- Department of Plastic Surgery, Liaquat National Hospital, Karachi, Sindh, Pakistan.
Correspondence Address:
Mirza Shehab Afzal Beg, Department of Plastic Surgery, Liaquat National Hospital, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_596_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Touqeer Hussain, Iqra Khan, Mehtab Ahmed, Mirza Shehab Afzal Beg. Neurotization of musculocutaneous nerve with intercostal nerve versus phrenic nerve – A retrospective comparative study. 15-Jul-2022;13:305
How to cite this URL: Touqeer Hussain, Iqra Khan, Mehtab Ahmed, Mirza Shehab Afzal Beg. Neurotization of musculocutaneous nerve with intercostal nerve versus phrenic nerve – A retrospective comparative study. 15-Jul-2022;13:305. Available from: https://surgicalneurologyint.com/surgicalint-articles/11719/
Abstract
Background: Brachial plexus injuries are common after both blunt and penetrating traumas resulting in upper limb weakness. The nerve transfer to the affected nerve distal to the injury site is a good option where proximal stump of the nerve is unhealthy or absent which has shown early recovery and better results. Commonly used procedures to restore elbow flexion are ipsilateral phrenic or ipsilateral intercostal nerves (ICNs) in global plexus injuries. The use of both intercostal and phrenic nerves for elbow flexion is well described and there is no definite consensus on the superiority of one on another.
Methods: All patients presented in the outpatient department of LNH and MC from January 2014 to December 2017 with pan plexus or upper plexus injury with no signs of improvement for at least 3 months were included in the study. After 3 months of conservative trial; surgery offered to patients.
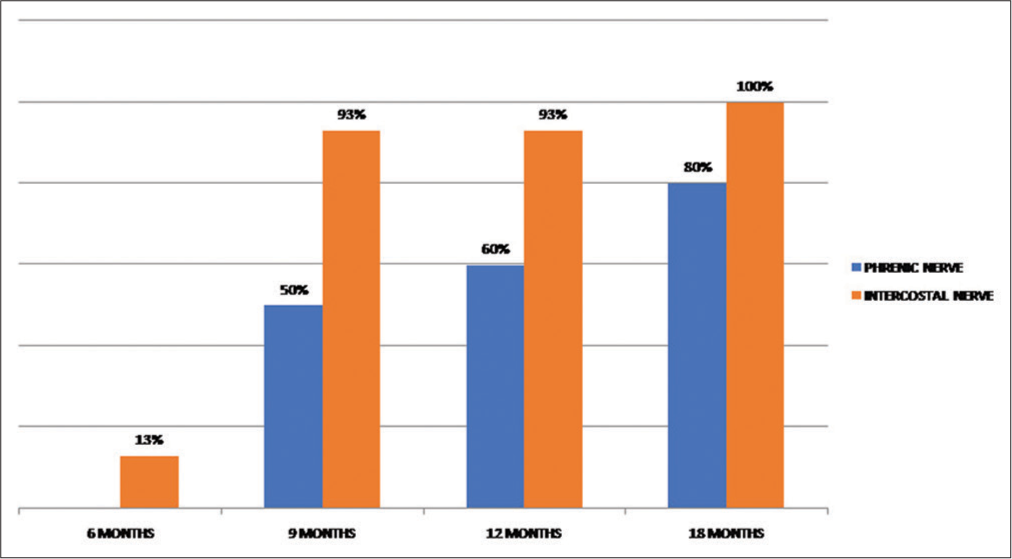
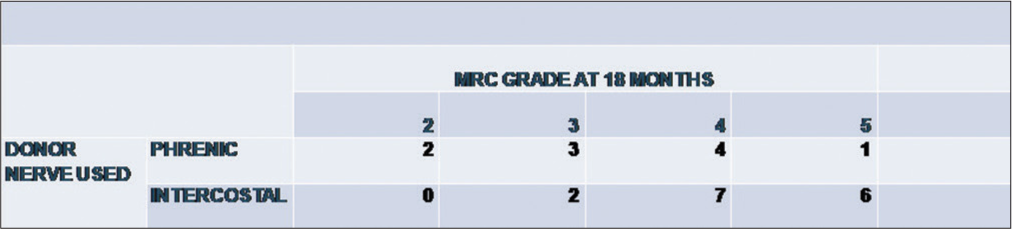
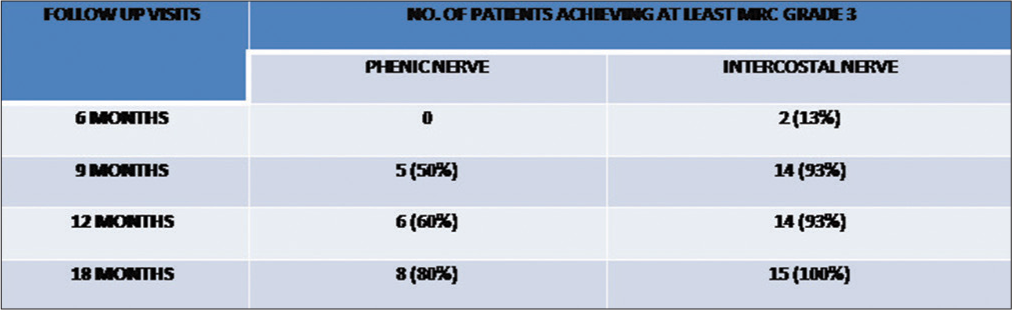
Results: A total of 25 patients (n = 25) were operated from January 2015 to December 2017. Patients were followed to record Medical Research Council (MRC) grades at 3, 6, 9, 12, and 18 months. The patients achieved at least MRC Grade 3; 70% at 12 months follow-up to 80% at 18 months in the phrenic nerve transfer group. While in the ICN transfer group, it is 86% and 100% at 12 and 18 months postoperative, respectively.
Conclusion: Our study has shown better results with ICN transfers to musculocutaneous nerve, recorded on MRC grading system.
Keywords: Brachial plexus injury, Intercostal nerve transfer, Musculocutaneous nerve injury, Neurotization, Phrenic nerve transfer
INTRODUCTION
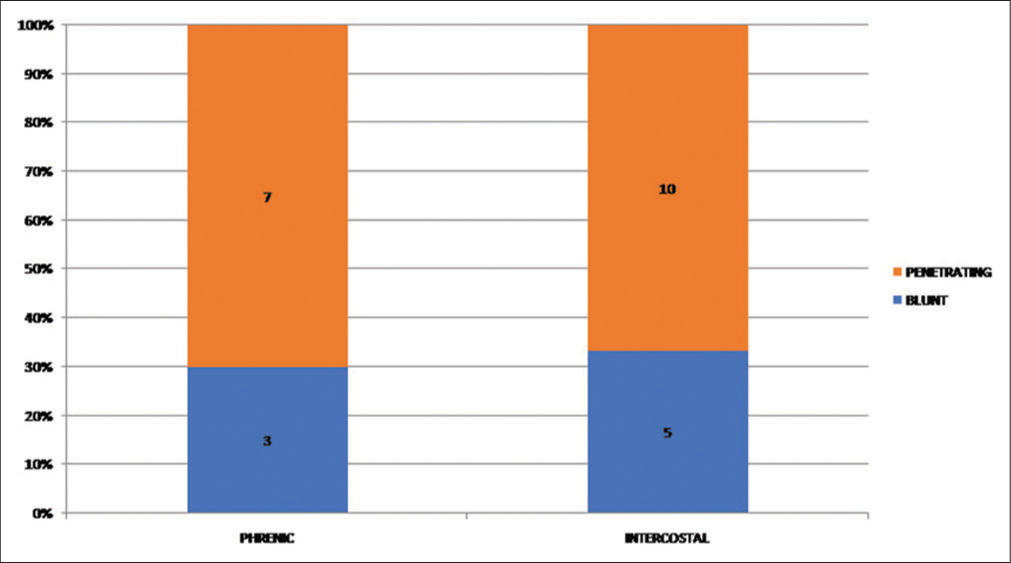
Brachial plexus injuries are common after both blunt and penetrating traumas. Treatment modalities depend on the mechanism of injury, location, as well as the timing of presentation of the patient to reconstructive surgeon.[
Failure of conservative approach, that is, no signs of improvement after 3–6 months, needs surgical exploration.[
Commonly used procedures to restore elbow flexion are fascicle transfer from the median or ulnar nerve in isolated musculocutaneous nerve injury (single/double Oberlin transfer),[
Although neurotization of musculocutaneous nerve with intercostal nerves and phrenic nerve is well known time tested procedures with abundant studies in literature, there are limited data which show comparison of these when both performed at a single center by the same surgeon. Our study is one of its kinds showing comparison of the two abovementioned donor nerves.
This study aims to compare the difference in functional outcomes of phrenic and ICN transfer when used as donor nerve for musculocutaneous nerve to restore elbow flexion.
MATERIALS AND METHODS
Patient population
All the patients who presented in the outpatient department of Liaquat National Hospital and Medical College from January 2014 to December 2017 with pan plexus or upper plexus injury with no signs of improvement for at least 3 months were included in the study. Patients with a history of rib fracture, thoracotomy, or chest tube placement are not considered for ICN transfer. After 3 months of conservative trial, NCS/EMG was done in all patients, and surgery was offered to patients with no clinical or electromyographical signs of improvement. A routine hematological workup was done for anesthesia assessment. Chest X-ray was done in all patients preoperatively to exclude phrenic nerve injury by checking diaphragm level.
Statistical analysis
Preoperative clinical examination was performed by operating surgeon with its documentation. Postoperatively, the patients followed at 3, 6, 9, 12, and 18 months. The outcome of elbow flexion is assessed through the MRC grading system by the operating surgeon and recorded. MRC Grade 3 was considered useful. Data analyzed on SPSS version 2019.
Operative technique
For ICN
We used three ICNs (3rd, 4th, and 5th) for transfer. Patients with a history of rib fracture or any surgical intervention to ipsilateral hemithorax were excluded from the study. Harvest is done through a single inframammary incision extending from the mid-axillary line to the costochondral junction. ICNs are identified by dissecting through subcutaneous tissues, pectoralis major, pectoralis minor, and intercostal muscles.[
For phrenic nerve
The phrenic nerve is explored through the supraclavicular incision and mobilized until it enters into thorax where it is divided and transferred directly to the musculocutaneous nerve without nerve grafts. The subjects in which nerve graft is required are excluded from the study to keep homogeneity.[
RESULTS
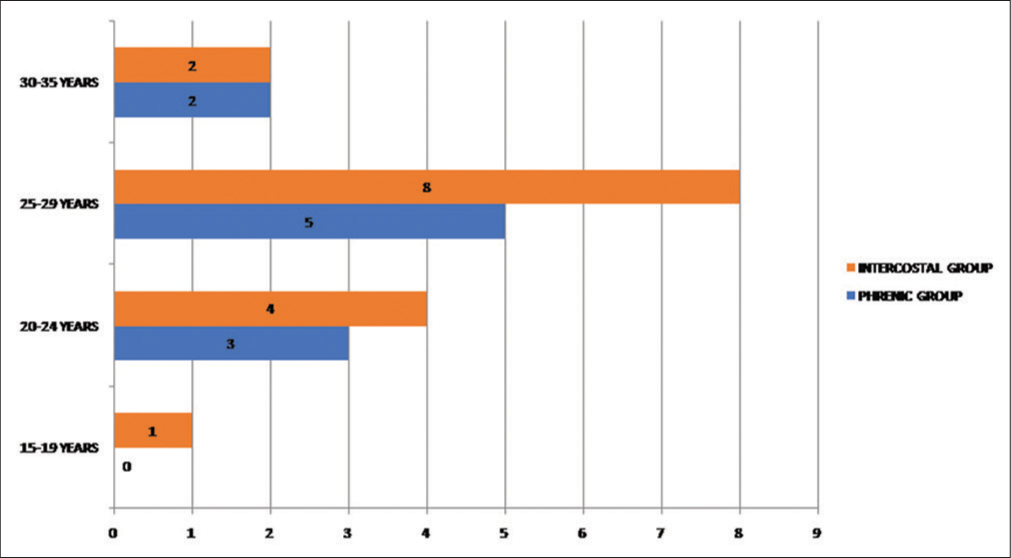
A total of 25 patients (n = 25) were operated from January 2015 to December 2017. Musculocutaneous nerve was neurotized with ICNs in 15 patients (group 1) while in 10 patients, phrenic was used as a donor nerve (Group 2). All the patients were male. The mean age of patients was 26 ± 2 years in phrenic and 26 ± 3 in the ICNs transfer group [
At 18 months of follow-up, MRC grade-wise distribution of patients of phrenic nerve transfer group showed one patient in MRC Grade 5, four patients in MRC Grade 4, three patients in MRC Grade 3, two in MRC Grade 2, and no patient in MRC Grades 1 and 0 (no muscle contraction at all) while in the ICN transfer group, most of the patients were in MRC Grade 4 (46% n = 7), 40% (n = 6) achieved MRC Grade 5, two patients achieved MRC Grade 3 while no patient was in MRC Grades 0, 1, and 2 [
No respiratory complications were observed in postoperative period in both groups.
DISCUSSION
Traumatic global brachial plexus injury is a debilitating injury and more severe if dominant side is affected. It may hinder the daily activities of life including feeding, writing, and house chores. The recovery of elbow function is the elemental function with brachial plexus injury. Surgical intervention is usually deferred till 3–6 months in hope of spontaneous recovery in blunt injuries. Nerve surgery is usually advised from 6 to 9 months postinjury. Nerve surgery after 1 year is typically not advised.[
The ICN contains both motor and sensory fibers. It has approximately 1300 axons having fewer motor fibers distally rather than proximally. However, in comparison to it, the phrenic nerves contain approximately 1756 myelinated nerve fibers and are mostly motor (70.1%).[
As per Kang et al., the study showed elbow flexion MRC grade of M3 or greater at 2 years[
It has been observed in studies that after phrenic nerve transfers, the patients develop respiratory symptoms that have comorbidities including chronic obstructive pulmonary diseases and obesity, as it may worsen dyspnea, mostly in lying position.[
The phrenic nerve plays an important role in respiration; but it can be sacrificed without causing much difficulty in respiratory function in most patients. As per the study of Luedemann et al., the division of right phrenic nerve affects more respiration rather than the left-sided phrenic nerve transection.[
There is no agreement about the paramount functional outcome scale for patients with brachial plexus injuries; the disabilities of the arm, shoulder, and hand (DASH) outcome questionnaire are frequently used. Wilcox et al. recommended that fatigue was a clinically pertinent characteristic of reinnervated muscles after surgery while in most studies, the MRC grading system is used to evaluate the outcome and a biceps strength ≥M3 is considered a good result.[
Limitation of the study included retrospective design and there was no control group. It was single center with limited number of patients. Besides that, it was not blinded. Either there was no evaluation of pulmonary function or documentation of any complications. They would have strengthened our study if they were reported.
CONCLUSION
Our study has shown better results with ICN transfers to musculocutaneous transfer without any respiratory sequel. We strongly recommend use of intercostal for musculocutaneous neurotization whenever possible because of higher MRC grades achieved as compared to phrenic nerve.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ali ZS, Heuer GG, Faught RW, Kaneriya SH, Sheikh UA, Syed IS. Upper brachial plexus injury in adults: Comparative effectiveness of different repair techniques. J Neurosurg. 2015. 122: 195-201
2. Blaauw G, Muhlig R, Vredeveld J. Management of brachial plexus injuries. Adv Tech Stand Neurosurg. 2008. 33: 201-31
3. de Mendonça Cardoso M, de Amoreira Gepp R, Mamare E, Guedes-Correa JF. Results of phrenic nerve transfer to the musculocutaneous nerve using video-assisted thoracoscopy in patients with traumatic brachial plexus injury: Series of 28 cases. Oper Neurosurg. 2019. 17: 261-7
4. de Mendonça Cardoso M, Gepp R, Correa JF. Outcome following phrenic nerve transfer to musculocutaneous nerve in patients with traumatic brachial palsy: A qualitative systematic review. Acta Neurochirurg. 2016. 158: 1793-800
5. Gu Y, Ma MK. Use of the phrenic nerve for brachial plexus reconstruction. Clin Orthop Relat Res. 1996. 323: 119-21
6. Hems T. Nerve transfers for traumatic brachial plexus injury: advantages and problems. J Hand Microsurg. 2011. 3: 6-10
7. Kaiser R, Waldauf P, Ullas G, Krajcová A. Epidemiology, etiology, and types of severe adult brachial plexus injuries requiring surgical repair: Systematic review and meta-analysis. Neurosurg Rev. 2020. 43: 443-52
8. Kang GH, Lim RQ, Yong FC. Elbow flexion reconstruction in brachial plexus avulsion injuries-results with intercostal nerve and distal nerve transfers. J Hand Surg. 2020. 25: 307-14
9. Leland HA, Azadgoli B, Gould DJ, Seruya M. Investigation into the optimal number of intercostal nerve transfers for musculocutaneous nerve reinnervation: A systematic review. Hand (N Y). 2018. 13: 621-6
10. Limthongthang R, Bachoura A, Songcharoen P, Osterman AL. Adult brachial plexus injury: Evaluation and management. Orthop Clin North Am. 2013. 44: 591-603
11. Luedemann W, Hamm M, Blömer U, Samii M, Tatagiba M. Brachial plexus neurotization with donor phrenic nerves and its effect on pulmonary function. J Neurosurg. 2002. 96: 523-6
12. Martins RS, Siqueira MG, Heise CO, Foroni L, Teixeira MJ. A prospective study comparing single and double fascicular transfer to restore elbow flexion after brachial plexus injury. Neurosurgery. 2013. 72: 709-15
13. Monreal R. Restoration of elbow flexion by transfer of the phrenic nerve to musculocutaneous nerve after brachial plexus injuries. Hand. 2007. 2: 206-11
14. Narakas A. The treatment of brachial plexus injuries. Int Orthop. 1985. 9: 29-36
15. Socolovsky M, Malessy M, Bonilla G, Di Masi G, Conti ME, Lovaglio A. Phrenic to musculocutaneous nerve transfer for traumatic brachial plexus injuries: Analyzing respiratory effects on elbow flexion control. J Neurosurg. 2018. 131: 165-74
16. Terzis JK, Barbitsioti A. Primary restoration of elbow flexion in adult post traumatic plexopathy patients. J Plast Reconstr Aesthetic Surg. 2012. 65: 72-84
17. Thatte MR, Babhulkar S, Hiremath A. Brachial plexus injury in adults: Diagnosis and surgical treatment strategies. Ann Indian Acad Neurol. 2013. 16: 26-33
18. Tsuyama N, Hara T, Maehiro S, Imoto T. Intercostal nerve transfer for traumatic brachial nerve palsy, Seikeigeka. Orthopedic surgery. 1969. 20: 1527-9
19. Tung TH, Mackinnon SE. Nerve transfers: Indications, techniques, and outcomes. J Hand Surg. 2010. 35: 332-41
20. Vialle R, Lepeintre JF, Tadié M. The thoracoabdominal intercostal nerves: An anatomical study for their use in neurotization. Surg Radiol Anat. 2005. 27: 8-14
21. Wahegaonkar AL, Doi K, Hattori Y, Addosooki AI. Technique of intercostal nerve harvest and transfer for various neurotization procedures in brachial plexus injuries. Tech Hand Upper Extrem Surg. 2007. 11: 184-94
22. Wilcox M, Brown H, Johnson K, Sinisi M, Quick TJ. An assessment of fatigability following nerve transfer to reinnervate elbow flexor muscles. Bone Joint J. 2019. 101: 867-71
23. Xiao C, Lao J, Wang T, Zhao X, Liu J, Gu Y. Intercostal nerve transfer to neurotize the musculocutaneous nerve after traumatic brachial plexus avulsion: A comparison of two, three, and four nerve transfers. J Reconstr Microsurg. 2014. 30: 297-304
24. Yang LJ, Chang KW, Chung KC. A systematic review of nerve transfer and nerve repair for the treatment of adult upper brachial plexus injury. Neurosurgery. 2012. 71: 417-29