- Department of Neurosurgery, Faculty of Medicine, Universitas Airlangga/Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia.
DOI:10.25259/SNI_125_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Asra Al Fauzi, Yunus Kuntawi Aji, Rudy Gunawan, Nur Setiawan Suroto. Neuroangiography patterns and anomalies of middle cerebral artery: A systematic review. 25-May-2021;12:235
How to cite this URL: Asra Al Fauzi, Yunus Kuntawi Aji, Rudy Gunawan, Nur Setiawan Suroto. Neuroangiography patterns and anomalies of middle cerebral artery: A systematic review. 25-May-2021;12:235. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10825
Abstract
Background: As the largest and most complex cerebral artery, the middle cerebral artery (MCA) patterns and anomalies are not fully reported. At present, there is confusion about the criteria for the different subtypes. The study of MCA patterns and anomalies is important because variants such as accessories or duplicates represent a high risk of failure during endovascular embolization or navigation during treatment for ischemic stroke. This study conducted a systematic review of studies on the neuroangiography patterns and anomalies of MCA.
Methods: We conducted a systematic review of four articles online databases and included English articles from PubMed, the Cochrane Library, Directory of Open Access Journals, and EBSCOhost.
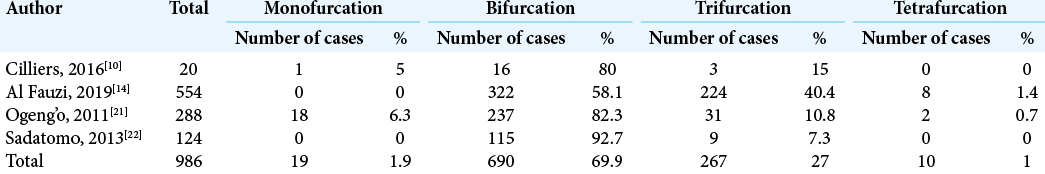
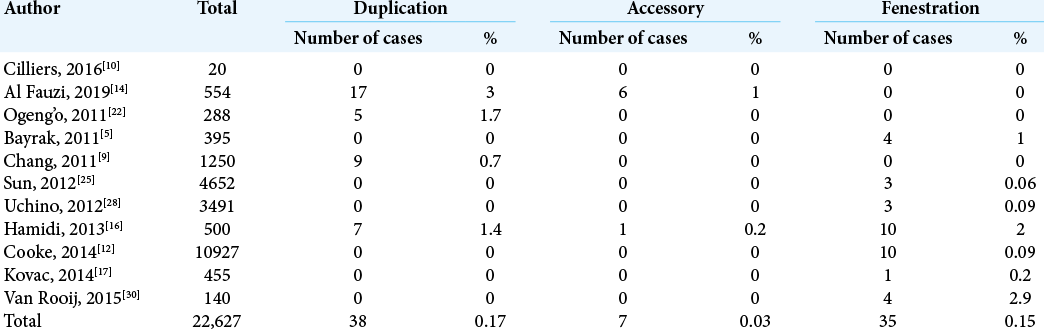
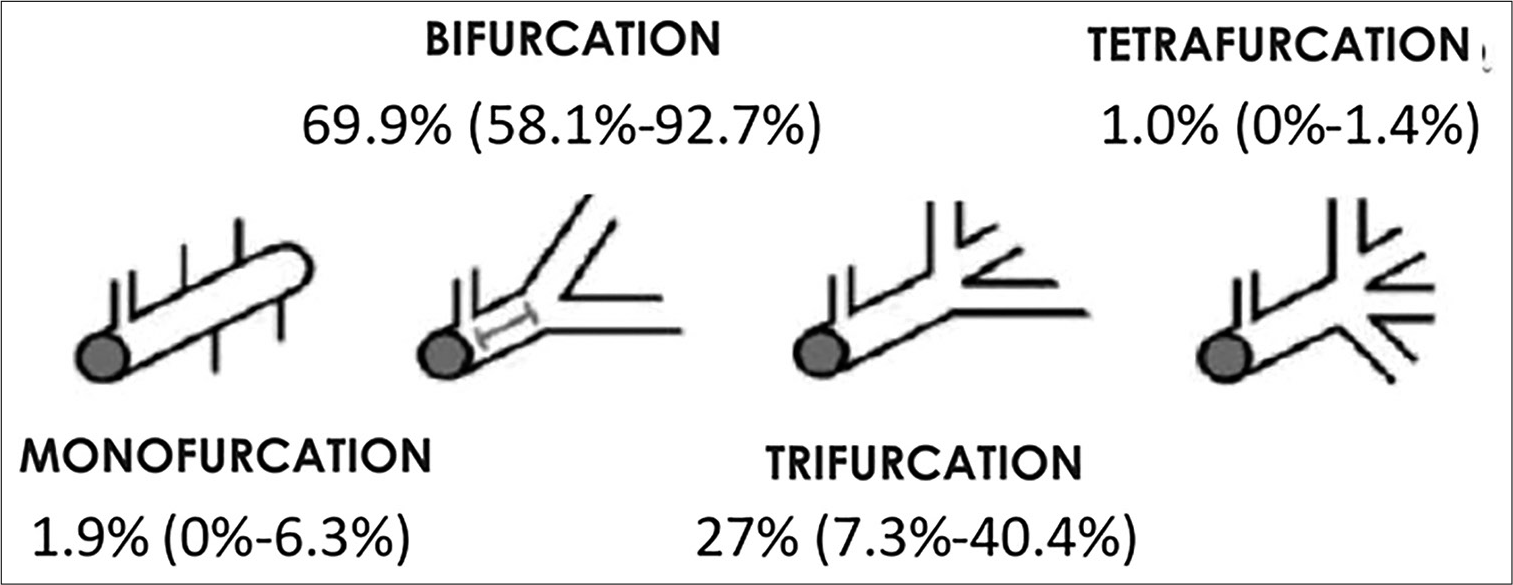
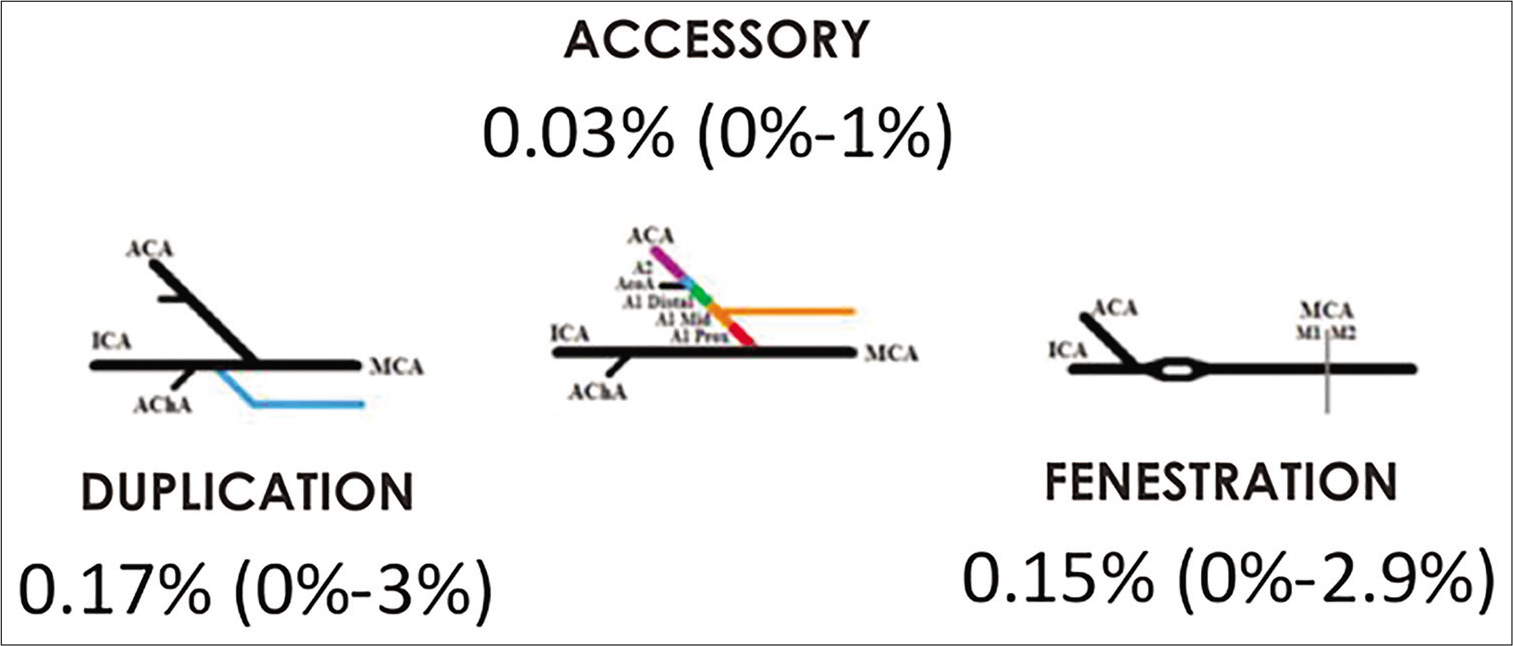
Results: The proportion of the MCA branching pattern was 1.9% (range from 0% to 6.3%) for monofurcation, 1.0% (range from 0% to 1.4%) for tetrafurcation, 69.9% (range from 58.1% to 92.7%) for bifurcation, and 27% (ranging from 7.3% to 40.4%) for trifurcation. The proportion of MCA anomalies for accessory is 0.03% (range from 0% to 1%), duplication is 0.17% (range from 0% to 3%), and fenestration is 0.15% (range from 0% to 2%).
Conclusion: The proportions of the branching pattern and anomalies of MCA based on the systematic review are described in this study. This study is the first to systematically review the neuroangiography pattern of MCA and neuroangiography variations/anomalies of MCA in the literature.
Keywords: Anomaly, Middle cerebral artery, Neuroangiography pattern, Systematic review
INTRODUCTION
The middle cerebral artery (MCA) is the largest and most complex cerebral artery since the cerebral neocortex has developed significantly in humans.[
MATERIALS AND METHODS
The systematic review was carried out following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.[
Search strategy
A literature search was carried out using the Boolean operator AND to search for literature containing all keywords and OR to search for literature containing alternative keywords. (“Middle Cerebral Artery” OR “MCA”) AND (“Neuroangiography” OR “Angiography” OR “Digital Subtraction Angiography” OR “DSA”) AND (“Patterns” OR “Variations” OR “Anomalies”) from literature searches on PubMed, the Cochrane Library, Directory of Open Access Journals, and EBSCOhost. English literature was collected, and no time restriction was applied in the search criteria.
Inclusion criteria
All clinical trials, cohort prospective, retrospective, and observational mentioning patterns and variations or anomalies of MCA in neuroangiography studies were included in the study.
Exclusion criteria
All review articles or consensus statements that did not have clinical information mentioning patterns and variations or anomalies of MCA in neuroangiography studies were excluded from the study.
Data extraction
The following data were extracted from the included studies wherever available: study author(s), year, pattern, and variation or anomalies of MCA, number of samples, race, and age.
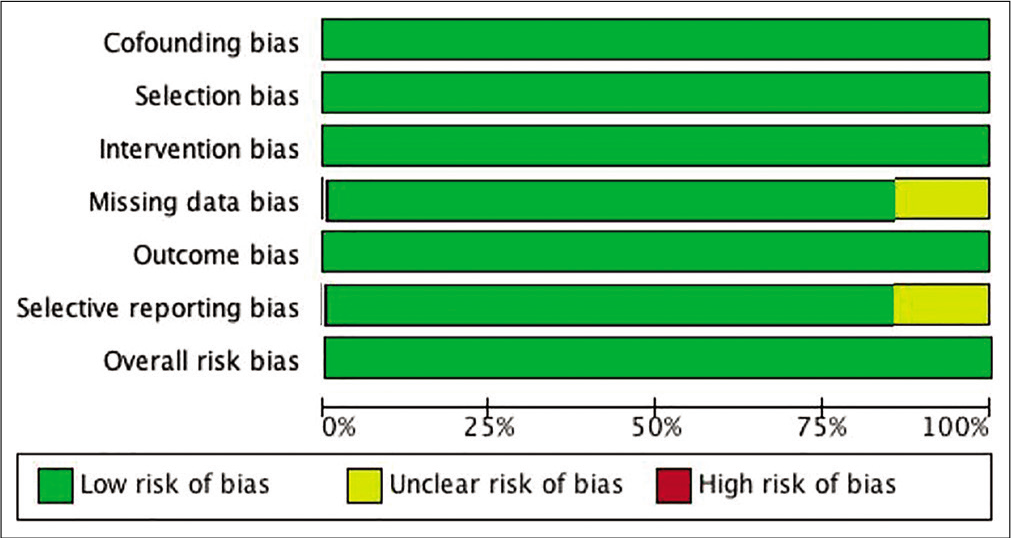
Risk of bias
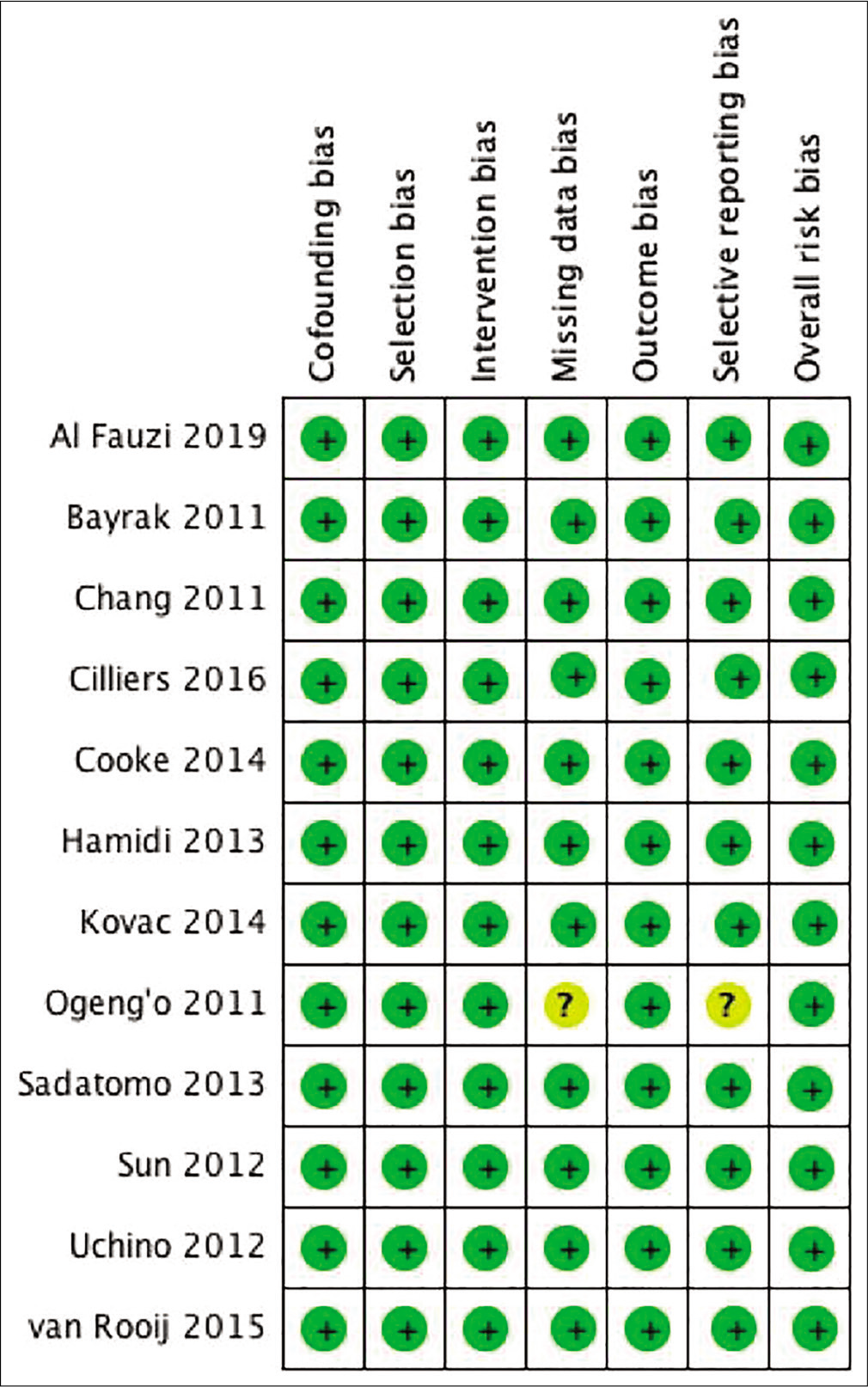
Two researchers analyzed the risk of bias study using the Cochrane Collaboration’s risk of bias tool and a quality assessment for observational studies based on the Newcastle-Ottawa tool according to the Cochrane Handbook for Systematic Reviews of Interventions Chapter, entitled “Assessing risk of bias in a nonrandomized study” [
Management and data analysis
A summary of the evidence used in data synthesis is presented in a summary form containing the characteristics of each study. Descriptive data are presented in the form of text and tables.
RESULTS
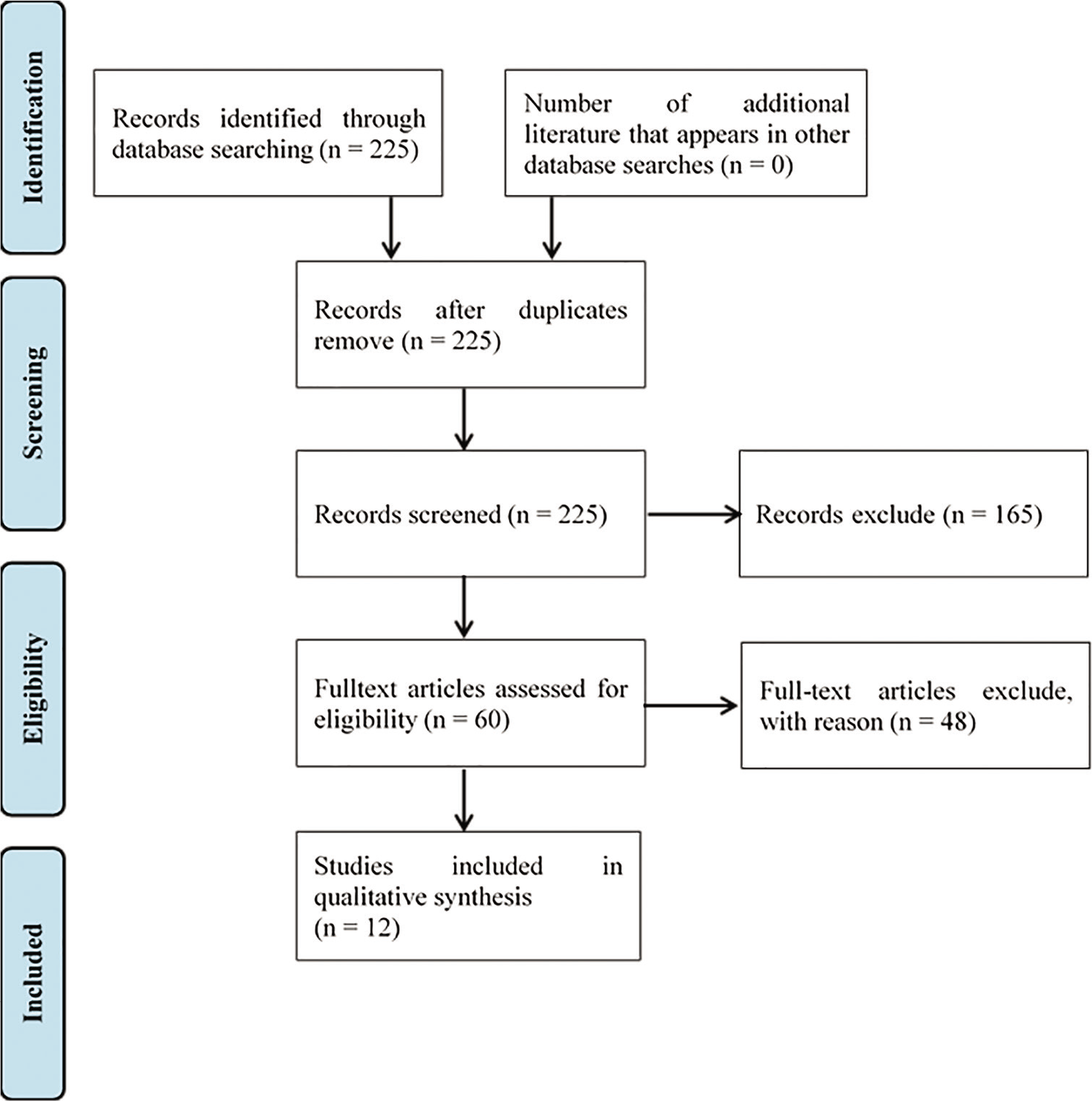
The online journal databases used in the search included PubMed (207 studies), Cochrane (17 studies), DoAJ (1 study), and EBSCO (0 study), for a total of 225 articles. Duplication screening did not reveal any duplicate articles. The screened titles and abstracts were then screened, resulting in 60 articles. The remaining 165 articles that were not related to the research topic were excluded from the study. The full texts of the 60 included articles were further screened. Forty-eight articles were excluded because further reading of the full text showed that the methodology and results did not follow the research we conducted. A total of 12 articles met the inclusion criteria of the study. The flowchart of the research literature search results is presented in [
Characteristics of the MCA literature
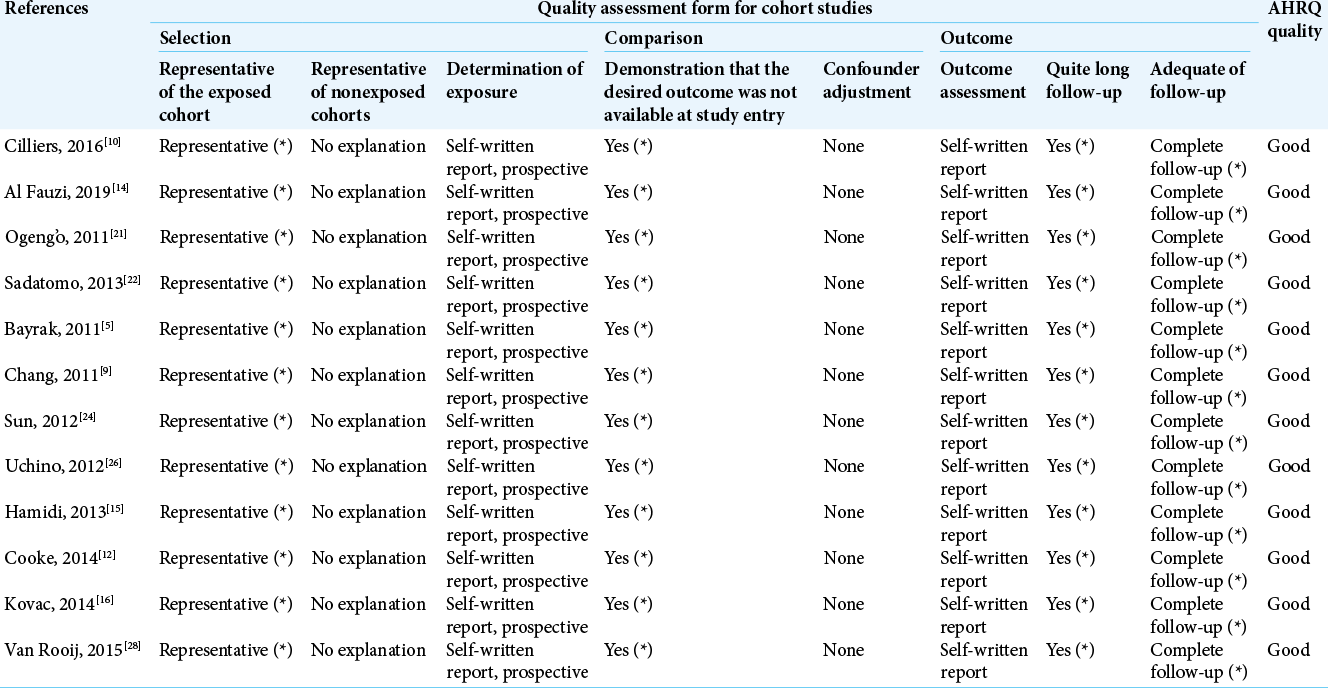
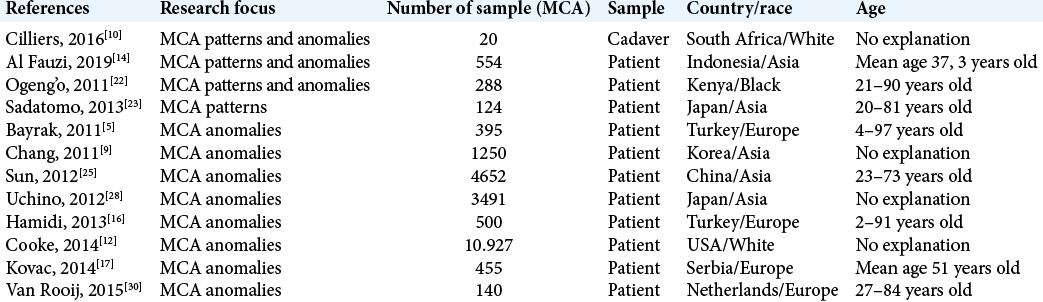
There were 12 studies included in the study, as shown in [
MCA pattern
The MCA branching pattern is determined by the division of the main branch into smaller branches. Bifurcation and trifurcation are most commonly described, although other types have been observed and several subtypes can be identified. Eleven different types of branching can be distinguished from the literature and these include the bifurcation subtypes (medial bifurcation, lateral bifurcation, medial pseudobifurcation, and lateral pseudobifurcation), trifurcation subtypes (true trifurcation, pseudotrifurcation, and lateral pseudobifurcation), and trifurcation (true trifurcation, pseudotrifurcation, distraction trifurcation, and proximal trifurcation).[
MCA anomaly
MCA anomalies occurred less frequently than other major intracranial artery anomalies.[
DISCUSSION
This research was conducted by systematically searching the entire literature on studies that reported patterns and variations/anomalies in MCA. The systematic study included 12 articles that were used for analysis of the MCA patterns.
Quality of the studies used
This systematic review obtained data from the studies using the stipulated study design. The study design used influenced the strength of the research results as levels of evidence that have a clear hierarchy. The hierarchical division began with randomized controlled trial studies as the highest quality, followed by cohort, case–control, and case series.[
Characteristics of the studies
Based on [
Based on [
MCA pattern
Eleven different types of branching can be distinguished from the literature, including the bifurcation subtypes (medial bifurcation, lateral bifurcation, medial pseudobifurcation, and lateral pseudobifurcation) and trifurcation subtypes (true trifurcation, pseudotrifurcation, distal trifurcation, and trifurcation). We classified the patterns into monofurcation, bifurcation, trifurcation, and tetrafurcation, which were the most commonly reported classifications in the literature. According to [
Regarding M1 branch, two branches were the most frequent patterns: the anterosuperior and posteroinferior branches. The orbitofrontal, operculofrontal, and central arteries arose from the anterosuperior branches. The remaining branches originated from the posteroinferior trunk. In the case of trifurcation, orbitofrontal and operculofrontal arose from the anterosuperior trunk. The central angular, parietal, and gyrus arteries arose from the middle branches, and the temporal branches arose from the posteroinferior branches. Another variant characterized by the division of M1 into several branches may also occur, but less frequently.
For the bifurcation subtypes, medial and lateral bifurcations describe the distance of the branching from the origin of the MCA (close or further away, respectively).[
MCA branching occurred at the highest point of the insula limen, proximal to the MCA genu in 86% of cases.[
This variability in the bifurcation pattern can be demonstrated on microanatomic examination and in clinical syndromes associated with divisional occlusion. The inferior division was slightly more dominant (32%). This division covered a wider cortical area than the superior division.
In the trifurcation subtype, true trifurcation was rarely observed. In another trifurcation subtype, the MCA branching and the dominant branch further branched off to give rise to the middle branch. In pseudotrifurcation, the first and second branches were <2 mm apart. With proximal trifurcation, the most common subtype, the two branches were more than 2 mm apart. In the distal trifurcation, the two branches were more than 2 mm apart and more than a quarter of the distance between the origin of the MCA and the first. The apparent trifurcation of MCA occurred in only 12% of the hemisphere.
Grellier et al. described monofurcation as branching after insula limen, although monofurcation can also be called when there was no major branching.[
MCA anomaly
MCA anomalies occurred less frequently than other major intracranial artery anomalies.[
According to [
MCA typically arose from ICA as a single artery. In some cases, two MCAs arose from the ICA, such as an accessory MCA or a duplicate MCA.[
Previous angiography and anatomical studies have shown a prevalence of 0.2–2.9% of duplicated MCAs and 0.3–4.0% of accessory MCA. The occurrence of MCA duplication and accessory MCA variants depended on the modality used (reduced by DSA compared to the autopsy, computed tomography scanning angiography, or magnetic resonance imaging angiography). MCA duplication was almost twice as common as an accessory MCA. In addition to the modality used to detect it, variations in their occurrence may also occur as these two variants were often confused with each other and with other and with more common variants, such as branching or trifurcation of the initial M1 segment.
The types of MCA variations were usually classified according to the descriptions presented by the Teal and Abanou groups. Abanou et al. classified MCA accessories into three types.[
Fenestration is when blood vessels have a common origin, split into two channels, and then recombine. Fenestration (window) refers to the focal opening in the artery (not duplicated in the origin of M1).[
MCA fenestration was rare. Proximal M1 segment fenestration was the most common. Gailloud et al.[
This study was limited by its observational analytic nature and the lack of supplementation data in the form of individual data by all included studies. Race/population and sample size can affect the percentage of branching patterns obtained, and a small number of samples could have increased the findings on one of the MCA anomalies, challenging the reliability of the numbers reported, whereas studies using a large sample size would have a low percentage of MCA variation/anomaly.
Nevertheless, this study is the first to systematically review the neuroangiography pattern of MCA and neuroangiography variations/anomalies of MCA in the literature.
CONCLUSION
Based on the studies included in this systematic review, the proportion of MCA branching patterns included 1.9% (range from 0% to 6.3%) monofurcation, 1.0% (range from 0% to 1.4%) tetrafurcation, 69.9% (range from 58.1% to 92.7%) bifurcation, and 27% (ranging from 7.3% to 40.4%) trifurcation. Accessory anomalies represented 0.03% (range from 0% to 1%), duplication 0.17% (ranges from 0% to 3%), and fenestration 0.15% (ranges from 0% to 2.9%) of the reported MCA anomalies.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abanou A, Lasjaunias P, Manelfe C, Lopez-Ibor L. The accessory middle cerebral artery (AMCA). Diagnostic and therapeutic consequences. Anat Clin. 1984. 6: 305-9
2. Almeida J, Chaddad F, Rhoton A, Oliveira E, Spetzler RF, Yashar M, Kalani S, Nakaji P.editors. Cranial vascular anatomy of the anterior circulation. Neurovascular Surgery. New York: Georg Thieme Verlag; 2015. p. 75-9
3. Baumeister RF, Leary MR. Writing narrative literature reviews. Rev Gen Psychol. 1997. 1: 311-20
4. Baumeister RF, Prinstein M, Patterson M.editors. Writing a literature review. The Portable Mentor: Expert Guide to a Successful Career in Psychology. New York: Springer US; 2013. p. 57-71
5. Bayrak AH, Senturk S, Akay HO, Ozmen CA, Bukte Y, Nazaroglu H. The frequency of intracranial arterial fenestrations: A study with 64-detector CT-angiography. Eur J Radiol. 2011. 77: 392-6
6. Bem D. Writing a review article for psychological bulletin. Psychol Bull. 1995. 118: 172-7
7. Bradac GB, Bradac GB.editors. Middle cerebral artery. Applied Cerebral Angiography. Berlin, Germany: Springer International Publishing; 2017. p. 81-93
8. Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011. 128: 305-10
9. Chang HY, Kim MS. Middle cerebral artery duplication: Classification and clinical implications. J Korean Neurosurg Soc. 2011. 49: 102-6
10. Cilliers K, Page BJ. Anatomy of the middle cerebral artery: Cortical branches, branching pattern and anomalies. Turk Neurosurg. 2017. 27: 671-81
11. Collaboration C. Glossary of Terms in The Cochrane Collaboration. Available from: http://www.webcache.googleusercontent.com/search?q=cache:uUiWPzMji9UJ:aaz.hr/resources/pages/57/7.%2520Cochrane%2520glossary.pdf+&cd=2&hl=en&ct=clnk&gl=id [Last accessed on 2021 Jan 28].
12. Cooke DL, Stout CE, Kim WT, Kansagra AP, Yu JP, Gu A. Cerebral arterial fenestrations. Interv Neuroradiol. 2014. 20: 261-74
13. Cooper H.editors. Psychological bulletin: Editorial. Psychol Bull. 2003. 129: 3-9
14. Fauzi AA, Aji YK, Suroto NS. Neuroangiography patterns of the middle cerebral artery: Study of 554 cerebral angiography results. J Clin Neurosci. 2019. 68: 62-8
15. Gailloud P, Albayram S, Fasel JH, Beauchamp NJ, Murphy KJ. Angiographic and embryologic considerations in five cases of middle cerebral artery fenestration. AJNR Am J Neuroradiol. 2002. 23: 585-7
16. Hamidi C, Bükte Y, Hattapoğlu S, Ekici F, Tekbaş G, Önder H. Display with 64-detector MDCT angiography of cerebral vascular variations. Surg Radiol Anat. 2013. 35: 729-36
17. Kovač JD, Stanković A, Stanković D, Kovač B, Šaranović D. Intracranial arterial variations: A comprehensive evaluation using CT angiography. Med Sci Monit. 2014. 20: 420-7
18. Krings T, Geibprasert S, Cruz J, Terbrugge K.editors. Neurovascular Anatomy, in Neurovascular Anatomy in Interventional Neuroradiology. New York: Thieme; 2015. p. 62-82
19. McKinney AM, McKinney AM.editors. Intracranial Anterior Circulation Variants, in Atlas of Normal Imaging Variations of the Brain, Skull, and Craniocervical Vasculature. Mineapolis: Springer International; 2017. p. 1087-97
20. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009. 151: 264-9, W64
21. Morris P.editors. The middle cerebral artery. Practical Neuroangiography. Philadelphia, PA: Lippincott Williams and Wilkins; 2015. p. 175-81
22. Ogeng’o JA, Njongo W, Hemed E, Obimbo MM, Gimongo J. Branching pattern of middle cerebral artery in an African population. Clin Anat. 2011. 24: 692-8
23. Sadatomo T, Yuki K, Migita K, Imada Y, Kuwabara M, Kurisu K. Differences between middle cerebral artery bifurcations with normal anatomy and those with aneurysms. Neurosurg Rev. 2013. 36: 437-45
24. Siddaway AP, Wood AM, Hedges LV. How to do a systematic review: A best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019. 289: 747-70
25. Sun ZK, Li M, Li MH, Li YD, Sun WP, Zhu YQ. Fenestrations accompanied by intracranial aneurysms assessed with magnetic resonance angiography. Neurol India. 2012. 60: 45-9
26. Takahashi M, Uchino A, Suzuki C. Anastomosis between accessory middle cerebral artery and middle cerebral artery diagnosed by magnetic resonance angiography. Surg Radiol Anat. 2017. 39: 685-7
27. Teal JS, Rumbaugh CL, Bergeron RT, Segall HD. Anomalies of the middle cerebral artery: Accessory artery, duplication, and early bifurcation. Am J Roentgenol Radium Ther Nucl Med. 1973. 118: 567-75
28. Uchino A, Saito N, Okada Y, Nakajima R. Duplicate origin and fenestration of the middle cerebral artery on MR angiography. Surg Radiol Anat. 2012. 34: 401-4
29. Uchiyama N. Anomalies of the middle cerebral artery. Neurol Med Chir (Tokyo). 2017. 57: 261-6
30. van Rooij SB, Bechan RS, Peluso JP, Sluzewski M, van Rooij WJ. Fenestrations of intracranial arteries. AJNR Am J Neuroradiol. 2015. 36: 1167-70
31. van Rooij SB, van Rooij WJ, Sluzewski M, Sprengers ME. Fenestrations of intracranial arteries detected with 3D rotational angiography. AJNR Am J Neuroradiol. 2009. 30: 1347-50
32. Viswanathan M, Patnode CD, Berkman ND, Bass EB, Chang S, Hartling L.editors. Assessing the Risk of Bias in Systematic Reviews of Health Care Interventions. Rockville, MD: Agency for Healthcare Research and Quality; 2008. p.