- Department of Neurological Surgery, Center for Nerve Injury and Paralysis, Washington University School of Medicine, St. Louis, MO 63110, USA
Correspondence Address:
Justin M. Brown
Department of Neurological Surgery, Center for Nerve Injury and Paralysis, Washington University School of Medicine, St. Louis, MO 63110, USA
DOI:10.4103/2152-7806.84392
Copyright: © 2011 Brown JM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Justin M. Brown. Nerve transfers in tetraplegia I: Background and technique. 30-Aug-2011;2:121
How to cite this URL: Justin M. Brown. Nerve transfers in tetraplegia I: Background and technique. 30-Aug-2011;2:121. Available from: http://surgicalneurologyint.com/surgicalint-articles/nerve-transfers-in-tetraplegia-i-background-and-technique/
Abstract
Background:The recovery of hand function is consistently rated as the highest priority for persons with tetraplegia. Recovering even partial arm and hand function can have an enormous impact on independence and quality of life of an individual. Currently, tendon transfers are the accepted modality for improving hand function. In this procedure, the distal end of a functional muscle is cut and reattached at the insertion site of a nonfunctional muscle. The tendon transfer sacrifices the function at a lesser location to provide function at a more important location. Nerve transfers are conceptually similar to tendon transfers and involve cutting and connecting a healthy but less critical nerve to a more important but paralyzed nerve to restore its function.
Methods:We present a case of a 28-year-old patient with a C5-level ASIA B (international classification level 1) injury who underwent nerve transfers to restore arm and hand function. Intact peripheral innervation was confirmed in the paralyzed muscle groups corresponding to finger flexors and extensors, wrist flexors and extensors, and triceps bilaterally. Volitional control and good strength were present in the biceps and brachialis muscles, the deltoid, and the trapezius. The patient underwent nerve transfers to restore finger flexion and extension, wrist flexion and extension, and elbow extension. Intraoperative motor-evoked potentials and direct nerve stimulation were used to identify donor and recipient nerve branches.
Results:The patient tolerated the procedure well, with a preserved function in both elbow flexion and shoulder abduction.
Conclusions:Nerve transfers are a technically feasible means of restoring the upper extremity function in tetraplegia in cases that may not be amenable to tendon transfers.
Keywords: Nerve transfer, reconstructive neurosurgery, surgical rehabilitation, tetraplegia
INTRODUCTION
Within the United States, there are approximately 225,000–300,000 persons with a spinal cord injury (SCI), with approximately 12,000 individuals suffering a new SCI each year.[
Currently, tendon transfers are the most commonly accepted intervention for restoring hand function in persons with tetraplegia. The distal end of a functional muscle is cut and reattached at the insertion site of a nonfunctional muscle. The new configuration produces a new function. The tendon transfer sacrifices function at a lesser location for function at a more important location. While these procedures offer functional gains for an estimated 70% of tetraplegic patients, recent surveys estimated that fewer than 10% of appropriate candidates actually received the interventions.[
Nerve transfers are conceptually quite similar to tendon transfers. Simply put, a nerve serving one function (and originating above the injury zone) is cut and reconnected to a nonfunctional nerve (below injury zone) serving a more important function. Thus, a patient who has effective elbow flexion but no finger flexion may have finger flexion restored by transferring some of the nerve branches that provide elbow flexion to the nerve that provides finger flexion. A number of nerve transfers have been developed for restoring function within the hand.[
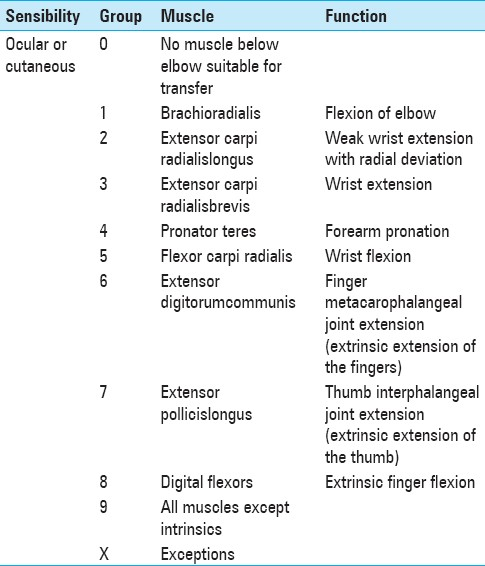
In contrast to tendon transfers, nerve transfers require a significant amount of time postoperatively before function is realized. This time is needed for the regeneration of transferred axons from the site of suture repair to their new target muscle. Nerve transfers, though, have a number of attributes that may make them more appealing than tendon transfers in some situations. First, they restore muscle groups without altering their biomechanics. Second, they do not require prolonged immobilization. Third, they offer potential reconstructions when no tendon transfer options are available, as in International Classification for Surgery of the Hand in Tetraplegia group 0 (ICSHT 0) [
MATERIALS AND METHODS
Case Report
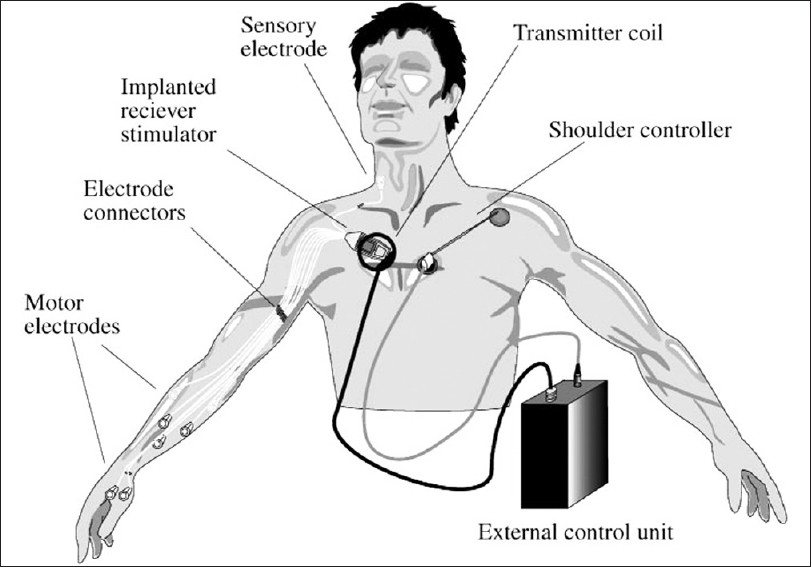
This 28-year-old, left-handed man was injured in a football accident 13 years before presentation, leaving him a C5 ASIA B tetraplegic. The patient remained motivated and an active participant in therapy. Nine years before presentation he underwent successful placement of a functional electrical stimulation (FES) system (Freehand System©, NeuroControl Corporation), which allowed him to artificially produce pinch and grip via a control driven by the contralateral shoulder [
The patient underwent detailed functional evaluation. On motor examination, he had full 5/5 Medical Research Council (MRC) strength in his upper trapezius and anterior and medial deltoids bilaterally. The MRC strength in his biceps/brachialis muscles, middle, and lower trapezius, and upper portions of his serratus anterior bilaterally was 4–4+/5. His posterior deltoid strength was 4+/5 on the right but 3+/5 on the left. Wrist extension was recorded as 3/5 on the right and 2+/5 on the left (although this movement was the result of a previous brachioradialis to extensor carpi radialis brevis tendon transfer performed at the time of the FES implant). No appreciable volitional function (0/5) was identified in the triceps, wrist and finger flexors, or interosseous muscles bilaterally. Given this complete paralysis of the hands, pinch and grip measurements were not feasible, but were followed as regeneration progresses.
Figure 1
The Freehand system is an implanted system with stimulation electrodes in key muscles of the arm and hand (in right arm). The coordinated activation of these electrodes provided for pinch and grasp within the otherwise paralyzed hand. The selection of output is provided by the contralateral shoulder controller (left shoulder; From Hobby J, Taylor PN, Esnouf J. Restoration of tetraplegic hand function by use of the NeuroControl Freehand System. J Hand Surg 2001; 26(5): 450-464)
Sensory testing revealed a visual analog scale rating of 8/10 in the right median distribution and 10/10 in the right ulnar, while 8/10 was described in both left median and ulnar distributions. Two-point discrimination was detectable at 6–7 mm in the right median, 6–8 mm in the right ulnar, 7–8 mm in the left median, and 6–9 mm in the left ulnar distributions, with the first number indicating the detection of a moving stroke across the finger and the second static pressure of the two probes.
He was also subjected to a battery of functional tests. On the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire, he scored a 72.5, with a 50.0 in the Work subcategory and an 87.5 in the Sports subcategory (where 0 = no disability and 100 = severe disability). On the Canadian Occupational Performance Measure, he scored a 3.8 in both performance and satisfaction, of a possible 10 points in each category. On the Action Research Arm Test, he scored 3/57 on the left and 6/57 on the right. The total time on the Jebsen-Taylor Hand Test was 324.3 s on the right and 515.34 s on the left, indicating severe dysfunction bilaterally (mean for age-matched controls being 37.65, with a standard deviation of 8.45). These measures provide a qualitative means of assessing either positive changes in the function that may result from an improved function within the intended target muscles or negative changes in the function which could result from ineffective reinnervation or weakening of donor muscles.
Electrodiagnostic studies demonstrated essentially normal median compound motor action potential (CMAP) amplitudes and velocity, with slightly prolonged ulnar latency on the left. Radial CMAPs demonstrated normal velocities, with slightly small amplitude from the extensor indicis proprius. Needle examination demonstrated no abnormal spontaneous activity in the left extensor digitorum communis, extensor carpi radialis longus, brachioradialis, extensor indicis proprius, biceps, brachialis, deltoid, triceps, pectoralis, and trapezius. Normal recruitment was noted in the trapezius, moderately reduced recruitment was noted in the brachialis, and severely reduced recruitment was noted in the brachioradialis and posterior deltoid. As would be expected, no motor unit potentials were detectible on needle EMG examination of the paralyzed muscles outside of passively triggered spasms. Conversely, all muscle groups were directly activated by the stimulation of the associated nerve, as would be expected in a patient who had benefitted from the implantation of an upper extremity FES system. This again confirms, that the paralysis is due to the spinal cord injury and has minimal to no contribution from peripheral axon loss.
Operative and reconstructive techniques
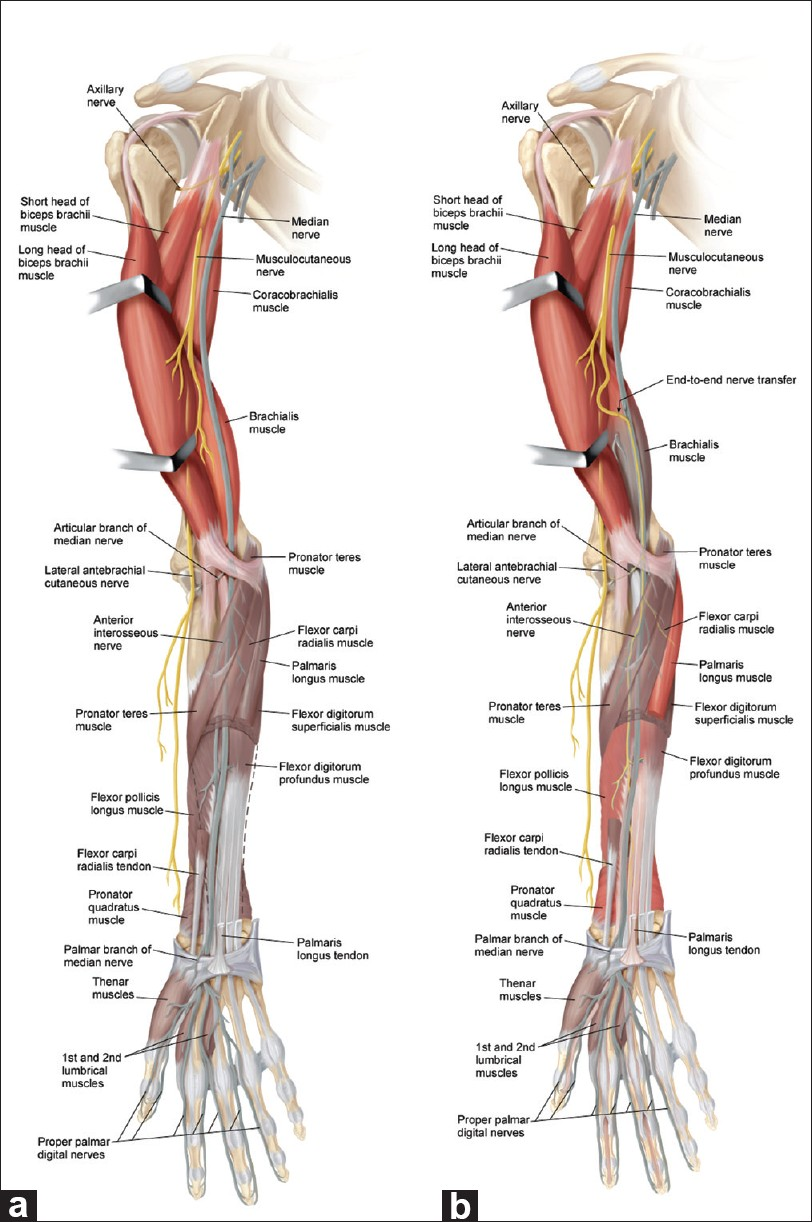
The basic goal of this procedure is to redistribute redundant cortically controlled nerves to activate paralyzed muscle groups which are critical to reaching and grasping. Following the removal of the previously placed FES system, the first objective of this operation was to redistribute control from the elbow flexors into the wrist and finger flexors to allow pinch and grasp [
Figure 2
The musculocutaneous to median nerve transfer strategy. (a) This patient's injury has left him with shoulder and biceps function (muscle is red, indicating a normal function) and little else (other muscles are gray, indicating lack of function). Based upon our examination and electrodiagnostic studies, he has retained excellent function within all of the musculocutaneous distribution, but no function in the median-innervated finger or wrist flexors. (b) Given the redundancy in present elbow flexors, we would plan to sacrifice much of the brachialis muscle distribution (now gray distally) in order to recover function within specific key wrist and finger flexors (palmaris longus for wrist and flexor pollicis longus and flexor digitorum profundus for fingers are now red indicating new function). By directing fibers into the posterior fascicle of the median nerve, which includes the anterior interosseous fibers and the fascicle to the palmaris longus, the pronator quadratus is likely to be reinnervated as well (red), providing additional pronation
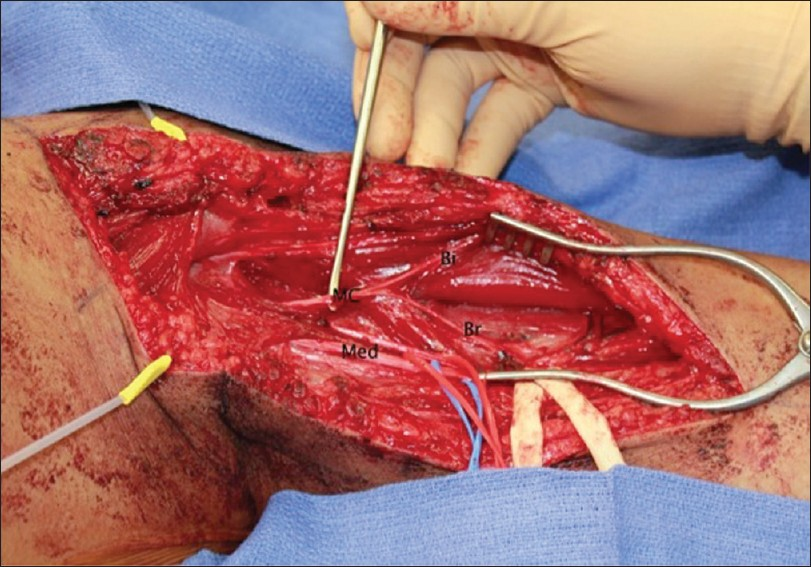
The patient was placed in the supine position, with his arm on an arm board [
Figure 3
The patient is positioned supine with the arm on an armboard. General endotracheal anesthesia is administered. Prior incisions from the implantation of the functional electrical stimulation system are marked as well as additional incisions required for the nerve transfer procedure. A tourniquet is not used in this case to avoid the potential for ischemic neurapraxia
We then explored the medial arm in preparation for the musculocutaneous to median nerve transfer to restore wrist and finger flexion. The musculocutaneous nerve was identified between the biceps and brachialis muscles, bifurcating at the midarm to send a branch to each of these muscles [
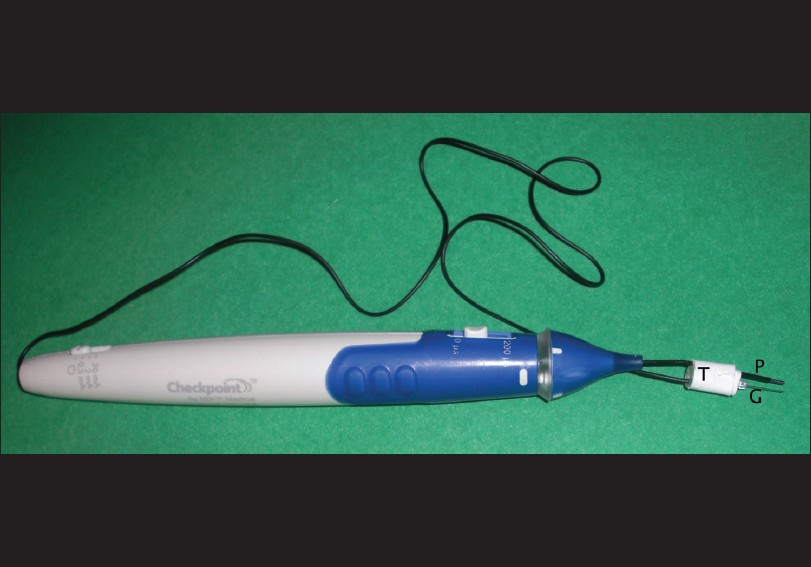
Next, a biphasic nerve/muscle stimulator with a range of stimulation control (Checkpoint® Stimulator/Locator, Cleveland, OH, USA,) was used in order to facilitate the identification of nerves and individual nerve fascicles without fatiguing or injuring the nerve. The identity of the donor nerve, the musculocutaneous, and its component branches to the biceps and brachialis was confirmed with direct stimulation. Of note, in a situation in which paralysis is secondary to an upper motor neuron (UMN) injury, “paralyzed” nerves will respond to direct stimulation just as normal nerves do. Therefore, transcranial stimulation was then used to confirm effective cortical activation of both biceps and brachialis muscles [
Figure 5
To avoid current spread and activate the specific fascicle of interest, bipolar stimulation is preferred. The ground needle (G) is placed parallel to the probe (P) and tape (T) is applied, positioning the needle tip within 1 mm of the probe tip. The tips should be even so that both will contact the nerve segment simultaneously
The now exposed and separated fascicles of the median nerve were directly stimulated in turn until one was identified that provided dominant contribution to wrist and finger flexion of digits 1–3 [
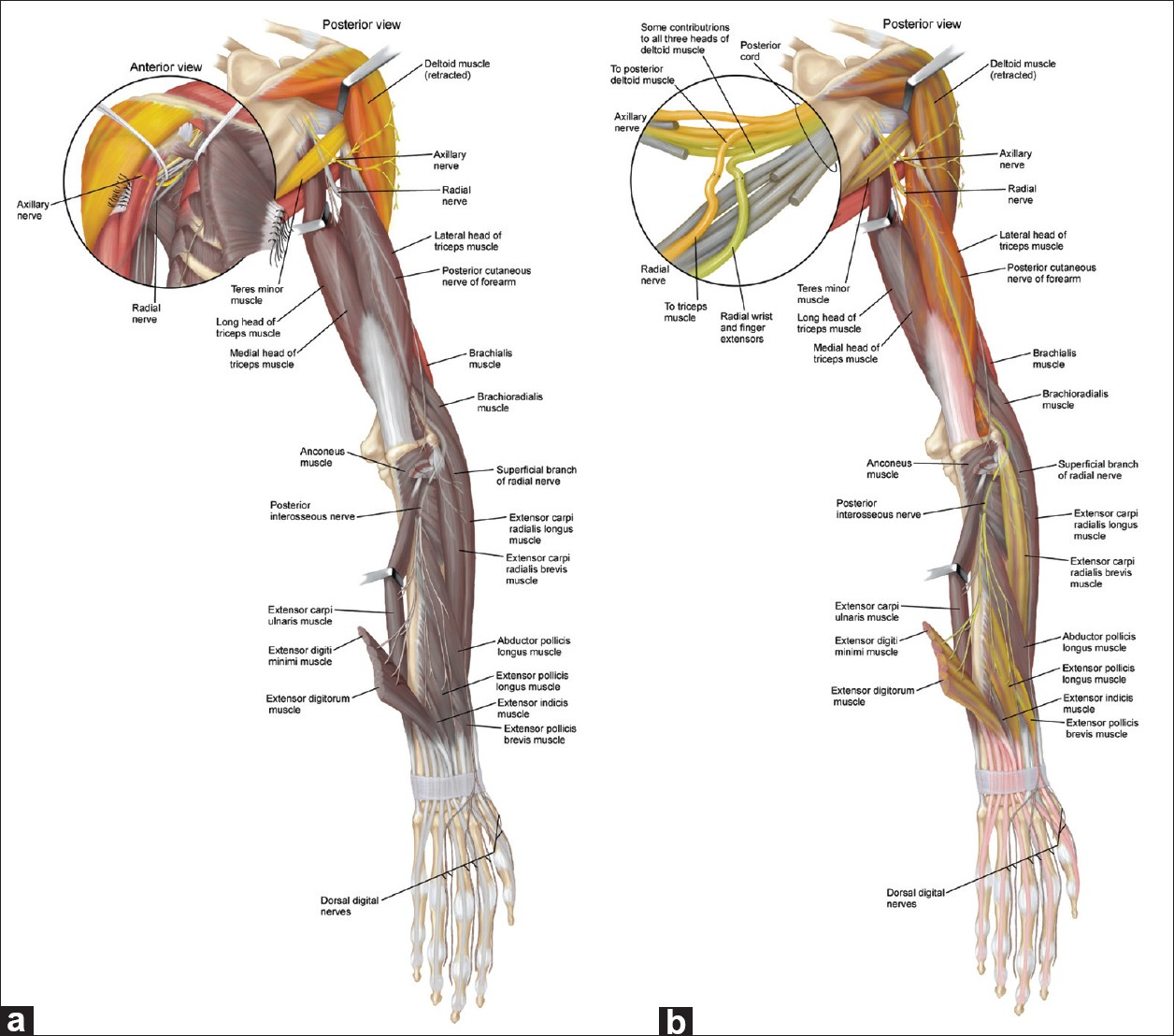
The next objective of our operation was to redistribute function from the shoulder musculature to the arm, forearm, and finger extensors to provide both reach and release [
Figure 6
The axillary to radial nerve transfer strategy. (a) Given this patient's superb shoulder function (colored muscle) but complete lack of radial nerve function (gray muscle), a subset of his axillary nerve fascicles was redistributed to the neighboring radial nerve. Specific subfascicles of the radial nerve were selected as recipients to achieve extension at the elbow, extension at the wrist, and extension at the fingers. (b) These are driven by separate portions of the axillary nerve so that the patient can conceptualize the movements to be coupled, thereby allowing specific pairing of shoulder extension with elbow extension and shoulder abduction with wrist and finger extension. To accomplish this, an axillary fascicle with predominant contribution to the posterior deltoid (yellow/orange fascicle in inset) was transferred to radial fascicles to the triceps (a subset of triceps now taking on that color, indicating its target). Additionally, axillary fascicles to the middle and anterior deltoid (green fascicle in inset) were redirected to wrist and finger extensors (taking on that color, indicating the target of that fascicle). Innervation to the deltoid is reduced as a result of these transfers (indicated by the patchy gray now present), but should recover in a few months, with motor unit enlargement
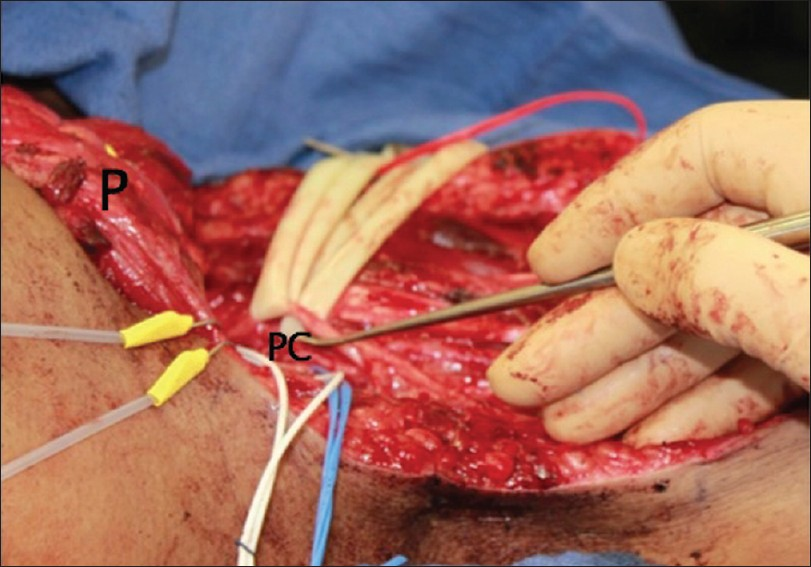
Figure 7
View from the axilla. The pectoralis muscle (P) is cut from its humeral insertion and retracted medially to expose the distal brachial plexus. At this level, the posterior cord has recently bifurcated into the axillary and radial nerves. The other elements of the brachial plexus are looped in ¼-inch Penrose drains and retracted to expose these nerves (also depicted in the inset in Figure 6a). The nerves are stimulated to confirm their identity and then intraneural dissection is undertaken to find the appropriate donor and recipient fascicles
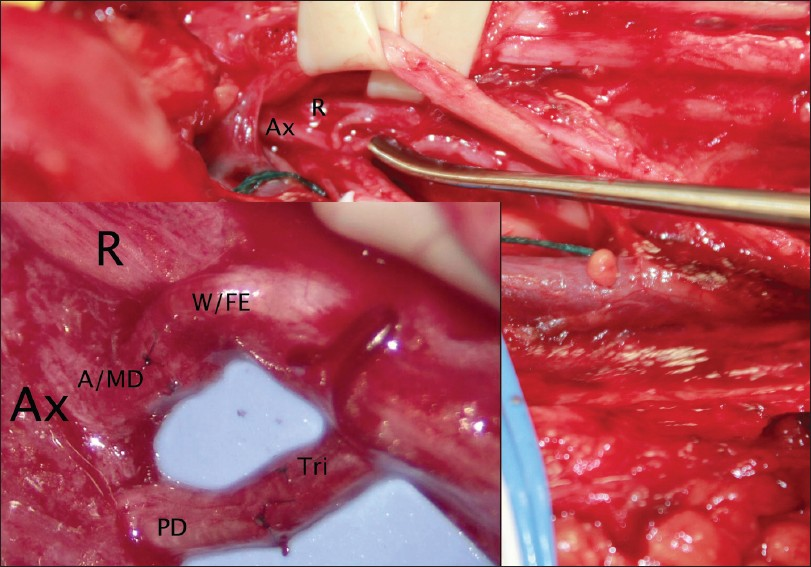
The axillary and radial nerves were directly stimulated to confirm their identity. At this point an EMG lead was placed in each of the anterior, middle, and posterior heads of the deltoid and transcranial stimulation was repeated, confirming active cortical control of all three heads of the deltoid. Then, similar to the median nerve dissection described above, the axillary nerve was explored and separated into five primary fascicles, which were stimulated as described above. Three of these fascicles were found to be contributing to global contraction of the deltoid, and the last two, smaller ones contributed primarily to the posterior deltoid. The radial nerve was dissected in a similar fashion, and a strong fascicle contributing to wrist and finger extension was identified, as well as one to the triceps [
Figure 8
Same view as in Figure 7, with fascicular repairs complete. Again, the brachial plexus, excluding the axillary and radial nerves, is looped and retracted. Donor fascicles have been cut from the axillary nerve, one corresponding to anterior and middle deltoid innervations and the other to posterior deltoid. These have been sutured to recipient fascicles of the radial nerve, one corresponding to wrist and finger extension and the other corresponding to elbow extension via triceps function). These have been coapted with three circumferential 9-0 nylon sutures
Postoperatively, the patient experienced pain primarily at the site of the pectoralis repair. He retained strong volitional activation of the deltoid and biceps, though a change in strength could not be adequately assessed given the temporary, imposed range of motion restriction. Pain was well controlled with oral medications, and the patient was discharged on postoperative day 2.
RESULTS
Feasibility of the technique
The dissections undertaken in this procedure closely resemble those encountered in brachial plexus repair with one added advantage: because neural tissue was healthy, the “dysfunctional” nerve could be stimulated so that specific targets quite distal to the site of dissection could be selected. As a result of this proximal dissection and repair, the nerve components were even smaller than those generally encountered with nerve transfer operations, making these repairs slightly more technically challenging. Otherwise, the skills required to perform this procedure are within the skill set of any experienced peripheral nerve surgeon.
Electrostimulation was critical to this case. Transcranial stimulation is available to most intraoperative electrodiagnostic teams. Unfortunately, visually negative stimulation can at times be interpreted as “positive” by the diagnostic team; therefore, detailed preoperative evaluation and electrodiagnostic studies are also essential. The direct stimulation of the recipient nerve ensures the presence of functional axons, making a nerve transfer in the chronic phase of the SCI feasible. A peripheral nerve or lower motor neuron (LMN) injury of this chronicity would be unlikely to accept axons in any useful manner.
Postoperative results
The pain resulting from this procedure was relatively minor. Most of the discomfort resulted from the pectoralis takedown. This pain began to abate within a few days of the procedure. Additionally, some paresthesias were noted; these lasted only a few weeks. The shoulder immobilizer was kept in place for 1 week to limit shoulder abduction and protect the pectoralis tendon repair. Otherwise, the patient was permitted to use the arm as he had previously done. Had the pectoralis been functional, a longer period of immobilization might have been required. Early follow-up took place 12 weeks after surgery. At this time, the patient reported no decrement in the motor strength in either elbow flexion or deltoid function. On manual motor testing, he was graded as 5/5 in elbow flexion and shoulder flexion and abduction. He was able to abduct the shoulder easily with a 10-lb weight hung at the elbow, just as he did preoperatively. In elbow flexion, however, he was able to curl only the 10-lb weight, whereas preoperatively he did this with 20 lb. This communication is limited to the details of this procedure and its safety, including short-term follow-up. Part II will address the ultimate functional consequences. The tetanic stimulation of the recipient nerve fascicles during surgery gives an indication of the potential ultimate recovery, but a number of factors will determine the ultimate success. It should be noted that the nerve transfers undertaken are performed at a significant distance from the target muscles. As a result, substantial time elapses prior to functional axons reaching the target muscles. At the typical rate of 1 mm per day, we would expect the first signs of reinnervation to emerge at 9–12 months and plateau by 2 years from the time of surgery. The time course of recovery will be carefully detailed in the second part of this communication.
DISCUSSION
Traumatic cervical SCI results in three distinct regions of spinal cord: the supralesional segment, the injured metamere, and the infralesional segment [
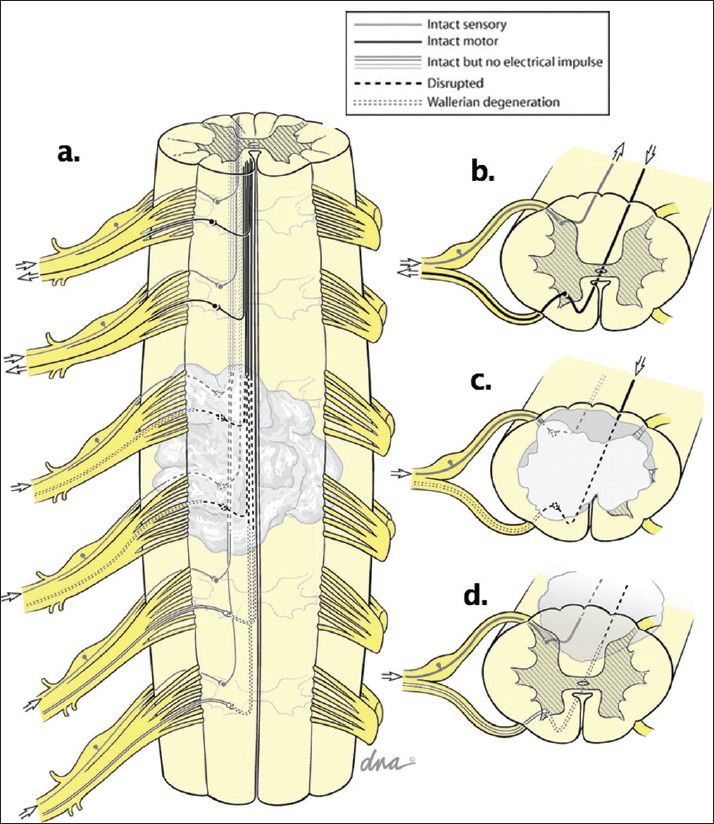
Figure 9
(a) traumatic spinal cord injury results in an indiscriminate disruption of the white and gray matter at and adjacent to the site of trauma, producing three regions of the CNS: (b) the supralesional segment, which retains normal control of its associated peripheral nerves; (c) the injured metamere, which is the site of the cord suffering actual tissue disruption; and (d) the infralesional segment, which often retains anatomical integrity but suffers from a loss of descending input from above. Recognizing which of these three conditions affects the particular muscles of interest allows one to develop an effective reconstructive neurosurgical intervention
The LMN injuries at the injured metamere segment must be adequately assessed. A substantial LMN injury would have precluded this patient from being a candidate for this procedure. In our experience, some patients may have several muscle groups with no detectable innervation, and others have signs of partial LMN injury scattered across many muscle groups, as in the patient discussed here.[
A nerve transfer procedure may restore a muscle group of the infralesional segment (affected by UMN injury) even years after an injury, as long as the mechanical properties of the limb remain intact as a result of good therapy hygiene, including regular range of motion exercises.[
Both nerve and tendon transfer procedures are used to address instances of paralysis of the arms and hands following a nervous system injury by bringing cortically controlled supralesional nerves or muscles into a position to control lesional or infralesional muscle groups.[
Most daily living activities are performed through lateral thumb pinch (key-pinch), grasp, and release. The restoration of these basic functions, combined with the re-establishment of elbow extension, increases independence, spontaneity, and function, as shown on a variety of outcome measures. Tendon transfers have been a useful method of accomplishing this goal. Unfortunately, there are impediments to an ideal result following such interventions. Muscle groups affected by LMN damage fibrose over time and lead to joint contractures. These contractures may develop late after discharge from rehabilitation and interfere with the function of the reconstructed hand. If surgery is not performed early, hand contractures may interfere with the ability to create a useful pinch or grasp, and additional surgical procedures may be required.[
Nerve transfers are a more recent addition to our armamentarium of procedures to restore function in SCIs, and they offer several advantages over tendon transfers. These procedures preserve the natural biomechanics of the extremity, maintaining force and excursion and avoiding scar-induced restrictions to movement. They do not require the extended periods of immobilization needed with tendon transfers – an important contributing factor to why most appropriate SCI candidates do not pursue these procedures. Nerve transfer operations provide options for many injuries that are not amenable to tendon transfers, including ICSHT group 0 (as with this patient) and those more proximal. Finally, nerve transfers offer a greater functional gain for a given transfer. That is, the transferred axons, which originally provided innervation to a single muscle and function, can reinnervate multiple target muscles. In this case, central plasticity ensues, often allowing an independent activation of multiple functions by the same axons that originally controlled only a single function. This stands in contrast with tendon transfers in which only one movement can generally be produced per muscle/tendon group transferred.[
At this time we cannot comment on the effectiveness of this intervention, except that it is relatively safe and technically feasible. The second part of this communication will detail the time course of the recovery process over the next 2 years.
CONCLUSION
Nerve transfers are a technically feasible means to restore hand function in the setting of tetraplegia. Compared with tendon transfers, they may be less painful and require less restrictive immobilization for a shorter period of time, with minimal loss to the donor muscle groups. In certain cases of tetraplegia, nerve transfers may offer the recovery of important functions that cannot be achieved through tendon transfers.
References
1. Anastakis DJ, Malessy MJ, Chen R, Davis KD, Mikulis D. Cortical plasticity following nerve transfer in the upper extremity. Hand Clin. 2008. 24: 425-44
2. Anderson KD. Targeting recovery: Priorities of the spinal cord-injured population. J Neurotrauma. 2004. 21: 1371-83
3. Brown JM, Mackinnon SE. Nerve transfers in the forearm and hand. Hand Clin. 2008. 24: 319-40-5
4. Brown JM, Tung TH, Mackinnon SE. Median to radial nerve transfer to restore wrist and finger extension: Technical nuances. Neurosurgery. 2010. 66: 75-83
5. Brown JM, Yee A, Mackinnon SE. Distal median to ulnar nerve transfers to restore ulnar motor and sensory function within the hand: Technical nuances. Neurosurgery. 2009. 65: 966-77
6. Bryden AM, Wuolle KS, Murray PK, Peckham PH. Perceived outcomes and utilization of upper extremity surgical reconstruction in individuals with tetraplegia at model spinal cord injury systems. Spinal Cord. 2004. 42: 169-76
7. Brunelli GA, Brunelli GR. Restoration of walking in paraplegia by transferring the ulnar nerve to the hip: A report on the first patient. Microsurgery. 1999. 19: 223-6
8. Committee S-QE. Spinal Cord Injury. Veteran's Affairs Quality Enhancement Research Initiative: Fact Sheet. 2010. p. 1-2
9. Coulet B, Allieu Y, Chammas M. Injured metamere and functional surgery of the tetraplegic upper limb. Hand Clin. 2002. 18: 399-412-6
10. Curtin CM, Gater DR, Chung KC. Upper extremity reconstruction in the tetraplegic population, a national epidemiologic study. J Hand Surg Am. 2005. 30: 94-9
11. Kakulas BA. Neuropathology: The foundation for new treatments in spinal cord injury. Spinal Cord. 2004. 42: 549-63
12. Kozin SH. Tetraplegia. J Am SocSurg Hand. 2002. 2: 141-52
13. Louie G, Mackinnon SE, Dellon AL, Patterson GA, Hunter DA. Medial antebrachial cutaneous--lateral femoral cutaneous neurotization in restoration of sensation to pressure-bearing areas in a paraplegic: A four-year follow-up. Ann PlastSurg. 1987. 19: 572-6
14. McDowell CL, Moberg CA, House JH. The second International Conference on Surgical Rehabilitation of the Upper Limb in Tetraplegia (quadriplegia). J Hand Surg. 1986. 11A: 604-8
15. Mulcahey MJ, Smith BT, Betz RR. Evaluation of the lower motor neuron integrity of upper extremity muscles in high level spinal cord injury. Spinal Cord. 1999. 37: 585-91
16. Birmingham UA.editors. NSCISC. Spinal Cord Injury Facts and Figures at a Glance. The National SCI Statistical Center. Birmingham, AL: U.S. Department of Education; 2010. p. 1-2
17. Peckham PH, Mortimer JT, Marsolais EB. Upper and lower motor neuron lesions in the upper extremity muscles of tetraplegics. Paraplegia. 1976. 14: 115-21
18. Squitieri L, Chung KC. Current utilization of reconstructive upper limb surgery in tetraplegia. Hand Clin. 2008. 24: 169-73
19. Waters RL, Sie IH, Gellman H, Tognella M. Functional hand surgery following tetraplegia. Arch Phys Med Rehabil. 1996. 77: 86-94