- Department of Neurosurgery, National Neuroscience Institute, King Fahad Medical City,
- Department of Pathology, Division of Neuropathology, King Fahad Medical City, Riyadh, Saudi Arabia.
Correspondence Address:
Sarah Bin Abdulqader, Department of Neurosurgery, National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_331_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sarah Bin Abdulqader1, Basim Noor Elahi1, Azhar Alshoumer2, Gmaan Alzhrani1. Neurenteric cyst of the dorsal craniocervical junction in an adult: A case report and operative video. 08-Jul-2022;13:291
How to cite this URL: Sarah Bin Abdulqader1, Basim Noor Elahi1, Azhar Alshoumer2, Gmaan Alzhrani1. Neurenteric cyst of the dorsal craniocervical junction in an adult: A case report and operative video. 08-Jul-2022;13:291. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11712
Abstract
Background: Neurenteric cysts (NCs) are rarely located in the dorsal craniocervical junction (CCJ).
Case Description: Here, we present a case and show the surgical video of a 24-year-old man with a history of neck pain, progressive hemiparesis, and difficulty swallowing. Radiological images revealed an intradural extramedullary lesion at the dorsal CCJ. Posterior approach with C1–C2 laminectomy for resection of the lesion was performed with significant improvement in symptoms postoperatively. Histopathological examination confirmed the diagnosis of NC.
Conclusion: This case demonstrates a rare location of a NC in an adult patient. Complete excision of the cyst wall and its content is the recommended treatment option.
Keywords: Craniocervical junction, Endodermal cyst, Foramen magnum, Neurenteric cyst
INTRODUCTION
Neurenteric cysts (NCs) (also known as endodermal, enterogenous, and bronchogenic cysts) are benign, rare, congenital lesions that are lined by endodermal cell-derived epithelium.[
CLINICAL PRESENTATION
History and examination
A 24-year-old man presented with a 4-week-history of neck pain, progressive hemiparesis, and mild dysphagia. Neurological examination revealed an increase in tone in the right upper and lower extremities, a power of 4/5 in the proximal muscle group, and a power of 3/5 in the distal muscle groups of the right upper extremities. He also had a power of 4/5 in the right lower extremity. On the left side, he had a normal tone in both upper and lower limbs and a power of 4/5 in both upper and lower extremities. He had positive Hoffman sign and brisk reflexes bilaterally. Cranial nerves examination revealed weakness in the right accessory nerve with a power of 4/5 for shoulder elevation; however, the remaining cranial nerves were intact.
Imaging studies
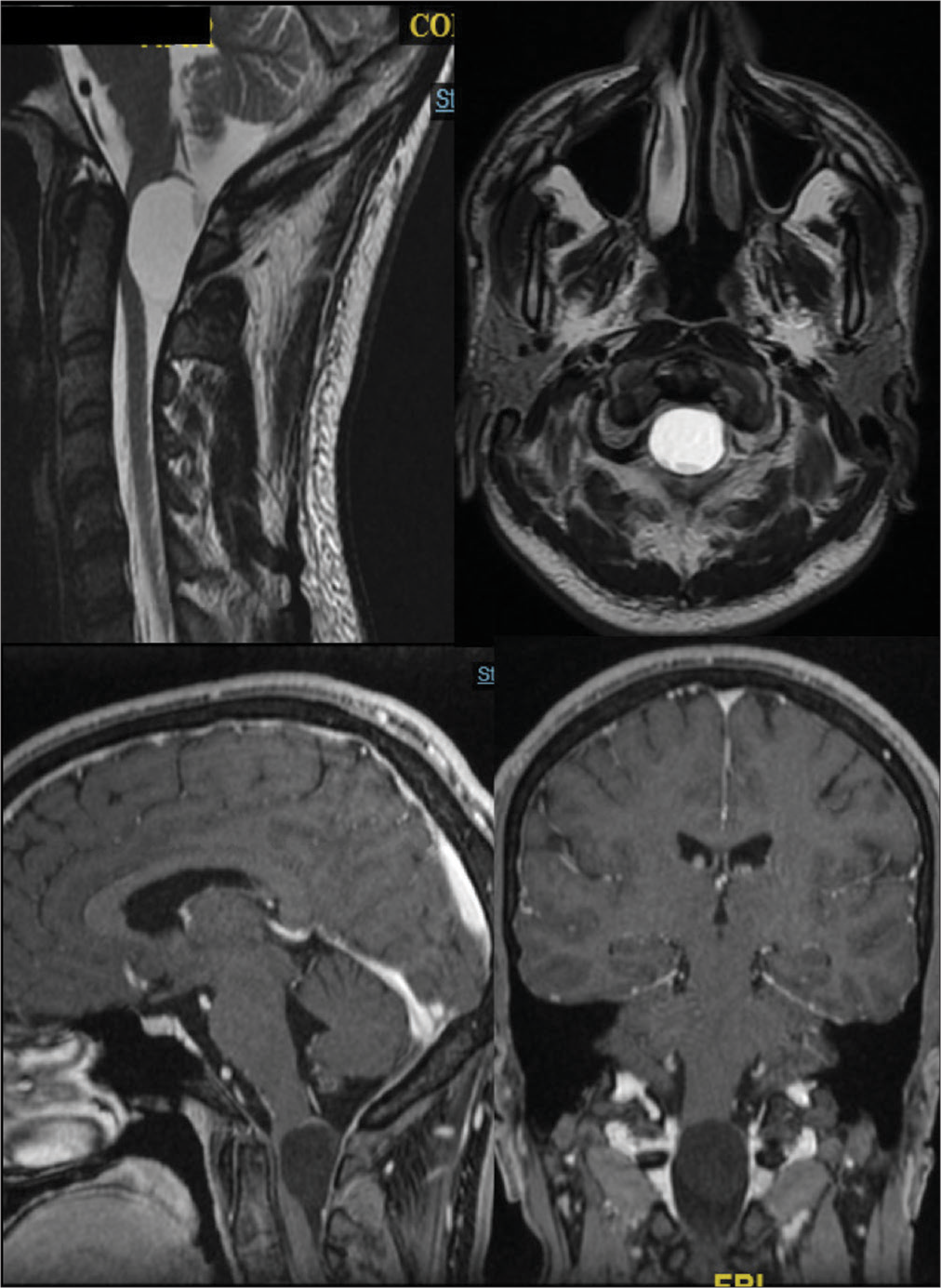
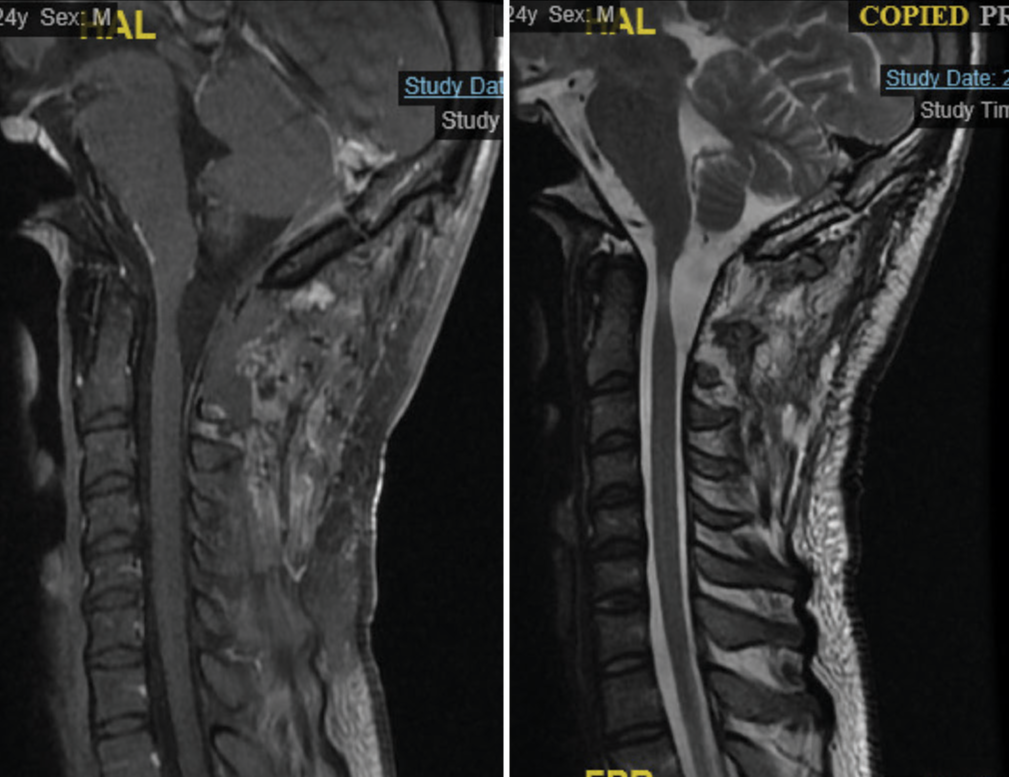
A plain head computed tomography scan and upper cervical spine revealed a hypodense craniocervical lesion up to the C2 level. Magnetic resonance imaging (MRI) of the cervical spine showed an intradural extramedullary lesion centered in the dorsal CCJ measuring 2.2 × 1.9 × 2.6 cm on AP, transverse, and CC dimensions, respectively. It showed increased signal intensity and a fluid-fluid level on T2 sequence and low signal intensity on T1 sequence. The lesion did not show enhancement with gadolinium, with no suppression of fluid-attenuated inversion-recovery sequences and no diffusion restriction on diffusion-weighted imaging [
Figure 1:
Preoperative imaging. Magnetic resonance imaging of the cervical spine showing an intradural extramedullary lesion centered in the dorsal craniocervical junction measuring 2.2 × 1.9 × 2.6 cm on AP, transverse, and CC dimensions, respectively. It showed increased signal intensity and a fluid-fluid level on T2 sequence and low signal intensity on T1 sequence.
Operation
With the aid of intraoperative neuromonitoring, a suboccipital craniotomy with C1–C2 laminectomy was performed to reach the lesion. The patient was placed in the prone position with the head fixed in three-point fixation device. A midline skin incision was made started from the inion to C2. Suboccipital craniotomy was performed followed by C1–C2 laminectomy. The dura was opened starting caudally and proceeding cranially. Tuck-up dural sutures were applied. The lesion came into view; and it was observed to be round, yellowish, with a pedicle attached to the dorsal cord, and traversed with multiple C1 rootlets; subsequently, the arachnoid was carefully incised. Arachnoid attachments were dissected, and the lesion was progressively mobilized. The central mass of the cyst was aspirated and debulked using suction in an attempt to create a safe plane for dissection. The wall of the cyst was dissected and elevated from the obex and the surrounding nerve roots and was ultimately resected. The dura was closed in a watertight fashion using standard measures [
Video 1
Postoperative course and follow-up
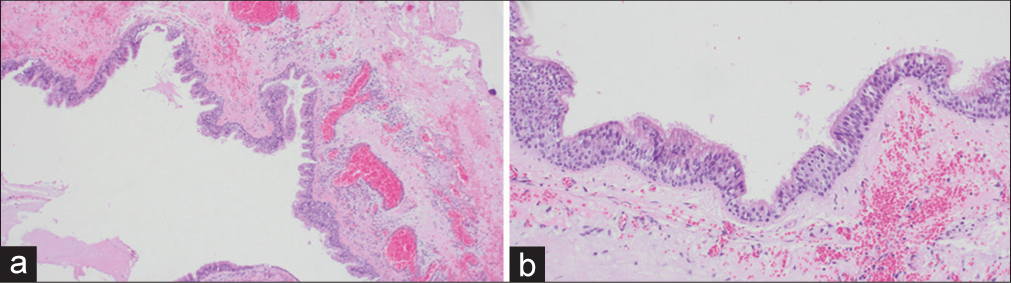
The subsequent histopathological examination confirmed the diagnosis of NC [
DISCUSSION
NCs are rare congenital lesions that represent 0.3–1.3% of all spinal lesions.[
The embryogenesis of NCs remains to be elucidated. Proposed theories include persistence of the neurenteric canal, abnormal vascular supply to the developing neural tissue, or split notochord syndrome.[
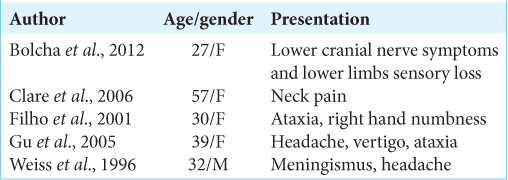
NCs have a male predilection and are commonly documented during the 2nd or 3rd decade.[
Although few cases have shown spontaneous regression,[
The appropriate surgical approach for CCJ NCs depends largely on the location of the cyst. Earlier reports have shown the feasibility of anterior transoral approach and far lateral transcondylar approach for ventrally located cysts. For dorsally located cysts, the posterior approach is advocated as it provides adequate results. It allows early aspiration and decompression of the cyst before manipulating the cyst capsule; therefore, it reduces the risk of injury to neighboring critical structures. Patients with a remnant cyst wall require careful follow-up with serial imaging to detect recurrence.
CONCLUSION
Dorsally located CCJ NCs are rare. Complete resection of the cyst wall and its contents is of paramount importance to prevent recurrence.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bejjani GK, Wright DC, Schessel D, Sekhar LN. Endodermal cysts of the posterior fossa. Report of three cases and review of the literature. J Neurosurg. 1998. 89: 326-35
2. Brooks BS, Duvall ER, el Gammal T, Garcia JH, Gupta KL, Kapila A. Neuroimaging features of neurenteric cysts: Analysis of nine cases and review of the literature. AJNR Am J Neuroradiol. 1993. 14: 735-46
3. Fortuna A, Mercuri S. Intradural spinal cysts. Acta Neurochir (Wien). 1983. 68: 289-314
4. Gauden AJ, Khurana VG, Tsui AE, Kaye AH. Intracranial neuroenteric cysts: A concise review including an illustrative patient. J Clin Neurosci. 2012. 19: 352-9
5. Góes P, Vaz-Guimaraes F, Suriano IC, Araujo S, Zymberg ST. Supratentorial neurenteric cyst: Analysis of 45 cases in the literature. Interdiscip Neurosurg. 2018. 11: 57-64
6. Iglesias J, De la Fuente P, Galbarriatu L, Paternain C, de Gopegui ER, Zaldumbide L. Neurenteric CYST of the craniocervical junction. Case report. Interdiscip Neurosurg. 2021. 23: 100852
7. Kachur E, Ang LC, Megyesi JF. Intraparenchymal supratentorial neurenteric cyst. Can J Neurol Sci. 2004. 31: 412-6
8. Kulkarni V, Daniel RT, Haran RP. Extradural endodermal cyst of posterior fossa: Case report, review of the literature, and embryogenesis. Neurosurgery. 2000. 47: 764-7
9. Lai PMR, Zaazoue MA, Francois R, Dupervil DG, Berkowitz AL, Alexandrescu S. Neurenteric cyst at the dorsal craniocervical junction in a child: Case report. J Clin Neurosci. 2018. 48: 86-9
10. Macdonald RL, Schwartz ML, Lewis AJ. Neurenteric cyst located dorsal to the cervical spine: Case report. Neurosurgery. 1991. 28: 583-7
11. Menéndez RH, D’Osvaldo DH, Vilariño A, Amante MF, Dillon HS. neurenteric cyst of the ventral craniocervical junction: Case report and review of the literature. World Neurosurg. 2019. 125: 257-60
12. Miyagi K, Mukawa J, Mekaru S, Ishikawa Y, Kinjo T, Nakasone S. Enterogenous cyst in the cervical spinal canal. Case report. J Neurosurg. 1988. 68: 292-6
13. Nicholas JE, Neil K, Francesco S, Gerald BB. Neurenteric cyst of the cerebellopontine angle: Case report. Neurosurgery. 1998. 42: 655-8
14. Ohba S, Akiyama T, Kanai R, Onozuka S, Kawase T. Endodermal cyst of the cranio-cervical junction. Acta Neurochir (Wien). 2008. 150: 257-63
15. Preece MT, Osborn AG, Chin SS, Smirniotopoulos JG. Intracranial neurenteric cysts: Imaging and pathology spectrum. AJNR Am J Neuroradiol. 2006. 27: 1211-6
16. Shenoy SN, Raja A. Spinal neurenteric cyst. Report of 4 cases and review of the literature. Pediatr Neurosurg. 2004. 40: 284-92