- Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma,
- Department of Neurosurgery, University of Arizona College of Medicine, Phoenix, Arizona,
- Department of Neurological Surgery, Northwestern Medicine, Lavin Family Pavilion, Chicago, Illinois, United States.
Correspondence Address:
Zachary A. Smith, Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, United States.
DOI:10.25259/SNI_936_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Xiaochun Zhao1, Kiana Y. Prather1, José M. Orenday-Barraza2, Fauziyya Y. Muhammad1, Lance M. Villeneuve1, María José Cavagnaro2, Ali A. Baaj2, Nader S. Dahdaleh3, Zachary A. Smith1. Nontraumatic atlantoaxial rotatory subluxation in adults: Report of two cases. 23-Dec-2022;13:589
How to cite this URL: Xiaochun Zhao1, Kiana Y. Prather1, José M. Orenday-Barraza2, Fauziyya Y. Muhammad1, Lance M. Villeneuve1, María José Cavagnaro2, Ali A. Baaj2, Nader S. Dahdaleh3, Zachary A. Smith1. Nontraumatic atlantoaxial rotatory subluxation in adults: Report of two cases. 23-Dec-2022;13:589. Available from: https://surgicalneurologyint.com/surgicalint-articles/12074/
Abstract
Background: Nontraumatic infectious atlantoaxial rotatory subluxation (AARS) is rare and less frequently encountered in adults versus children. We utilized a stepwise approach to treat two adults with nontraumatic infectious AARS and summarized the relevant literature.
Case Description: Two patients, ages 35 and 66, presented with classic clinical and imaging findings for infectious nontraumatic AARS. Here, we summarized the management for these two patients along with the literature.
Conclusion: Nontraumatic infectious AARS in adults requires prompt X-ray diagnosis and timely application of traction to minimize neurological deficits. MR/CT imaging next offers critical information regarding whether operative stabilization is warranted.
Keywords: Atlantoaxial, Cock-robin, Grisel syndrome, Nontraumatic, Subluxation
INTRODUCTION
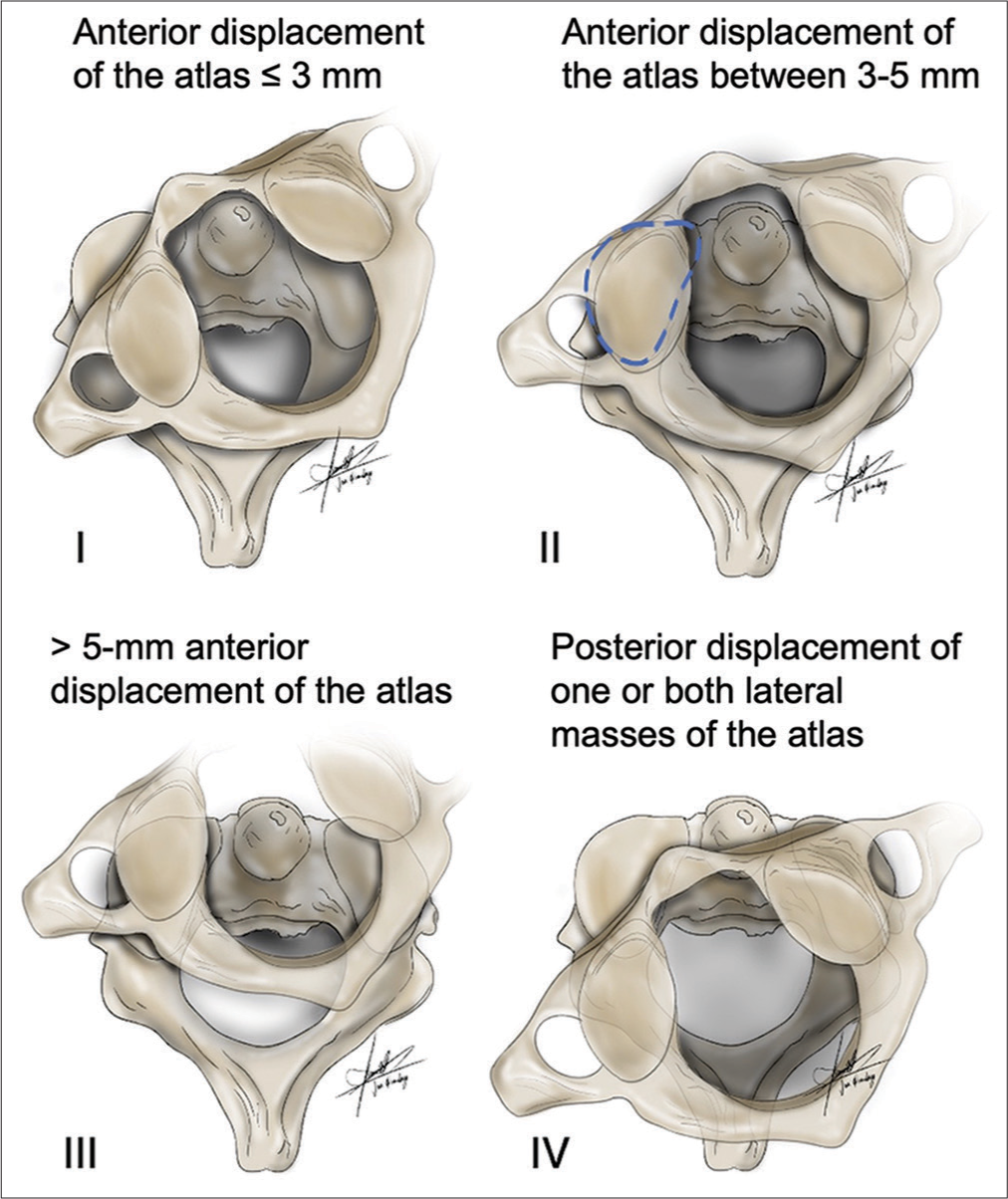
Nontraumatic atlantoaxial rotatory subluxation (AARS) associated with an infectious or inflammatory etiology is often managed conservatively with traction or bracing. It is mostly seen in the pediatric age group. The severity of subluxation is usually based on the Fielding and Hawkins classification system [
CASE DESCRIPTION
Case 1
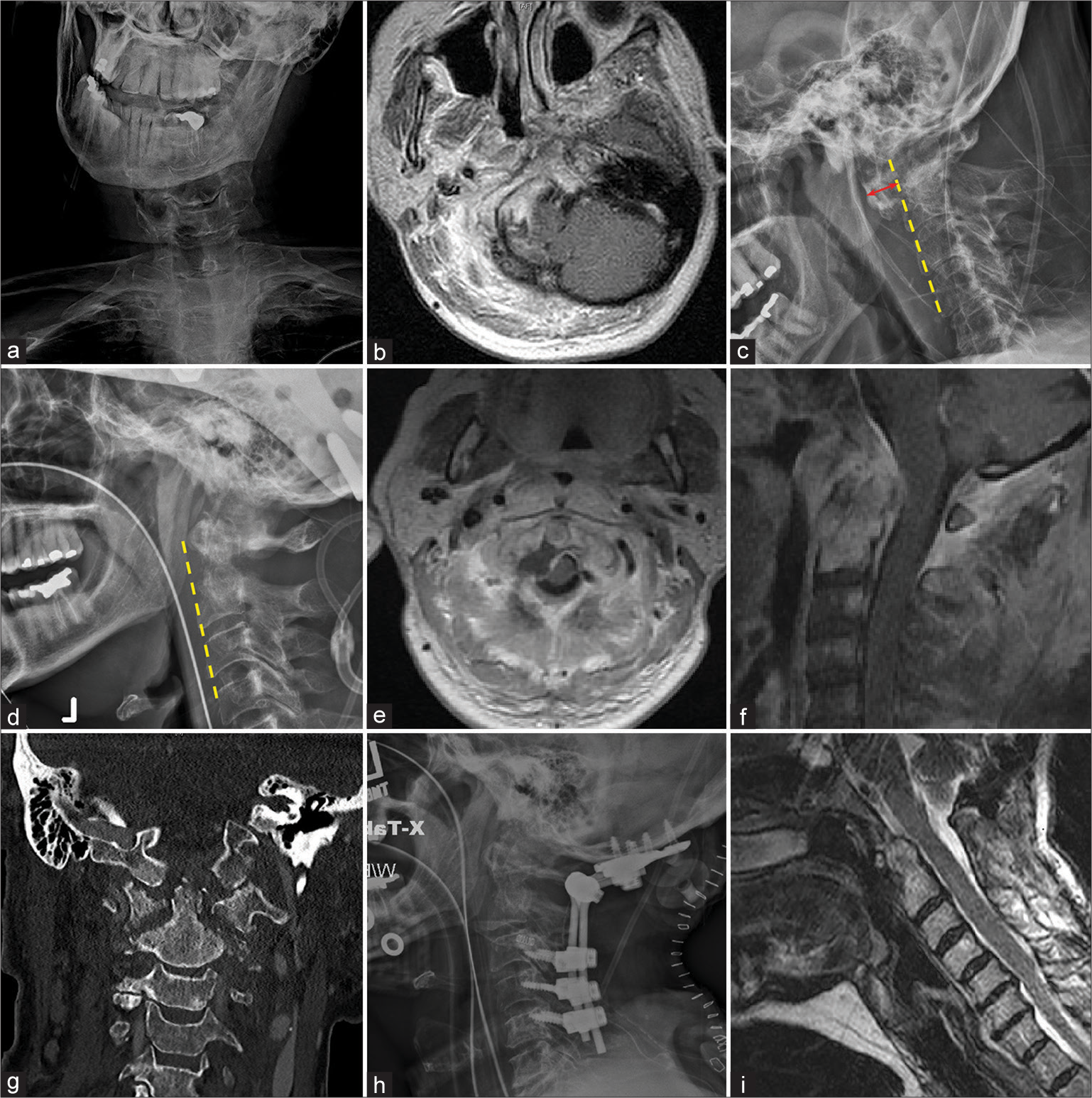
A 66-year-old female presented with 2 months of dysphagia, neck pain, dysarthric speech, and severe torticollis with the classic “cock-robin” position for several weeks’ duration [
Figure 2:
Case 1: X-ray of the neck demonstrating cock-robin position (a); T1 magnetic resonance imaging (MRI) of suboptimal quality due to neck tilt (b); lateral X-ray of the craniocervical junction showing increased atlanto-dental interval marked by the red arrow (c); post traction imaging demonstrating complete reduction on lateral X-ray (d) with extensive inflammation seen on axial (e) and sagittal (f) T1 MRI and coronal computed tomography (g) of the cervical spine; postoperative lateral neck X-ray (h); and sagittal T2 MRI (i) demonstrating proper instrumentation and alignment. Yellow dashed line indicates anterior alignment of the cervical spine.
Case 2
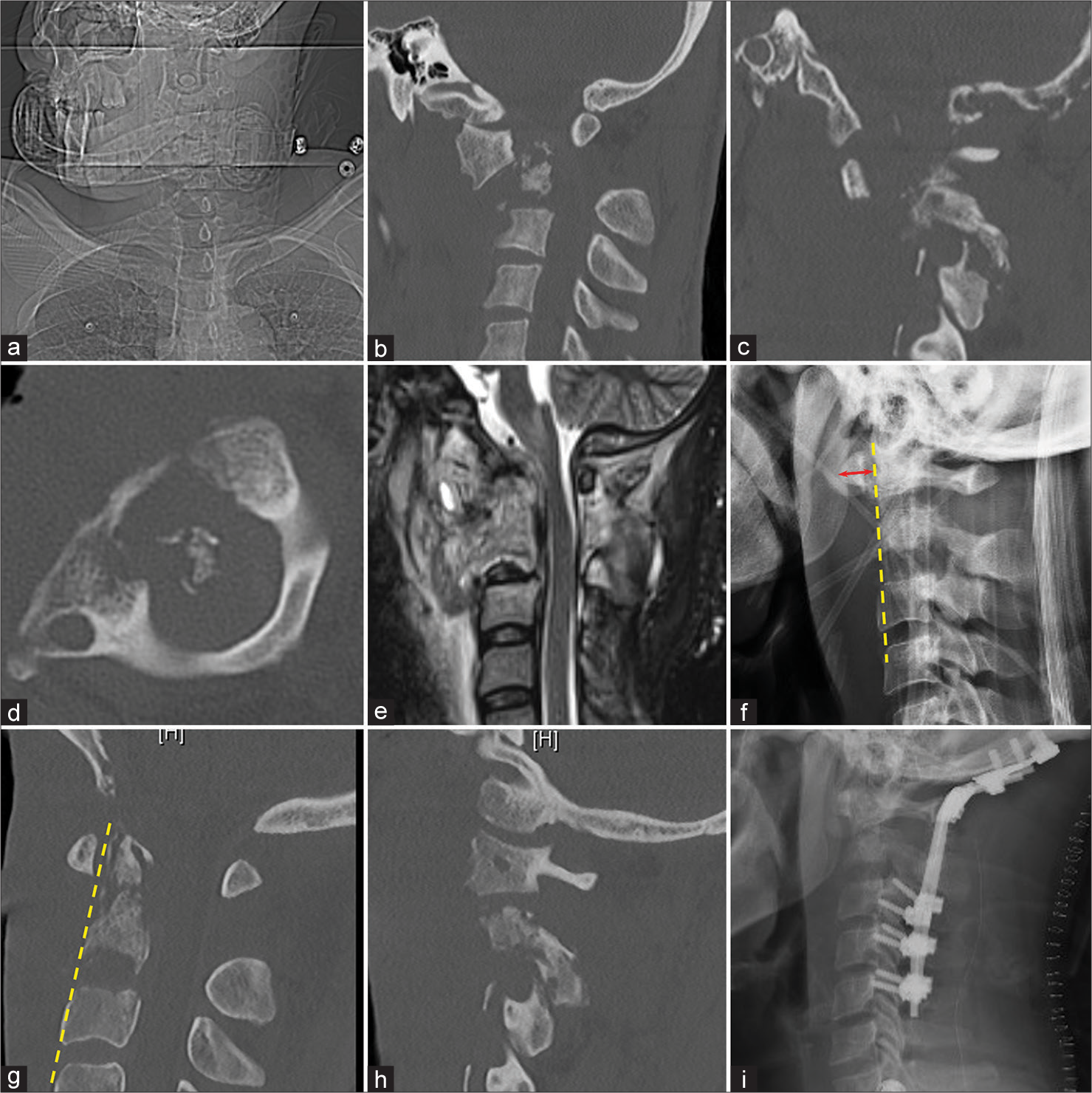
A 35-year-old male with a history of intravenous drug abuse presented with 1 week of fevers, upper neck pain and progressive dysphonia, dysphagia, and quadriparesis (1/5 upper and 3/5 lower extremities with high cervical pin level). On examination, his neck was locked in the “cock-robin” position [
Figure 3:
Case 2: X-ray of the neck showing cock-robin position (a); computed tomography (CT) of the cervical spine demonstrating anterior C1 subluxation with destruction of the odontoid process (sagittal, b) and facet joint (coronal, c) with rotation seen in the axial plane (d); sagittal T2 magnetic resonance imaging demonstrating inflammatory process involving C1-2 with cord signal change (e); lateral neck X-ray with increased atlanto-dental interval marked by the red arrow (f); post-traction CT showing restoration of alignment at midline (g) and facet joint (h); and postoperative lateral X-ray with proper instrumentation (i). Yellow dashed line indicates anterior alignment of the cervical spine.
DISCUSSION
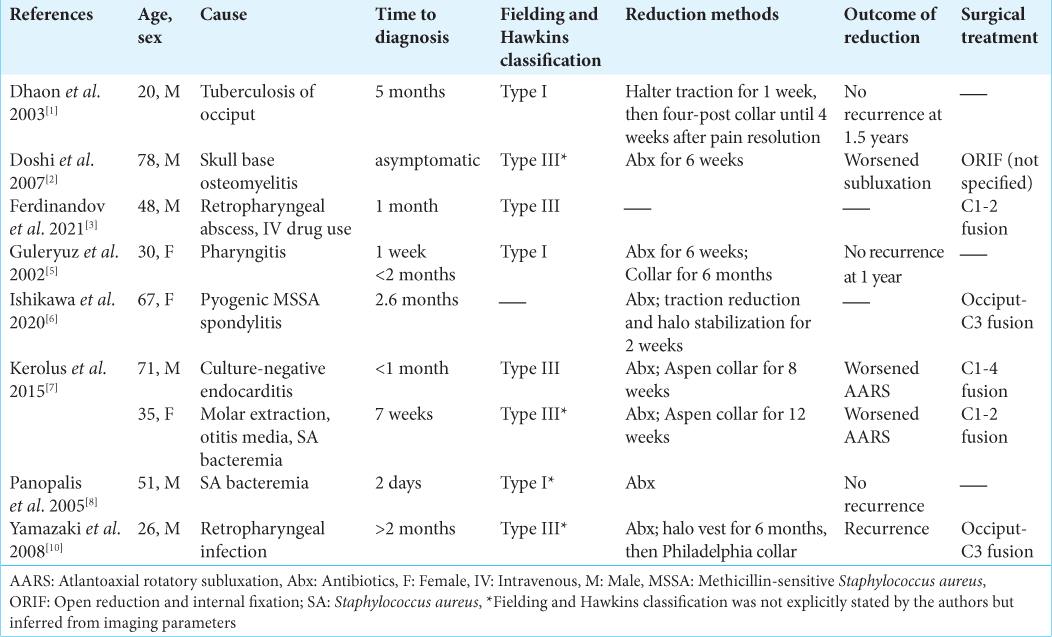
Nontraumatic AARS in adults is usually attributable to infection [
Utility of CT and MR studies for diagnosing AARS
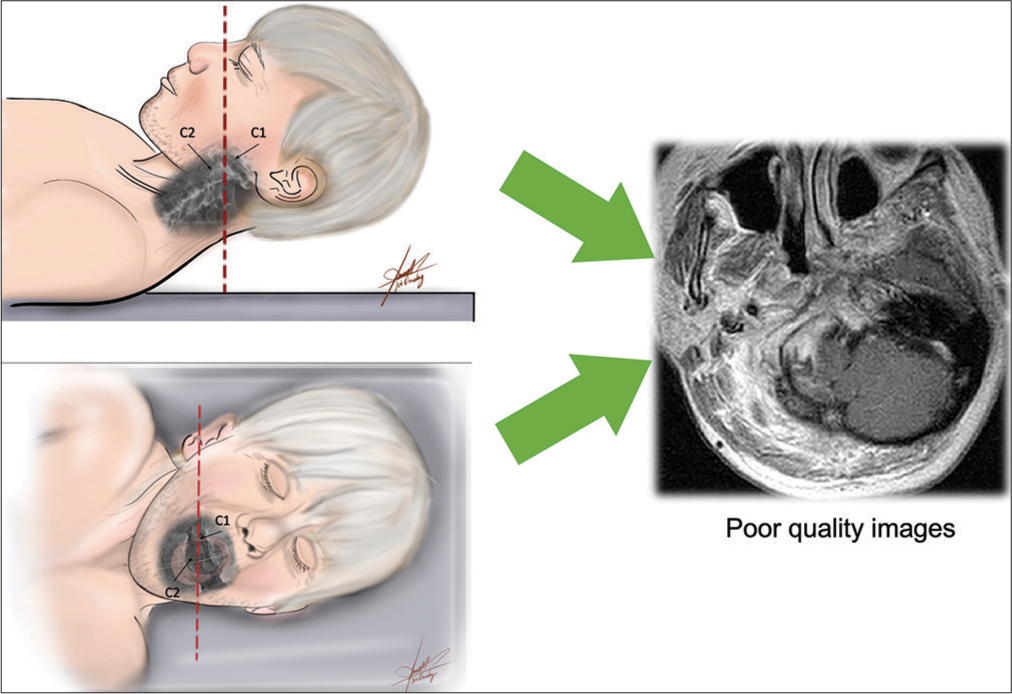
Patients with suspected nontraumatic AARS should undergo CT and MRI to confirm the diagnosis but only following adequate reduction, as placing them flat in the scanner before stabilization is not safe [
Protocol for diagnosing AARS
The diagnosis of AARS should be established based on clinical evaluation and X-ray studies. Advanced imaging, including CT and MRI, should be delayed until adequate traction (i.e., 5-10-15 lbs) or halo stabilization has been achieved. Surgical instrumentation/fusion in adults may then be warranted based on whether patients fulfill Type III or IV Fielding and Hawkins classification criteria.
CONCLUSION
Nontraumatic AARS is rare in adults. We support a stepwise management strategy that first includes traction for C1/C2 reduction and halo stabilization, followed by advanced MR/ CT imaging to document cord decompression and determine whether fusion is warranted.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Dhaon BK, Jaiswal A, Nigam V, Jain V. Atlantoaxial rotatory fixation secondary to tuberculosis of occiput: A case report. Spine (Phila Pa 1976). 2003. 28: E203-5
2. Doshi J, Anari S, Zammit-Maempel I, Paleri V. Grisel syndrome: A delayed presentation in an asymptomatic patient. J Laryngol Otol. 2007. 121: 800-2
3. Ferdinandov D, Yankov D, Bussarsky A. Grisel’s syndrome in adults: A case report. Surg Neurol Int. 2021. 12: 15
4. Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am. 1977. 59: 37-44
5. Guleryuz A, Bagdatoglu C, Duce MN, Talas DU, Celikbas H, Köksel T. Grisel’s syndrome. J Clin Neurosci. 2002. 9: 81-4
6. Ishikawa Y, Miyakoshi N, Hongo M, Kasukawa Y, Kudo D, Shimada Y. Pyogenic atlantoaxial rotational dislocation representing adult torticollis with vertebral artery occlusion: A case report and review. World Neurosurg. 2020. 144: 82-7
7. Kerolus M, Jeans EB, Fontes RB, Deutsch H, Traynelis VC. Atlantoaxial instability of inflammatory origin in adults: Case reports, literature review, and rationale for early surgical intervention. Neurosurgery. 2015. 76: E226-32 discussion E232
8. Panopalis P, Christopoulos S, Churchill-Smith M, Chankowsky J, Ménard HA. Grisel’s syndrome: Non-traumatic subluxation of the atlantoaxial joint. J Rheumatol. 2005. 32: 1619
9. Wetzel FT, La Rocca H. Grisel’s syndrome. Clin Orthop Relat Res. 1989. 240: 141-52
10. Yamazaki M, Someya Y, Aramomi M, Masaki Y, Okawa A, Koda M. Infection-related atlantoaxial subluxation (Grisel syndrome) in an adult with Down syndrome. Spine (Phila Pa 1976). 2008. 33: E156-60