- Department of Neurosurgery, University of Kansas Medical Center, Kansas City, KS, USA
- School of Medicine, University of Kansas Medical Center, Kansas City, KS, USA
Correspondence Address:
Kyle Anthony Smith
Department of Neurosurgery, University of Kansas Medical Center, Kansas City, KS, USA
DOI:10.4103/2152-7806.161240
Copyright: © 2015 Smith KA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Smith KA, Lavin P, Chamoun R. Neuroendoscopic treatment of symptomatic giant Virchow–Robin spaces. Surg Neurol Int 20-Jul-2015;6:120
How to cite this URL: Smith KA, Lavin P, Chamoun R. Neuroendoscopic treatment of symptomatic giant Virchow–Robin spaces. Surg Neurol Int 20-Jul-2015;6:120. Available from: http://surgicalneurologyint.com/surgicalint_articles/neuroendoscopic-treatment-of-symptomatic-giant-virchow-robin-spaces/
Abstract
Background:Virchow-Robin spaces (VRS) or perivascular spaces are interstitial cystic spaces surrounding the vasculature of brain parenchyma and course from the subarachnoid space. Small VRS (less than 2 mm) appear in all age groups, but can enlarge and be confused with other lesions like cystic neoplasms. These enlarged VRS are termed giant tumefactive perivascular spaces (GRPVS).
Case Description:We present the case of a 50-year-old male who presents with right eye pain, blurred vision, headache, and gait imbalance. He was diagnosed with GRPVS and underwent an endoscopic third ventriculostomy and cyst fenestration. Postoperative imaging showed a decrease in size of the ventricular system with evidence of flow through the aqueduct and ventriculostomy. Brainstem VRS cysts decreased in size.
Conclusion:Unlike the other small number of case reports, this patient is unique in his age of presentation and successful endoscopic method of treatment. The endoscopic approach provided great exposure and adequate access to the lesions. Clinically, symptoms improved, cyst size decreased, and need for permanent shunt placement was averted.
Keywords: Cyst fenestration, endoscopy, neuroendoscopy, Virchow-Robin spaces
INTRODUCTION
Virchow–Robin spaces (VRS) are spaces that surround the walls of vessels within the brain parenchyma. VRS are found in all age groups but may increase in size and frequency with age.[
CASE REPORT
History
This 50-year-old male presented to our inpatient neurosurgical serve with complaints of right eye pain, blurred vision and occasional diplopia, headache, and gait difficulty with frequent falls due to imbalance. He denies numbness or weakness of extremities. Past medical history included type II diabetes, hypertension, and hyperlipidemia.
Examination
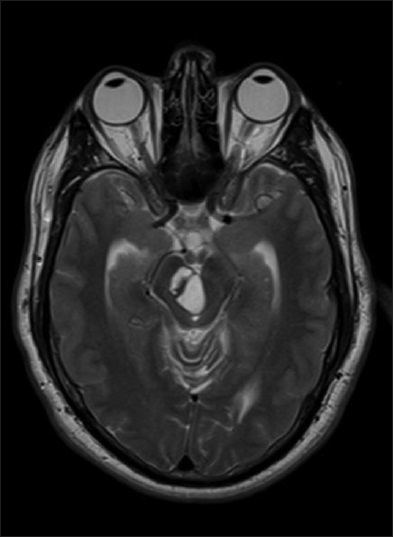
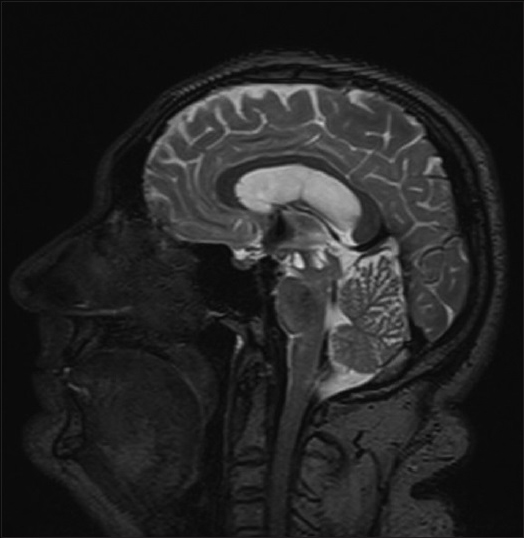
On exam, he was alert and oriented to person, place, and time. He had decreased vision in right eye and diplopia on extreme lateral gaze. Subtle horizontal nystagmus was noted. The remaining cranial nerve exam was grossly intact. Patient had normal strength and sensation in all four extremities. He had negative Romberg sign but mildly ataxic gait. Magnetic resonance imaging (MRI) without contrast showed a stable cluster of three cysts centered within the tegmentum of the right midbrain, which in aggregate measured 2.2 cm × 1.4 cm × 1.4 cm [
Operation
Under general anesthesia, the patient was fixed in Mayfield head holder, and stereotactic navigation was registered for use during the procedure. Two burr holes were placed. A posterior burr hole was planned in the right frontal area near the coronal suture in order to perform the ETV. A second burr hole was planned anterior to the first one in order to access the brainstem cyst and the posterior third ventricle. The endoscope was introduced through the posterior burr hole into the lateral ventricle and through the foramen of Monro into the third ventricle. Third ventriculostomy was performed in the usual fashion in the floor of the ventricle, anterior to the mammillary bodies. Next, the endoscope was introduced through the anterior frontal burr hole and taken into the third ventricle through the foramen of Monro in a more posterior trajectory in order to reach the brainstem cyst. Fenestration of the cyst was performed with the endoscopic bipolar. Contents of the cyst were consistent with pure cerebrospinal fluid. An external ventricular drain (EVD) was left for intracranial pressure monitoring following the procedure. The closure was done using burr hole covers and routine skin closure. The patient tolerated the procedure well and was transferred to the intensive care unit for further monitoring and care.
Postoperative course
Intracranial pressures remained within normal limits, and the EVD was removed the following morning after surgery. Patient was able to ambulate without assistance with minimal pathway deviations and perform daily activities of living independently. Cognition remained intact, and he conversed appropriately. Postoperative MRI showed a decrease in size of the ventricular system with evidence of flow through the aqueduct and ostium of the ETV. There was a stable appearance of cystic lesions in the brain stem with some decrease in size [
At 1-month follow-up his gait, diplopia, and headache had significantly improved. At 5 months, headache, and diplopia had essentially resolved, and computed tomography scan showed well-decompressed cyst and ventricles [
DISCUSSION
Virchow–Robin spaces are interstitial fluid-filled potential spaces that surround cerebral arteries and arterioles.[
References
1. Fayeye O, Pettorini BL, Foster K, Rodrigues D. Mesencephalic enlarged Virchow-Robin spaces in a 6-year-old boy: A case-based update. Childs Nerv Syst. 2010. 26: 1155-60
2. Flors L, Leiva-Salinas C, Cabrera G, Mazón M, Poyatos C. Obstructive hydrocephalus due to cavernous dilation of Virchow-Robin spaces. Neurology. 2010. 74: 1746-
3. House P, Salzman KL, Osborn AG, MacDonald JD, Jensen RL, Couldwell WT. Surgical considerations regarding giant dilations of the perivascular spaces. J Neurosurg. 2004. 100: 820-4
4. Kwee RM, Kwee TC. Virchow-Robin spaces at MR imaging. Radiographics. 2007. 27: 1071-86
5. Morisako H, Tuyuguchi H, Nagata T, Chokyu I, Ichinose T, Ishibashi K. Enlarged perivascular spaces associated with hydrocephalus: A case report. No Shinkei Geka. 2009. 37: 681-6
6. Papayannis CE, Saidon P, Rugilo CA, Hess D, Rodriguez G, Sica RE. Expanding Virchow Robin spaces in the midbrain causing hydrocephalus. AJNR Am J Neuroradiol. 2003. 24: 1399-403
7. Rohlfs J, Riegel T, Khalil M, Iwinska-Zelder J, Mennel HD, Bertalanffy H. Enlarged perivascular spaces mimicking multicystic brain tumors.Report of two cases and review of the literature. J Neurosurg. 2005. 102: 1142-6
8. Salzman KL, Osborn AG, House P, Jinkins JR, Ditchfield A, Cooper JA. Giant tumefactive perivascular spaces. AJNR Am J Neuroradiol. 2005. 26: 298-305
9. Staines DR, Brenu EW, Marshall-Gradisnik S. Postulated role of vasoactive neuropeptide-related immunopathology of the blood brain barrier and Virchow-Robin spaces in the aetiology of neurological-related conditions. Mediators Inflamm 2008. 2008. p.