined using at least 30 additional surface registration points. For at least 12 postoperative months, we evaluated; resection margins, the frequency of local tumor recurrence, and complications.
RESULTS
Forty en bloc resections in 14 patients were accompanied by osteotomies utilizing preoperative 3D planning and navigation [
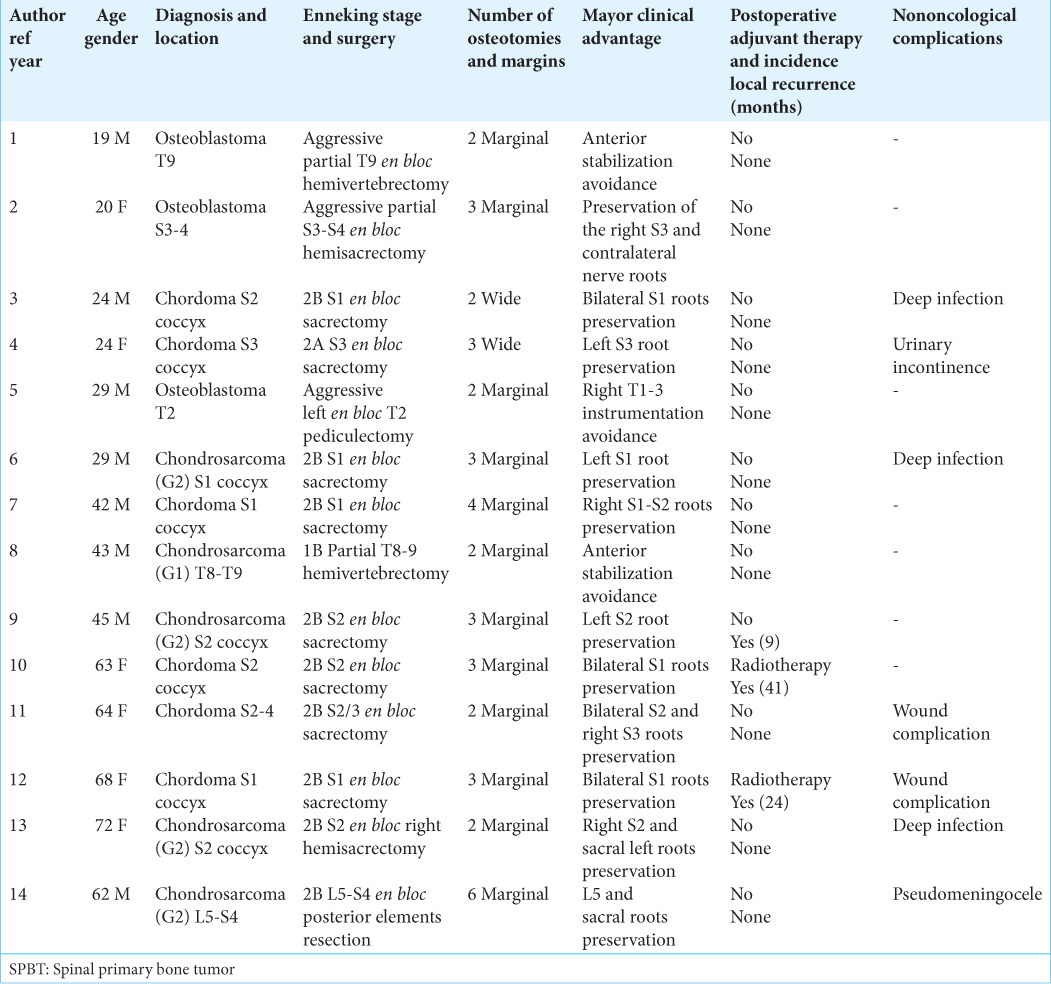
Figure 1:
(a-c) Sagittal, coronal, and axial computed tomography (CT) of the left-sided T9 vertebral body osteoblastoma. (d) T2-WI magnetic resonance imaging of tumor’s proximity to aorta, lung, and cord. (e) Preoperative multiplanar osteotomy planning. Red cut – first-step transthoracic approach; blue cut – second-step posterior approach to release the tumor en bloc. (f-h) Postoperative CT images demonstrate complete tumor resection. Images i and j show surgical sample of tumor in the left posterolateral T8 vertebral body surrounded by the T7 and T8 rib heads and soft tissue.
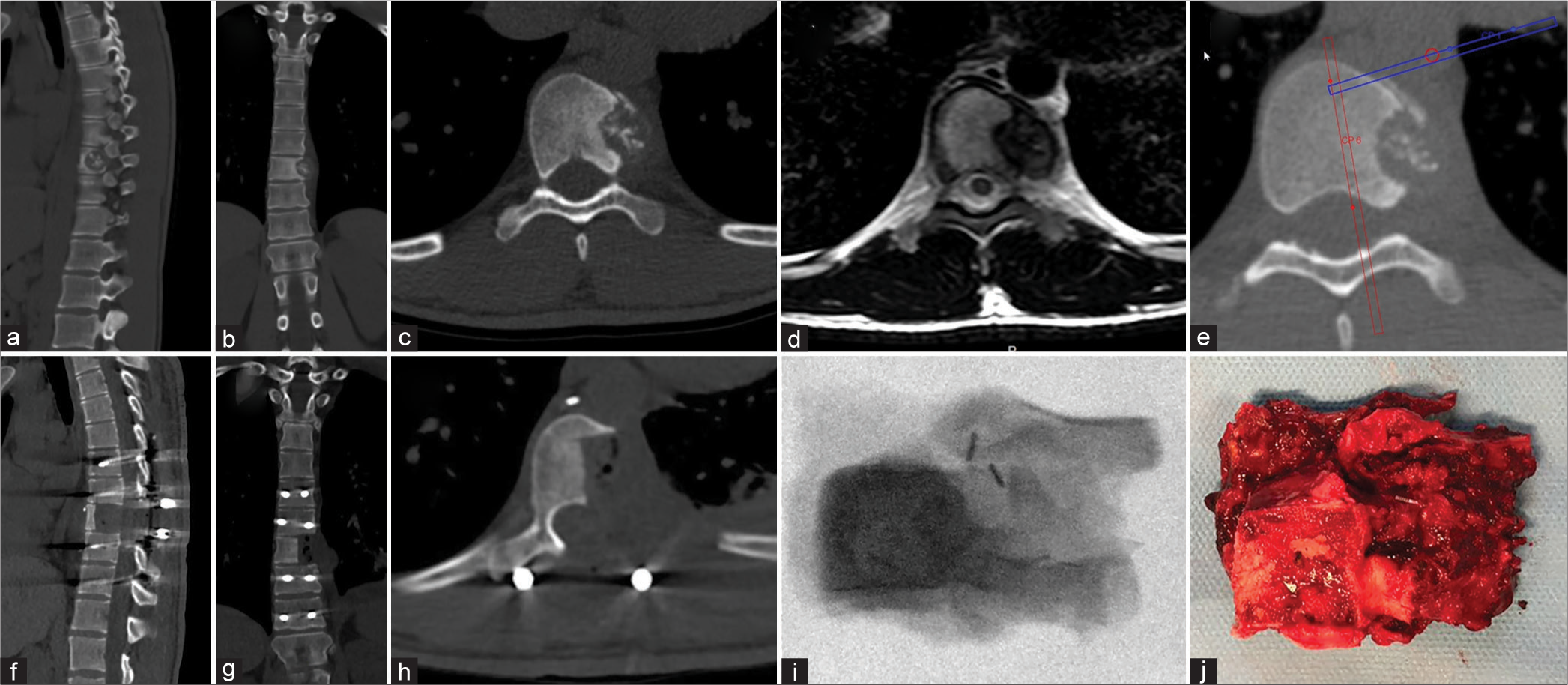
Figure 2:
(a) T2-WI coronal magnetic resonance imaging showing right-sided osteoblastoma and relationship to 4th right sacral foramen. (b and c) Sagittal and coronal computed tomography (CT) images of spinal primary bone tumors. (d) Planned preoperative multiplanar osteotomies through the blue, yellow and red lines, the green area is the tumor reconstruction. (e) Intraoperative navigation/registration. (f) Intraoperative image of the medial osteotomy/correlation with the navigated tracker. (g) En bloc resection of tumor. (h) Postoperative CT total tumor excision with structural graft.
DISCUSSION
Several authors have reported the advantages of using navigation during uniplanar osteotomies for en bloc resections of SPBT with different imaging and cutting technologies.[
The availability of computer-assisted surgery since 2010 has facilitated 3D planning of en bloc resections of primary bone tumors, particularly in performing accurate osteotomies with safe margins preserving healthy tissues [
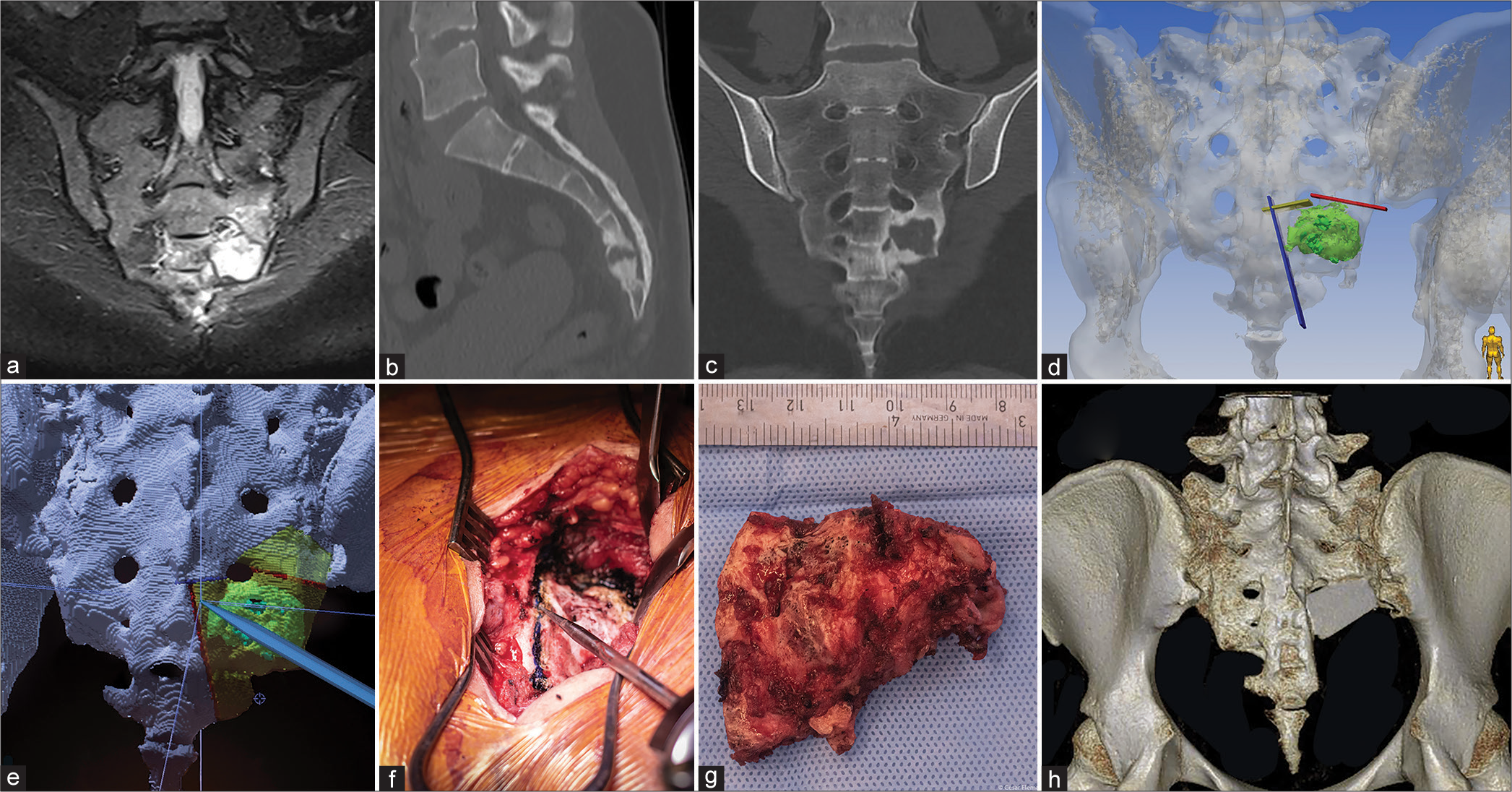
Figure 3:
Navigated multiplanar osteotomies for en bloc resection of spinal primary bone tumors. (a) Preoperative planning of patient 6, an S1 coccyx chondrosarcoma (G2), 3 cuts (blue, yellow, and red lines) were made. (b) Patient 8, a T8-T9 chondrosarcoma (G1), 4 cuts (pink, blue, purple, and light-blue) were made the yellow part represents the partial osteotomy area. (c) Patient 7, S1 coccyx chordoma, 4 cuts were planned (cyan, light-blue, blue, and red lines). (d) Patient 12, an S1 coccyx chordoma, 3 line-cuts were done (green, red, and blue). (e) Correspond to patient 5, a T2 osteoblastoma, 2 osteotomies were done (light-blue and blue lines), the purple area represent the ipsilateral hemi-laminectomy. (f) Patient 10, an S2 coccyx chordoma were 3 osteotomies were planned.
CONCLUSION
Navigated multiplanar osteotomies increased the precision and safety of en bloc resections for 14 primary spinal bone tumors SPBT that included 11 malignant and three benign/locally aggressive lesions.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Docquier PL, Paul L, Cartiaux O, Delloye C, Banse X. Computer-assisted resection and reconstruction of pelvic tumor sarcoma. Sarcoma. 2010. 2010: 125162
2. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980. 153: 106-20
3. Hsu W, Kosztowski TA, Zaidi HA, Dorsi M, Gokaslan ZL, Wolinsky JP. Multidisciplinary management of primary tumors of the vertebral column. Curr Treat Options Oncol. 2009. 10: 107-25
4. Kobayashi K, Imagama S, Ito Z, Ando K, Yokoi K, Ishiguro N. Utility of a computed tomography-based navigation system (O-Arm) for en bloc partial vertebrectomy for lung cancer adjacent to the thoracic spine: Technical case report. Asian Spine J. 2016. 10: 360-5
5. Mavrogenis AF, Savvidou OD, Mimidis G, Papanastasiou J, Koulalis D, Demertzis N. Computer-assisted navigation in orthopedic surgery. Orthopedics. 2013. 36: 631-42
6. Nasser R, Drazin D, Nakhla J, Al-Khouja L, Brien E, Baron EM. Resection of spinal column tumors utilizing image-guided navigation: A multicenter analysis. Neurosurg Focus. 2016. 41: E15
7. Ng S, Boetto J, Poulen G, Berthet JP, Marty-Ane C, Lonjon N. Partial vertebrectomies without instrumented stabilization during en bloc resection of primary bronchogenic carcinomas invading the spine: Feasibility study and results on spine balance. World Neurosurg. 2019. 122: e1542-50
8. Ritacco LE, Milano FE, Farfalli GL, Ayerza MA, Muscolo DL, Aponte-Tinao LA. Accuracy of 3-D planning and navigation in bone tumor resection. Orthopedics. 2013. 36: e942-50
9. Ritacco LE, Milano FE, Farfalli GL, Ayerza MA, Muscolo DL, de Quirós FG. Bone tumor resection: Analysis about 3D preoperative planning and navigation method using a virtual specimen. Stud Health Technol Inform. 2013. 192: 1162
10. Wong KC, Kumta SM, Antonio GE, Tse LF. Image fusion for computer-assisted bone tumor surgery. Clin Orthop Relat Res. 2008. 466: 2533-41