- Department of Neurosurgery, Carle Illinois College of Medicine, University of Illinois Urbana-Champaign, Champaign,
- Department of Neurosurgery, Carle Illinois College of Medicine, Urbana, Illinois, United States.
Correspondence Address:
Paul M. Arnold, MD Department of Neurosurgery, Carle Foundation Hospital, Champaign, Illinois, United States.
DOI:10.25259/SNI_1252_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anant Naik1, Samantha L. Houser1, Christina M. Moawad1, Ravishankar K. Iyer1, Paul M. Arnold2. Noniatrogenic spinal cord ischemia: A patient level meta-analysis of 125 case reports and series. 03-Jun-2022;13:228
How to cite this URL: Anant Naik1, Samantha L. Houser1, Christina M. Moawad1, Ravishankar K. Iyer1, Paul M. Arnold2. Noniatrogenic spinal cord ischemia: A patient level meta-analysis of 125 case reports and series. 03-Jun-2022;13:228. Available from: https://surgicalneurologyint.com/surgicalint-articles/11641/
Abstract
Background: Guidelines are needed to manage spinal cord infarctions. Here, we evaluated the incidence of noniatrogenic spinal ischemia, focusing on the spinal levels involved, and the relative efficacy of different management strategies.
Methods: We performed a meta-analysis of 147 patients who sustained noniatrogenic spinal cord ischemia within the past 10 years. The most common causes of injury were idiopathic (i.e., 47% medical/surgery-related) followed by systemic/chronic conditions (23.6%) and aortic vascular pathology (20%). Postdiagnostic treatment options included rehabilitation in 53.7% of patients, while steroids (35.37%), antiplatelets aggregates (30.61%), and anticoagulation (18.37%) were also used.
Results: Traumatic causes of spinal cord ischemia were associated with worse outcomes, while those without a clear diagnosis despite extensive work-up had better results. At discharge, patients managed with cerebrospinal fluid (CSF) drainage had significant improvement (P = 0.04), while other therapies were not effective. Notably, ischemia mostly occurring between the T4 and T7 levels and was associated with the worst outcomes. In this thoracic “watershed” region, thoracic cord ischemia was most likely attributed to an increased susceptibility toto cord under-perfusion in this region (P
Conclusion: This meta-analysis revealed a variety of etiologies for noniatrogenic typically T4-T7 spinal cord ischemia. Several different treatment strategies may be utilized in this patient population, including CSF drainage, blood pressure elevation, corticosteroids, antiplatelets/anticoagulants/thrombolytics, mannitol, naloxone, surgical revascularization, hyperbaric oxygen, and systemic hypothermia.
Keywords: Cerebrovascular accident, Iatrogenic injury, Spinal infarction, Spinal cord injury, Stroke
INTRODUCTION
The incidence of spinal cord infarction is approximately 0.003%.[
MATERIALS AND METHODS
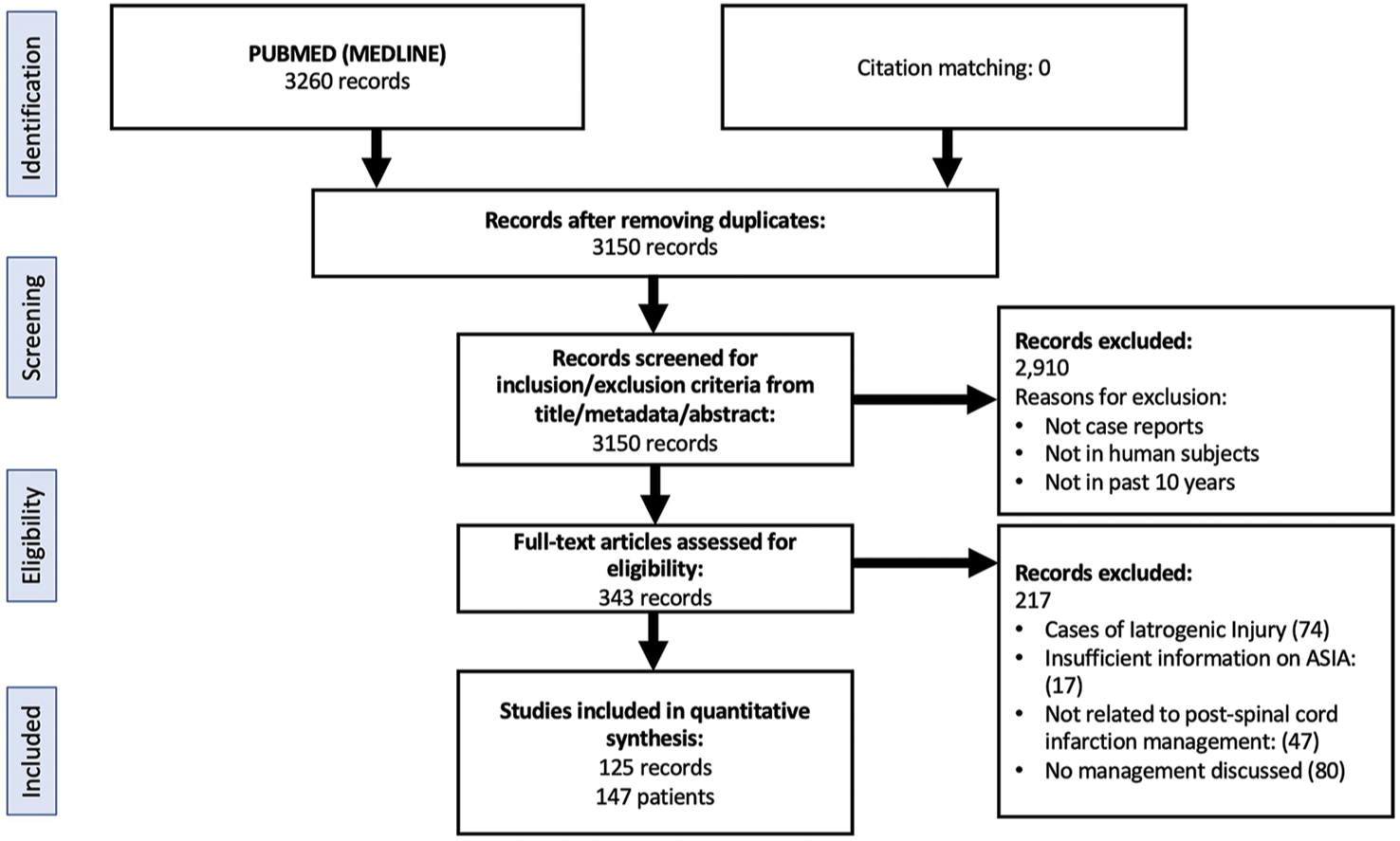
This systematic review was undertaken and reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [
Eligibility criteria and search strategies
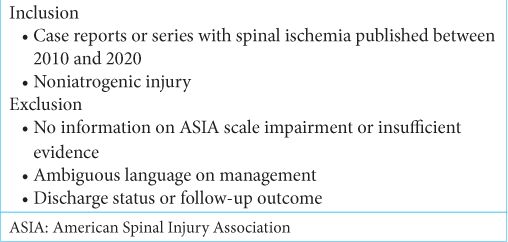
We gathered information on the management of spinal ischemia in 147 patients over the past 10 years. Eligibility criteria were defined before the literature search [
Clinical data
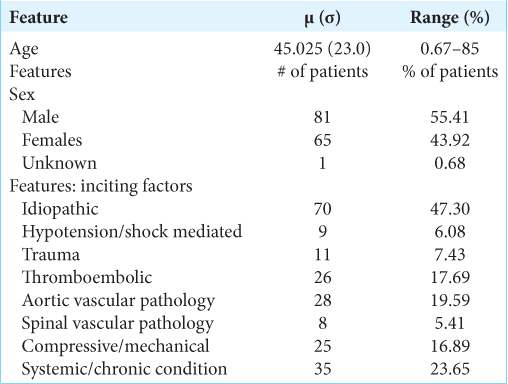
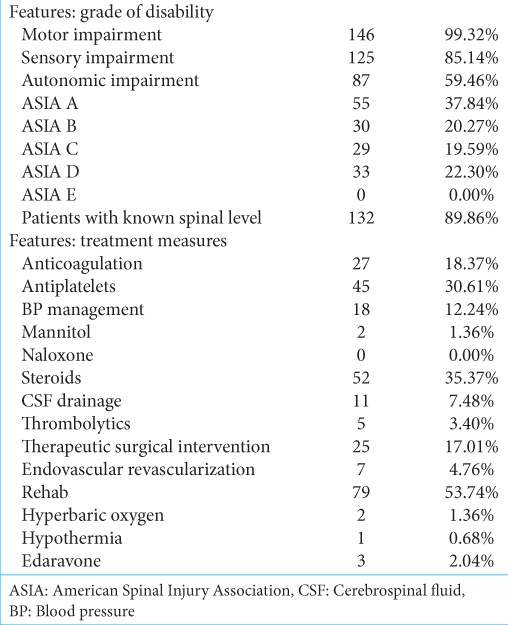
The 147 patients included in this analysis averaged 45 years of age; 55.4% were male. Ischemic SCI injuries were classified as idiopathic (classified because of unknown etiology, 47.3%), 23.6% systemic or chronic conditions (e.g., polycythemia vera), and 19.6% due to aortic/vascular pathology. Noniatrogenic ischemic SCI resulted in the following deficits: motor (146), sensory (125), and autonomic impairment (i.e., 59% including loss of bowel and bladder functional). The American Spinal Injury Association (ASIA) scores were used to classify most patients’ neurological function following noniatrogenic iSCI and included; A – (37.8%), D – (22.3%); with A- and B-level impairment being critical (58%), while B- and C-level impairment was subcritical (42%) [
Summary measures and statistical analysis
Data analysis was performed using GraphPad Prism 9.0 (GraphPad Software, Inc., San Diego, CA) and MATLAB 2020b (MathWorks, Inc., Natick, MA) software. We also used Fisher’s exact test or Chi-goodness-of-fit test, odds ratios, the Haldane-Anscombe correction, and the Cochran-Mantel-Haenszel test which were utilized.
RESULTS
Therapeutic management of infarctions
Following the PRISMA guidelines, we utilized 125 records, involving a total of 147 total patients, sustaining noniatrogenic spinal cord ischemic injuries [
Outcomes
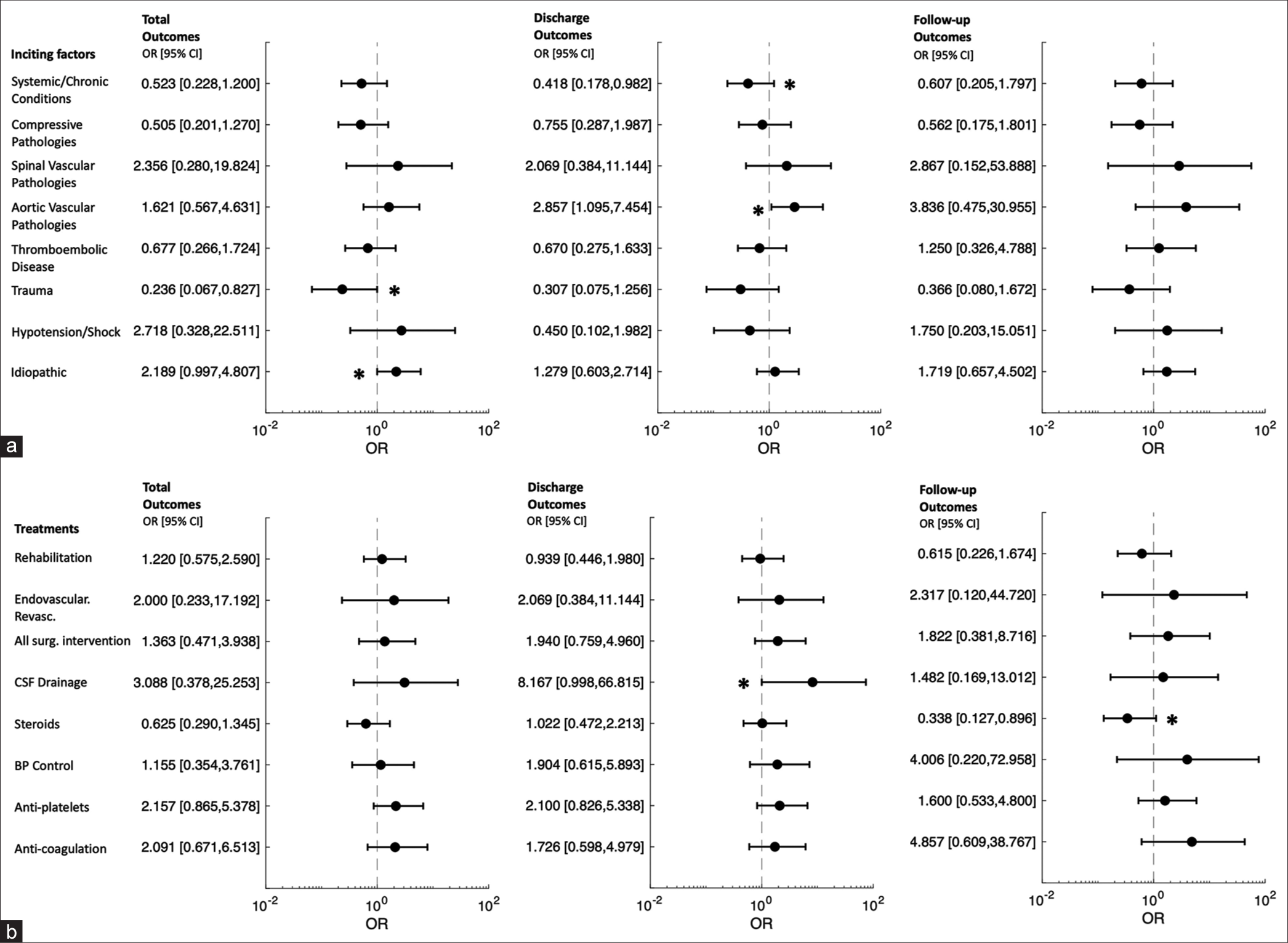
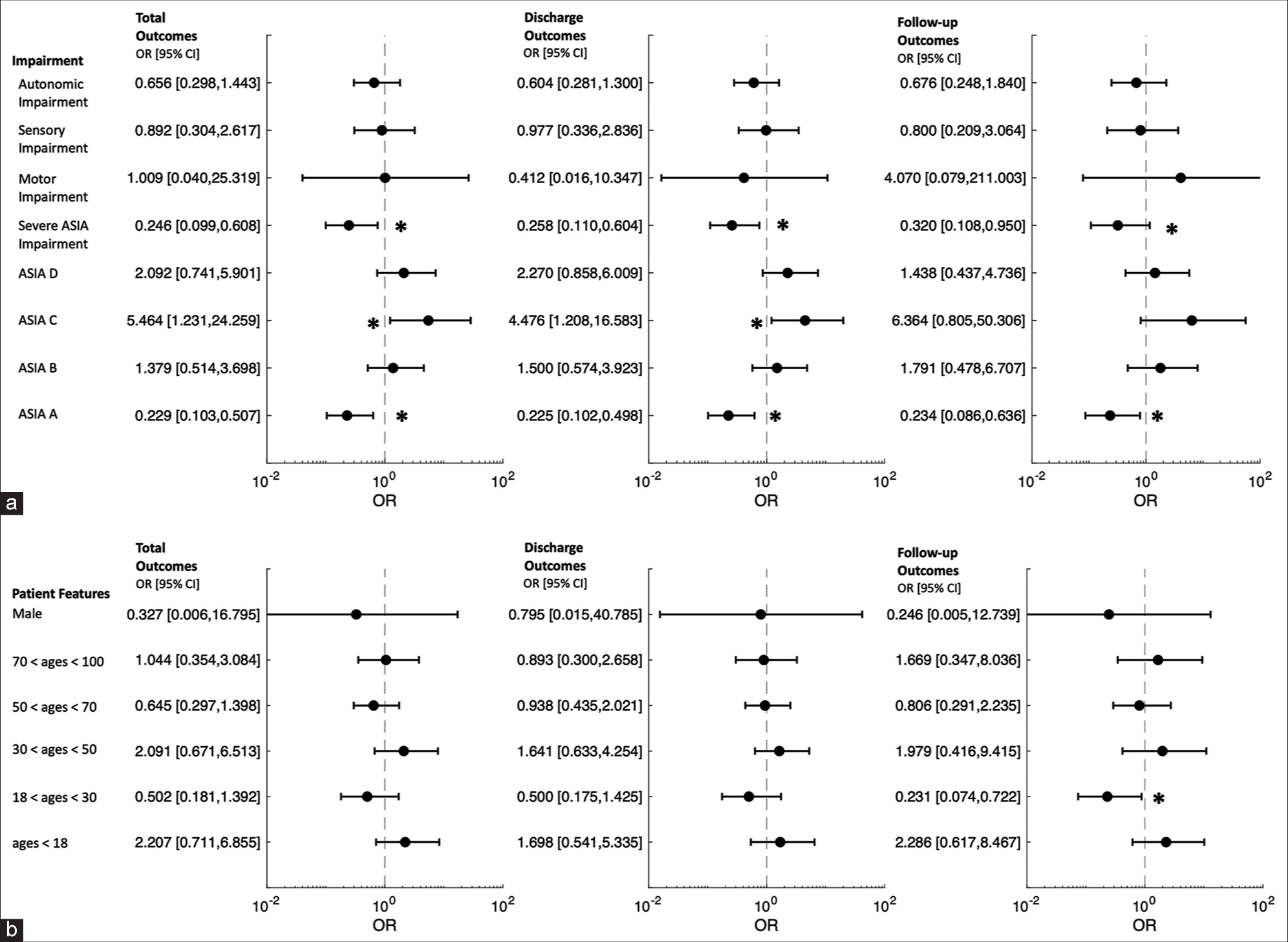
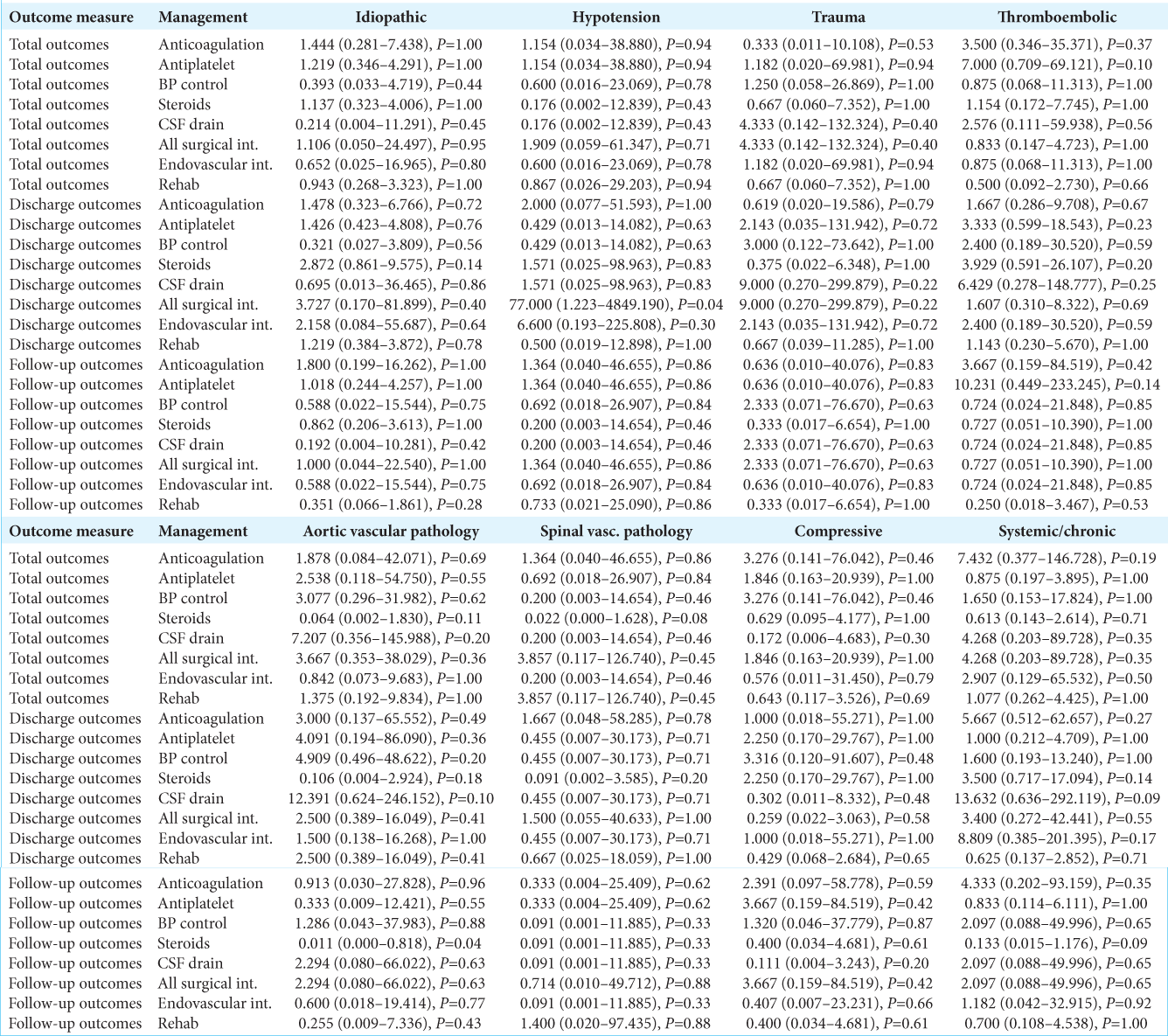
Of the 147 patients’ outcomes that were analyzed those with spinal cord ischemia due to trauma or systemic/chronic causes had poor overall outcomes, while those presenting with idiopathic causes or aortic vascular pathologies had improved outcomes [
Associations with location of infarctions
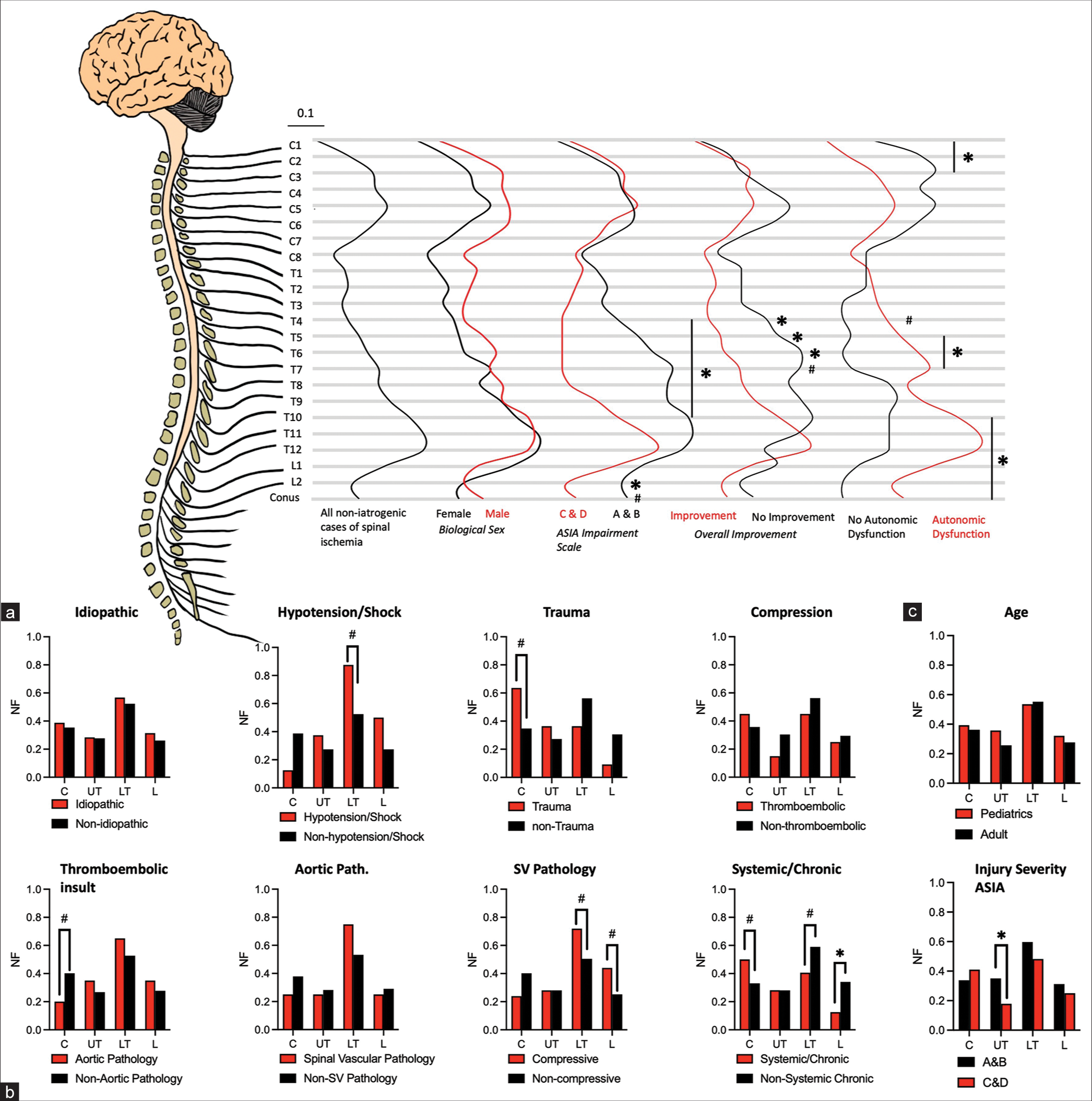
The level of ischemic cord injury correlated with the level of spinal infarction [
Figure 4:
Association with location of injury with outcomes. (a) Association of location with normalized frequency of patient demographics. (b) Association of location by etiology of injury and (c) age and injury severity. Significance determined by P < 0.05 and denoted by asterisk (*). Trend toward significance determined by P < 0.10 and denoted by (#).
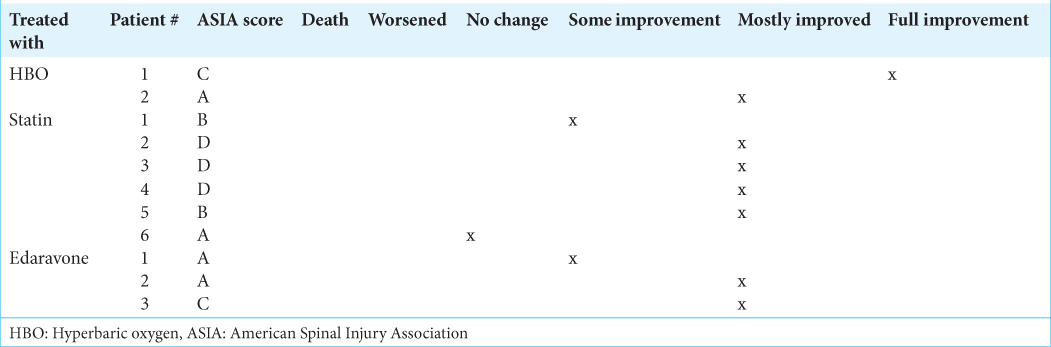
Emerging therapeutics
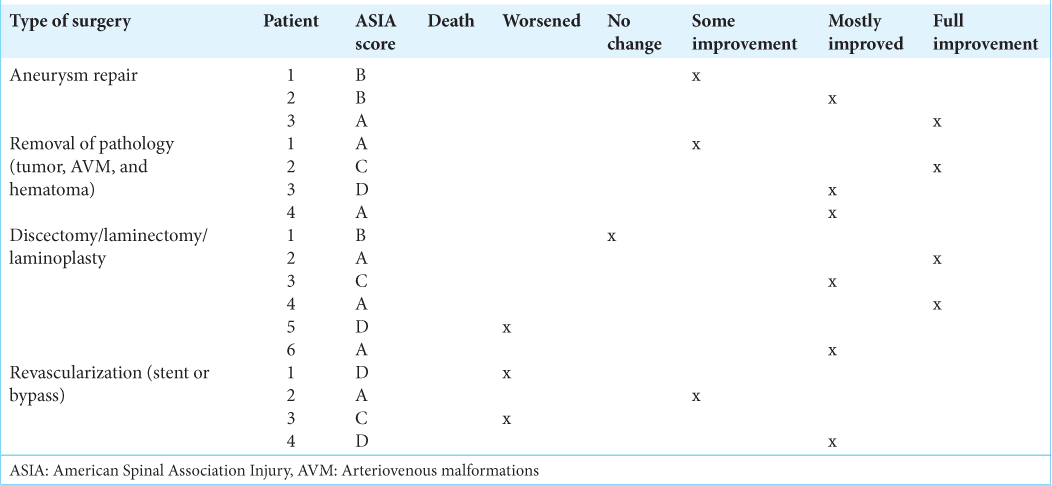
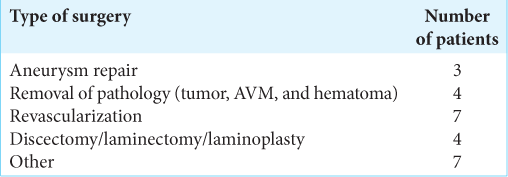
Emerging therapies for ischemic SCI included the use of statins, edaravone, and HBO, and selective surgery. Those undergoing aortic aneurysm repair following ischemia and experienced some improvement. However, the four patients were surgically revascularized (i.e., stent or bypass) and demonstrated no significant improvement [
DISCUSSION
Here, we performed a meta-analysis of 125 case reports involving 147 patients to evaluate the incidence of noniatrogenic spinal cord ischemia, focusing on causes, treatment, and outcomes.[
CONCLUSION
Based on a meta-analysis of 147 patients, effective strategies for treating noniatrogenic spinal cord injury included predominantly CSF drainage and antiplatelet aggregate therapy and, while other treatment options (i.e., steroid usage, HBO, and edaravone) were less effective.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
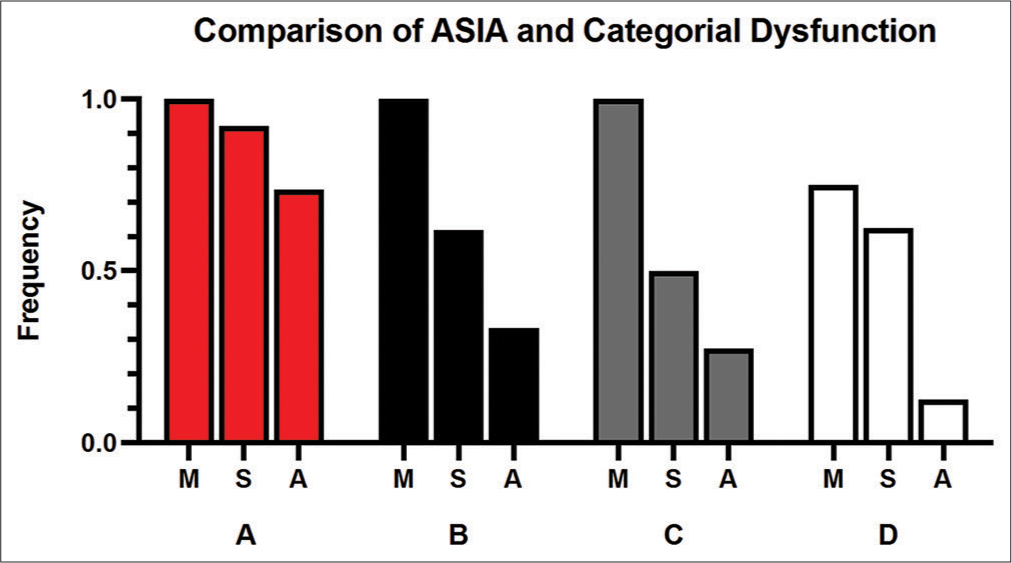
SUPPLEMENTAL FIGURE
Supplemental Figure 1:
A comparison of ASIA impairment to the categorical dysfunction. Motor (M), sensory (S), autonomic (A), dysfunction compared to ASIA-A through ASIA-D. Autonomic dysfunction is present most frequently in ASIA-A impairment. Sensory impairment is also present most frequently in ASIA-A. About 70% of ASIA-A have motor, sensory, and autonomic impairment.
SUPPLEMENTAL TABLES
References
1. Brown J, Usmani B, Arnaoutakis G, Serna-Gallegos D, Plestis K, Shah S. 10-year trends in aortic dissection: Mortality and weekend effect within the US nationwide emergency department sample (NEDS). Heart Surg Forum. 2021. 24: E336-44
2. Chiu P, Miller DC. Evolution of surgical therapy for Stanford acute Type A aortic dissection. Ann Cardiothorac Surg. 2016. 5: 275-95
3. Choi JU, Hoffman HJ, Hendrick EB, Humphreys RP, Keith WS. Traumatic infarction of the spinal cord in children. J Neurosurg. 1986. 65: 608-10
4. Dong J, Wang F, Sundararajan S. Use of dual antiplatelet therapy following ischemic stroke. Stroke. 2020. 51: 79-80
5. Francis K. Physiology and management of bladder and bowel continence following spinal cord injury. Ostomy Wound Manage. 2007. 53: 18-27
6. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009. 339: b2700
7. Pikija S, Mutzenbach JS, Kunz AB, Nardone R, Leis S, Deak I. Delayed Hospital Presentation and Neuroimaging in Non-surgical Spinal Cord Infarction. Front Neurol. 2017. 8: 143
8. Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American spinal injury association (ASIA) impairment scale. Clin Orthop Relat Res. 2017. 475: 1499-504
9. Robertson CE, Brown RD, Wijdicks EF, Rabinstein AA. Recovery after spinal cord infarcts: Long-term outcome in 115 patients. Neurology. 2012. 78: 114-21
10. Salvador de la Barrera S, Barca-Buyo A, Montoto-Marqués A. Spinal cord infarction: prognosis and recovery in a series of 36 patients. Spinal Cord. 2001. 39: 520-525
11. Sandercock PA, Counsell C, Tseng MC, Cecconi E. Oral antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev. 2014. 2014: CD000029
12. Yadav N, Pendharkar H, Kulkarni GB. Spinal cord infarction: Clinical and radiological features. J Stroke Cerebrovasc Dis. 2018. 27: 2810-821
13. Zalewski NL, Rabinstein AA, Krecke KN, Brown RD, Wijdicks EF, Weinshenker BG. Characteristics of spontaneous spinal cord infarction and proposed diagnostic criteria. JAMA Neurol. 2019. 76: 56-63