- Department of Neurosurgery, Nakagami Hospital, Okinawa, Japan
- Uchikado Neuro-Spine Clinic, Fukuoka, Japan
- Department of Neurosurgery, Kurume University School of Medicine, Fukuoka, Japan
Correspondence Address:
Naohisa Miyagi
Department of Neurosurgery, Kurume University School of Medicine, Fukuoka, Japan
DOI:10.4103/2152-7806.157303
Copyright: © 2015 Miyagi N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Miyagi N, Uchikado H, Aoki T, Sakata K, Hirohata M, Morioka M. Nontraumatic aneurysm rupture following an endoscopic third ventriculostomy and ventricular drainage: Case report of a rare complication. Surg Neurol Int 19-May-2015;6:80
How to cite this URL: Miyagi N, Uchikado H, Aoki T, Sakata K, Hirohata M, Morioka M. Nontraumatic aneurysm rupture following an endoscopic third ventriculostomy and ventricular drainage: Case report of a rare complication. Surg Neurol Int 19-May-2015;6:80. Available from: http://surgicalneurologyint.com/surgicalint_articles/nontraumatic-aneurysm-rupture-following-endoscopic-third/
Abstract
Background:Although endoscopic third ventriculostomy is a safe procedure, the authors report a case of aneurysmal subarachnoid hemorrhage as an unusual and serious complication of an endoscopic third ventriculostomy and ventricular drainage.
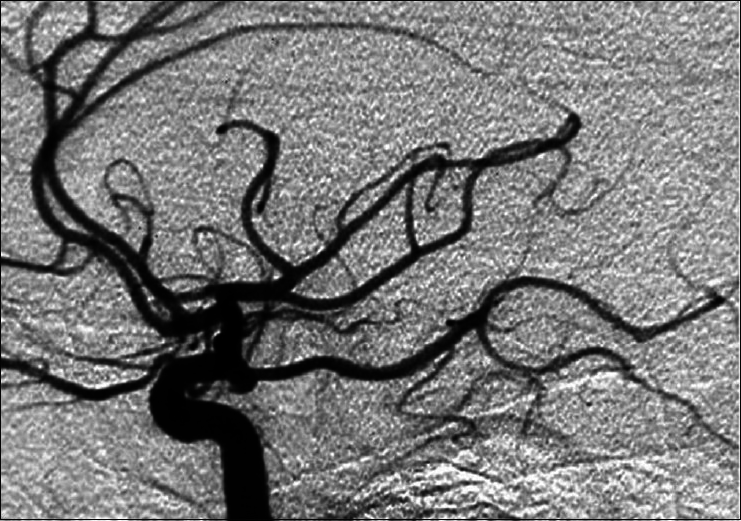
Case Description:A 60-year-old male presented with obstructive hydrocephalus caused by midbrain tumors was admitted to our hospital. Endoscopic third ventriculostomy and external ventricular drainage were successfully performed. Two days after the operation, he became comatose, and a computed tomography (CT) scan revealed a diffuse subarachnoid hemorrhage. Emergency cerebral angiogram showed an aneurysm of the left internal carotid artery. Endovascular coil embolization of the ruptured aneurysm was then performed.
Conclusion:The rupture of the aneurysm may have been induced by excessive cerebrospinal fluid drainage after the endoscopic third ventriculostomy. Planning for intracranial endoscopic procedures should consider that rupture of an unknown previously unruptured aneurysm is a possible complication.
Keywords: Complication, endoscopic third ventriculostomy, obstructive hydrocephalus, subarachnoid hemorrhage, ventricular drainage
INTRODUCTION
Endoscopic third ventriculostomy (ETV) is a well-established procedure for treating various forms of noncommunicating hydrocephalus.[
CASE REPORT
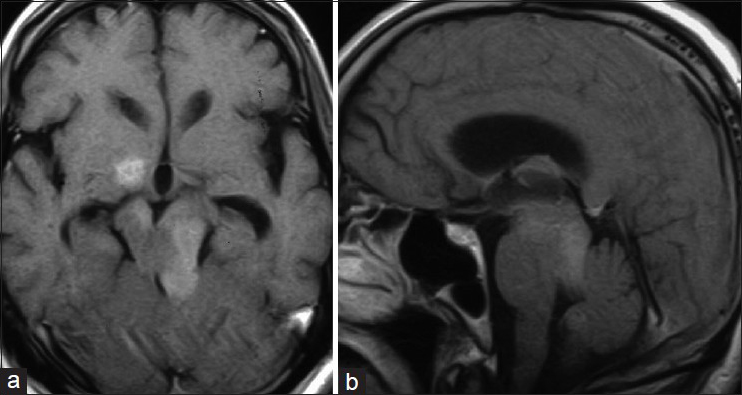
A 60-year-old male presented with slowly progressive drowsiness was admitted to our hospital. Magnetic resonance imaging (MRI) revealed an obstructive hydrocephalus caused by midbrain tumors [Figure
Operation
The operating sheath was inserted into the right lateral ventricle through a right-sided coronal burr hole. The endoscope was advanced into the third ventricle through the sheath and the foramen of Monro. The floor of the third ventricle was thin and translucent. Under continuous visual control, the biopsy forceps and a 4-French Fogarty balloon catheter were used to perforate and widen the stoma. The basilar tip and bilateral posterior cerebral artery were visible below the stoma, but there was no injury to these arteries. A biopsy was not performed because the tumor did not appear on the surface of the ventricle, but cerebrospinal fluid (CSF) cytology revealed malignant lymphoma cells. After some minutes of irrigation, no bleeding was confirmed, and external ventricular drainage was then inserted into the right lateral ventricle.
Postoperative course
The patient was in our intensive care unit with continuous monitoring of heart rate and blood pressure. His systolic blood pressure was stable in the range of 130–110 mmHg. He was drowsy, but did not exhibit confusion or other signs of significant pain. After the procedure, the initial level of ventricular drainage was 10 cm H2O. About 220 ml of CSF was drained in the first day after surgery. The patient remained drowsy, but a computed tomography (CT) scan the day after the operation showed no abnormal findings except dilated lateral ventricles. The CSF continued to drain. Two days after the operation, we set the level of ventricular drainage to be the same as that on the first day. About 300 ml of CSF was gradually drained with about 16 h before the bleeding began. The patient suddenly became comatose, and the bloody CSF was rapidly drained immediately. An emergency CT scan revealed a diffuse SAH [
DISCUSSION
Although the efficacy and safety of ETV is currently well accepted, several types of traumatic complications have been reported including basilar artery injury, perforation of the anterior cerebral artery branch, massive intraventricular hemorrhage, and contusions of the thalamus and hypothalamus.[
Intraaneurysmal pressure is equal to the systemic blood pressure. Transmural pressure can be defined as the difference between the blood pressure and the intracranial pressure.[
In the present case, we did not perform any preoperative assessment of the cerebrovascular vessels. Wardlaw and White reviewed prospective autopsy and angiographic studies, and indicated that between 3.6% and 6% of the population harbor an unruptured intracranial aneurysm.[
References
1. Abtin K, Thompson BG, Walker ML. Basilar artery perforation as a complication of endoscopic third ventriculostomy. Pediatr Neurosurg. 1998. 28: 35-41
2. Dusick JR, Mc Arthur DL, Bergsneider M. Success and complication rates of endoscopic third ventriculostomy for adult hydrocephalus: A series of 108 patients. Surg Neurol. 2008. 69: 5-15
3. Fountas KN, Kapsalaki EZ, Machinis T, Karampelas I, Smisson HF, Robinson JS. Review of the literature regarding the relationship of rebleeding and external ventricular drainage in patients with subarachnoid hemorrhage of aneurysmal origin. Neurosurg Rev. 2006. 29: 14-8
4. Handa J, Matsuda I, Handa H. Association of brain tumor and intracranial aneurysm. Surg Neurol. 1976. 6: 25-9
5. Hasan D, Vermeulen M, Wijdicks EF. Management problems in acute hydrocephalus after subarachnoid hemorrhage. Stroke. 1989. 20: 747-53
6. Hopf NJ, Grunert P, Fries G, Resch KD, Perneczky A. Endoscopic third ventriculostomy: Outcome analysis of 100 consecutive procedures. Neurosurgery. 1999. 44: 795-806
7. McIver JI, Friedman JA, Wijdicks EF, Piepgras DG, Pichelmann MA, Toussaint LG. Preoperative ventriculostomy and rebleeding after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2002. 97: 1042-4
8. McLaughlin MR, Wahlig JB, Kaufmann AM, Albright AL. Traumatic basilar aneurysm after endoscopic third ventriculostomy: Case report. Neurosurgery. 1997. 41: 1400-4
9. Pare L, Delfino R, Leblanc R. The relationship of ventricular drainage to aneurysmal rebleeding. J Neurosurg. 1992. 76: 422-7
10. Rezende MT, Spelle L, Piotin M, Mounayer C, Lucas Cde P, Abud DG. Selective endovascular treatment of a traumatic basilar aneurysm after endoscopic third ventriculostomy. Neuroradiology. 2008. 50: 443-6
11. Schroeder HW, Niendorf WR, Gaab MR. Complications of endoscopic third ventriculostomy. J Neurosurg. 2002. 96: 1032-40
12. Stefini R, Ghitti F, Bergomi R, Catenacci E, Latronico N, Mortini P. Uncommon presentation of ruptured intracranial aneurysm during surgical evacuation of chronic subdural hematoma: Case report. Surg Neurol. 2008. 69: 89-92
13. Taylor PE. Delayed postoperative hemorrhage from intracranial aneurysm after craniotomy for tumor. Neurology. 1961. 11: 225-31
14. Wardlaw JM, White PM. The detection and management of unruptured intracranial aneurysms. Brain. 2000. 123: 205-21