- Department of Neurosurgery, The Royal Melbourne Hospital, VIC 3050, Australia
Correspondence Address:
Shaun Previn Appaduray
Department of Neurosurgery, The Royal Melbourne Hospital, VIC 3050, Australia
DOI:10.4103/2152-7806.166801
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Appaduray SP, Lo P. Nonoperative management of craniovertebral junction and cutaneous tuberculosis. Surg Neurol Int 06-Oct-2015;6:157
How to cite this URL: Appaduray SP, Lo P. Nonoperative management of craniovertebral junction and cutaneous tuberculosis. Surg Neurol Int 06-Oct-2015;6:157. Available from: http://surgicalneurologyint.com/surgicalint_articles/nonoperative-management-of-craniovertebral-junction-and/
Abstract
Background:Craniovertebral junction (CVJ) and cutaneous tuberculosis (TB) are both rare, each occurring in 0.3-1.0% of patients. To our knowledge, there are no existing cases reporting these manifestations of TB simultaneously. We report a case of TB involving the left CVJ as well as the skin, and discuss our management while providing a review of the literature.
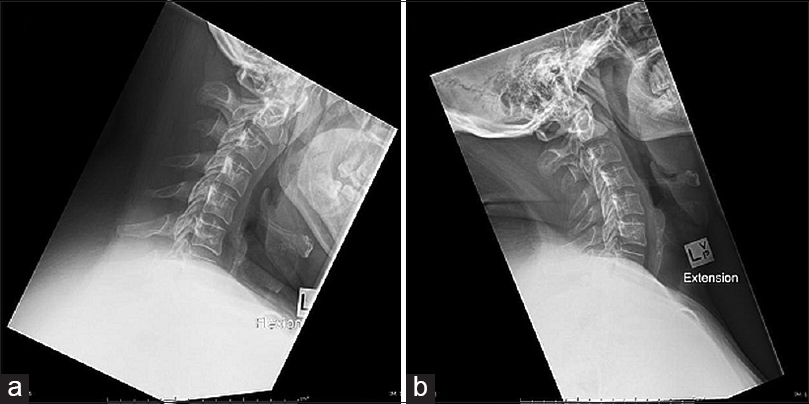
Case Description:An adult patient was presented with progressive nocturnal neck pain associated with the development of several skin lesions. Investigations revealed multiple osseous lesions including the left CVJ. Biopsy of the CVJ lesion was unamenable due to proximity of the vertebral artery; therefore, the patient underwent biopsy of the other sites. Histological examination demonstrated features consistent with TB infection and the patient commenced 12 months of standard anti-TB therapy with cervical spine immobilization. At 2-month review, the patient was well with a near-complete resolution of neck pain and cutaneous lesions. Repeat imaging at 6 months follow-up demonstrated a stable C1 lesion with no evidence of instability.
Conclusion:CVJ TB may be treated solely with anti-TB therapy and immobilization to good effect if there is no gross instability or neurological deficit. Similarly, cutaneous TB responds well to standard anti- TB therapy. Our experience suggests that co-existing tuberculous lesions in the CVJ and skin can be simultaneously managed with standard therapy without significant alterations to treatment regimes or prognosis.
Keywords: Craniovertebral junction, cutaneous tuberculosis, spinal, tuberculosis
INTRODUCTION
Craniovertebral junction (CVJ) tuberculosis (TB) is, especially uncommon and accounts for 0.3–1.0% of spinal TB, as illustrated in a review by Gupta et al. which found only 51 cases of CVJ TB from 1978 to 2004.[
CASE REPORT
A 31-year-old male of Indian extraction was presented with a 2-month history of progressive nocturnal neck pain and 8 months of multiple skin lesions, but no neurological deficit. He had visited India 12 months previously and had received routine bacillus Calmette–Guérin vaccinations before immigrating to Australia at 21 years of age.
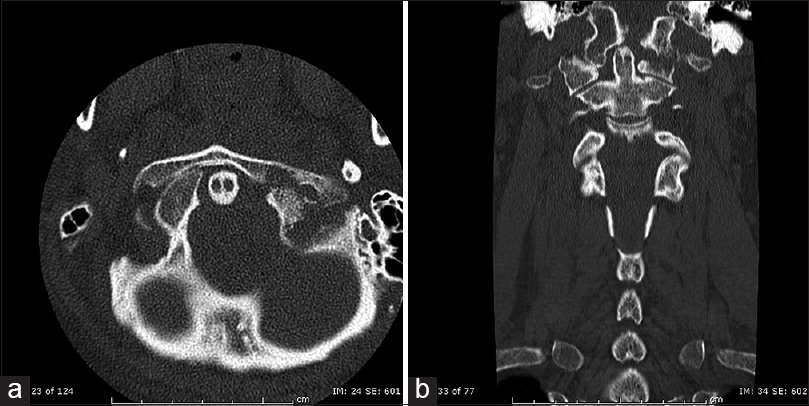
Skin examination revealed; a 4.5 cm solid mass overlying the right deltoid, a 1.5 cm mobile mass on the left chin, and a 1.5 cm mobile mass on the dorsum of the left foot. Although he had a positive QuantiFERON Gold assay (titer 11.68 IU/ml), his chest X-ray was normal. Cervical computerized tomography (CT) showed destructive bony changes at the left atlanto-occipital junction (between the left occipital condyle and superior articular facet of the left lateral mass of C1); there was a soft tissue mass between these plus left-sided lateral subluxation of C1–C2 [Figures
Figure 2
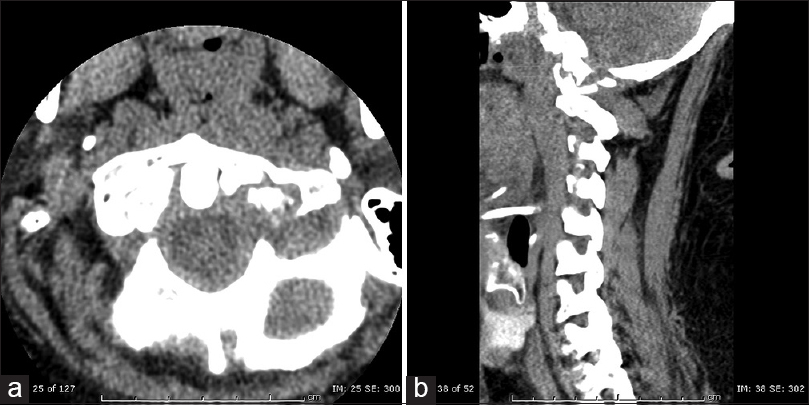
(a) Axial and (b) Sagittal cervical spine computerized tomography with bony changes as described in
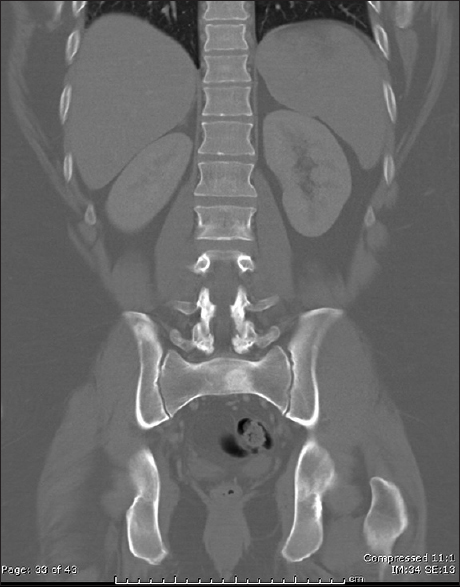
He was immobilized in a halo vest. A CT of the chest, abdomen, and pelvis showed lytic and sclerotic bony lesions in the ribs, pelvis, sacrum, and right acromion [
DISCUSSION
Craniovertebral junction tuberculosis
CVJ TB predominantly affects the anterior structures of the vertebrae. The infection destroys bony and ligamentous structures, resulting in neuraxial compression and instability.[
Treatment options for CVJ TB are controversial due to the absence of well-established guidelines.[
Cutaneous tuberculosis
Cutaneous TB is reported in <1% of cases.[
Case discussion
The site of the lesion was impacted upon our management decisions. Biopsy was unamenable due to the risk of damaging the adjacent vertebral artery and its associated sequelae. The cutaneous lesions in this case were multifocal, solid subcutaneous nodules with no evidence of exudation. This was consistent with the typical features of lupus vulgaris. As there was no overt instability or compression, we elected for biopsy of the other osseous sites as well as the cutaneous lesions and commenced ATT for treatment. These biopsies indeed demonstrated PCR findings consistent with TB and eventually produced a positive culture.
The long-term outcome of nonoperative management of both CVJ and cutaneous TB is excellent.[
In summary, we present a manifestation of extrapulmonary TB presenting with CVJ and cutaneous lesions, both of which are rare occurrences. We concur with the findings in the literature that CVJ TB can be managed nonoperatively, particularly in the absence of cervical instability or neurological deficit.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arora S, Sabat D, Maini L, Sural S, Kumar V, Gautam VK. The results of nonoperative treatment of craniovertebral junction tuberculosis: A review of twenty-six cases. J Bone Joint Surg Am. 2011. 93: 540-7
2. Banashankari GS, Rudresh HK, Harsha AH, Bharathi R, Kamble P. An unusual presentation of cutaneous tuberculosis for surgeons-review of literature. Indian J Surg. 2012. 74: 314-7
3. Chadha M, Agarwal A, Singh AP. Craniovertebral tuberculosis: A retrospective review of 13 cases managed conservatively. Spine (Phila Pa 1976). 2007. 32: 1629-34
4. Dhammi IK, Singh S, Jain AK. Hemiplegic/monoplegic presentation of cervical spine (C1-C2) tuberculosis. Eur Spine J. 2001. 10: 540-4
5. du Plessis J, Andronikou S, Theron S, Wieselthaler N, Hayes M. Unusual forms of spinal tuberculosis. Childs Nerv Syst. 2008. 24: 453-7
6. Edwards RJ, David KM, Crockard HA. Management of tuberculomas of the craniovertebral junction. Br J Neurosurg. 2000. 14: 19-22
7. Fang D, Leong JC, Fang HS. Tuberculosis of the upper cervical spine. J Bone Joint Surg Br. 1983. 65: 47-50
8. Frankel A, Penrose C, Emer J. Cutaneous tuberculosis: A practical case report and review for the dermatologist. J Clin Aesthet Dermatol. 2009. 2: 19-27
9. Gupta SK, Mohindra S, Sharma BS, Gupta R, Chhabra R, Mukherjee KK. Tuberculosis of the craniovertebral junction: Is surgery necessary?. Neurosurgery. 2006. 58: 1144-50
10. Kotil K, Dalbayrak S, Alan S. Craniovertebral junction Pott's disease. Br J Neurosurg. 2004. 18: 49-55
11. Krishnan A, Patkar D, Patankar T, Shah J, Prasad S, Bunting T. Craniovertebral junction tuberculosis: A review of 29 cases. J Comput Assist Tomogr. 2001. 25: 171-6
12. Lee DK, Cho KT, Im SH, Hong SK. Craniovertebral junction tuberculosis with atlantoaxial dislocation: A case report and review of the literature. J Korean Neurosurg Soc. 2007. 42: 406-9
13. Lifeso R. Atlanto-axial tuberculosis in adults. J Bone Joint Surg Br. 1987. 69: 183-7
14. Qureshi MA, Afzal W, Khalique AB, Pasha IF, Aebi M. Tuberculosis of the craniovertebral junction. Eur Spine J. 2013. 22: 612-7
15. Ramesh V, Sen MK, Nair D, Singla R, Sengupta A. Cutaneous tuberculosis caused by multidrug-resistant tubercle bacilli: Report of three cases. Int J Dermatol. 2011. 50: 300-3
16. Sadek AR, Wallage W, Jaiganesh T. Cervical spine tuberculosis causing instability and neurological compromise. JRSM Short Rep. 2011. 2: 47-
17. Turgut M. Multifocal extensive spinal tuberculosis (Pott's disease) involving cervical, thoracic and lumbar vertebrae. Br J Neurosurg. 2001. 15: 142-6
18. Yates VM, Ormerod LP. Cutaneous tuberculosis in Blackburn district (U.K.): A 15-year prospective series, 1981-95. Br J Dermatol. 1997. 136: 483-9