- Department of Neurosurgery, Kanazawa University, Kanazawa, Ishikawa, Japan.
DOI:10.25259/SNI_361_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Wataru Uchida, Tomoya Kamide, Takehiro Uno, Akifumi Yoshikawa, Kouichi Misaki, Mitsutoshi Nakada. Ocular ischemic syndrome due to severe internal carotid artery stenosis improved by intracranial stent placement: A case report. 21-Jun-2021;12:294
How to cite this URL: Wataru Uchida, Tomoya Kamide, Takehiro Uno, Akifumi Yoshikawa, Kouichi Misaki, Mitsutoshi Nakada. Ocular ischemic syndrome due to severe internal carotid artery stenosis improved by intracranial stent placement: A case report. 21-Jun-2021;12:294. Available from: https://surgicalneurologyint.com/surgicalint-articles/10903/
Abstract
Background: Treatment of cervical internal carotid artery (ICA) stenosis has contributed to the improvement of ocular ischemic syndrome. However, there have been few cases of visual impairment caused by ocular ischemic syndrome due to intracranial ICA stenosis, which improved through intracranial stent placement.
Case Description: A 76-year-old man presented with right-sided paralysis. Radiographic examination revealed severe stenosis of the left intracranial ICA (distal cavernous-infraclinoid portion) and a watershed infarction of the left cerebral hemisphere. Conservative therapy including antiplatelet drugs was initiated, but severe visual acuity disturbance in his left eye occurred 1 month after onset. The antegrade ocular artery flow recovered after urgent intracranial stent placement, and his vision improved immediately after the procedure.
Conclusion: Visual impairment presenting as ocular ischemic syndrome can occur due to severe stenosis of the intracranial ICA, and treatment of these lesions could improve the symptoms.
Keywords: Internal carotid artery stenosis, Intracranial, Ocular ischemic syndrome, Stent placement
INTRODUCTION
Ocular ischemic syndrome, including visual impairment, amaurosis fugax, and pain, occurs secondary to severe atherosclerotic carotid artery stenosis, resulting in 50% reduction in ipsilateral perfusion pressure.[
CASE REPORT
A 76-year-old man presented with right-sided paralysis. Cerebral magnetic resonance imaging revealed a watershed infarction in the left hemisphere, and cerebral angiography revealed severe stenosis of the left intracranial ICA (distal cavernous-infraclinoid portion), without stenosis of the cervical ICA [
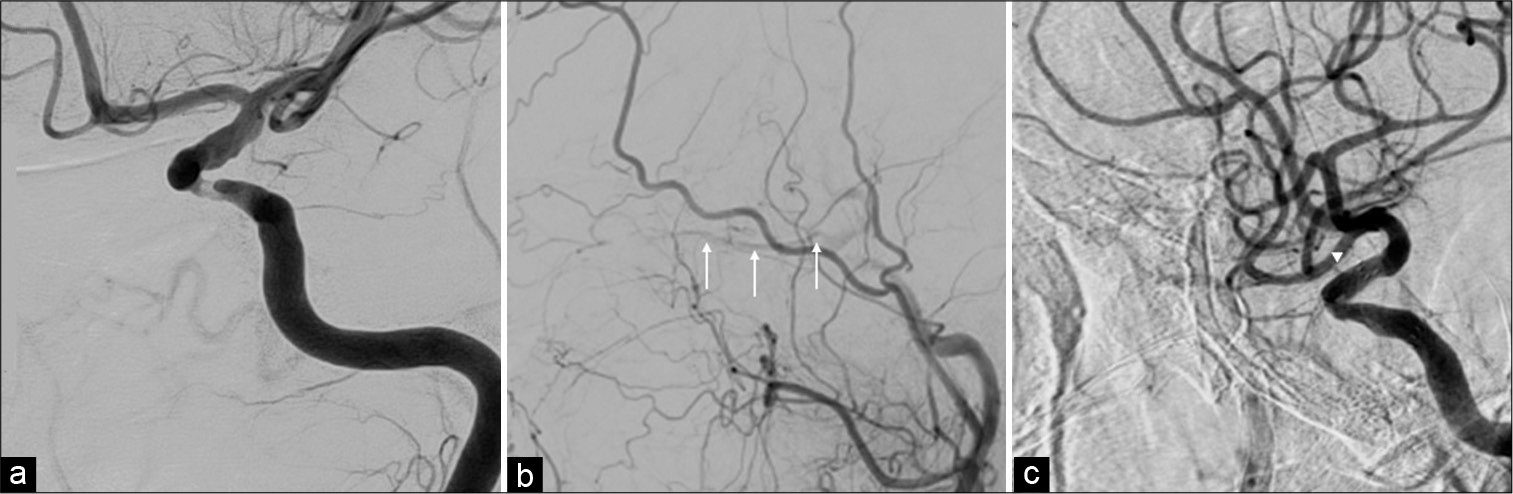
Figure 1:
Cerebral angiography of the left internal carotid artery (ICA) demonstrating severe stenosis of the left ICA at the distal cavernous-infraclinoid portion. The ocular artery was not confirmed (a). Cerebral angiography of the left common carotid artery before stent placement demonstrating the ocular artery (arrows) was depicted by a collateral blood flow from the external carotid system (b). Cerebral angiography of the left ICA after stent placement demonstrating the ocular artery (arrowhead) was depicted by a directed blood flow from the ICA (c).
Decreased blood flow to the ocular artery due to stenosis progression of the left ICA was suspected. Urgent cerebral angiography performed 2 days after the occurrence of visual impairment demonstrated that the left ICA was almost completely occluded, and the ocular artery was confirmed through anastomosis from the external carotid artery [
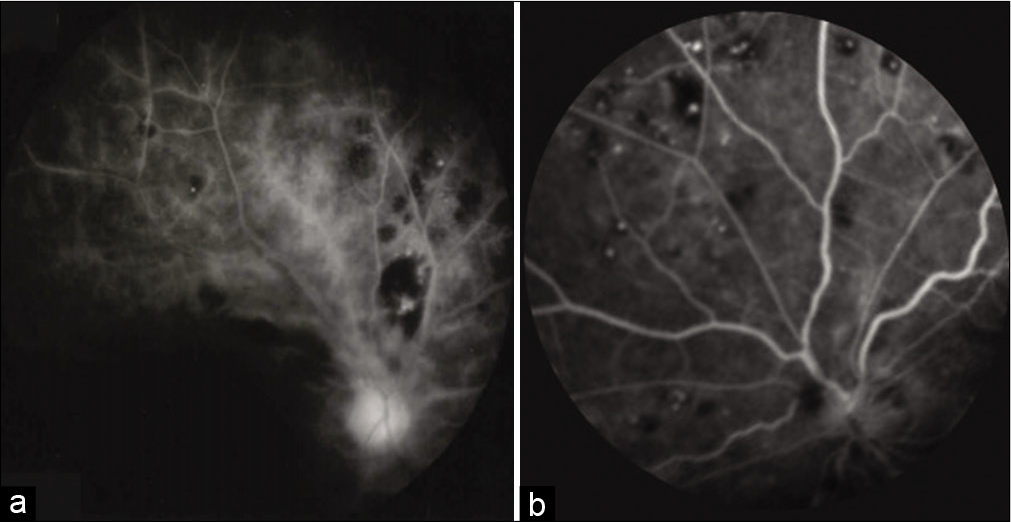
The A-R time was reduced from 54 s to 11 s, and retinal angiography also showed improvement in the visualization of blood vessels [
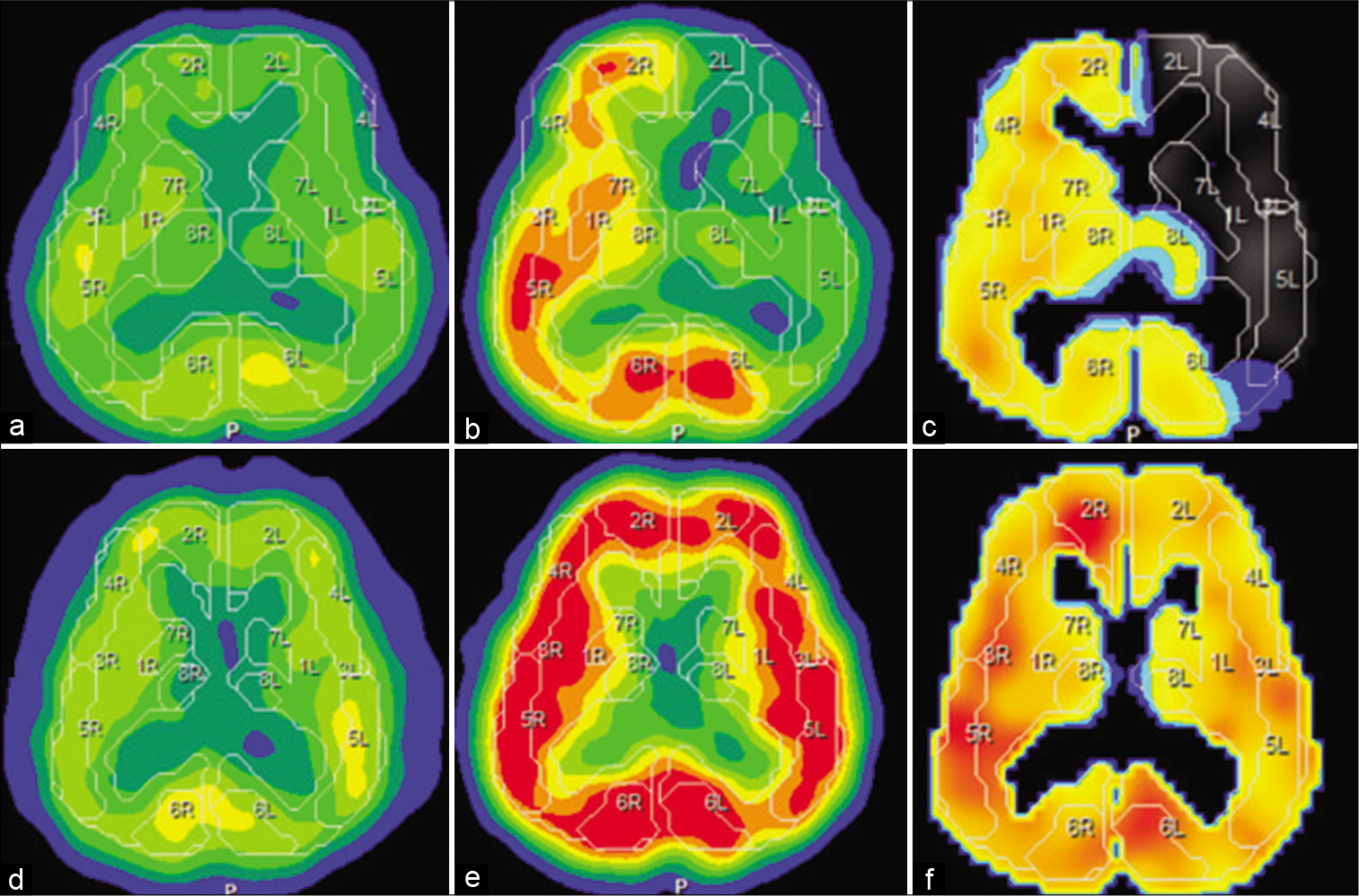
Figure 3:
Preoperative single-photon emission computed tomography (SPECT) demonstrated that his left cerebral hemisphere reserve was reduced (a-c). Postoperative SPECT showed improvement in the left cerebral blood flow reserve (e-g). (a and d) Cerebral blood flow (CBF) at rest; (b and e) CBF after acetazolamide challenge (Diamox CBF); (c and f) cerebral vascular reserve defined as (Diamox CBF-resting CBF)/ resting CBF×100%).
DISCUSSION
Ocular ischemic syndrome is caused by ocular hypoperfusion due to stenosis or occlusion of the cervical ICA.[
To evaluate ocular blood flow and retinal circulation, the A-R time measured by fluorescein fluorescence fundus examination was used in this case. In patients with severe cervical ICA stenosis, the A-R time was prolonged and was improved after CAS at a high rate.[
Complications related to PTA have been reported: cerebral embolism, vessel dissection, hemodynamic compromise, and cerebral hyperperfusion syndrome. Regarding visual acuity, angioplasty of the ICA could increase ocular blood flow, but intraocular pressure elevation due to increased aqueous humor might result in decreased visual acuity.[
The Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis trial supports the use of aggressive medical management rather than PTAS with the Wingspan system in patients with intracranial arterial stenosis.[
CONCLUSION
The improvement in blood flow in the ICA contributes to an increased blood flow in the ocular artery irrespective of whether it is cervical or intracranial ICA in patients with ocular ischemic syndrome. PTAS might be considered as a treatment option for ocular ischemic syndrome due to intracranial ICA stenosis when the best medical treatment fails.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Biousse V, Newman NJ. Eye syndromes and the neuroophthalmology of stroke. Handb Clin Neurol. 2009. 93: 595-611
2. Brown GC, Magargal LE. The ocular ischemic syndrome. Clinical, fluorescein angiographic and carotid angiographic features. Int Ophthalmol. 1988. 11: 239-51
3. Derdeyn CP, Chimowitz MI, Lynn MJ, Fiorella D, Turan TN, Janis LS. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): The final results of a randomized trial. Lancet. 2014. 383: 333-41
4. Hayashi M, Sato K, Yokouchi T, Harashina JI, Nakayama H, Akahata M. Retinal circulation before and after carotid artery stenting. Surg Cereb Stroke. 2011. 39: 96-102
5. Katsuta T, Fujimoto A, Oba K. Deterioration of glaucoma after carotid endarterectomy. Neurol Med Chir (Tokyo). 2013. 53: 418-21
6. Kawaguchi S, Iida J, Uchiyama Y. Ocular circulation and chronic ocular ischemic syndrome before and after carotid artery revascularization surgery. J Ophthalmol. 2012. 2012: 350475
7. Lee JH, Yun JK, Kim DW, Kang SD. Clinical and angiographic outcomes of wingspan stent placement for treatment of symptomatic intracranial stenosis: Single center experience with 19 cases. J Cerebrovasc Endovasc Neurosurg. 2012. 14: 157-63
8. Marx JL, Hreib K, Choi IS, Tivnan T, Wertz FD. Percutaneous carotid artery angioplasty and stenting for ocular ischemic syndrome. Ophthalmology. 2004. 111: 2284-91
9. Mi Lee K, Kim EJ, Heo SH, Kyung HJ. Paradoxical development of neovascular glaucoma following carotid angioplasty and stenting. Interv Neuroradiol. 2016. 22: 540-3
10. Ng E, Choong AM, Walker PJ. Neovascular glaucoma post carotid endarterectomy: A case report and review of the literature. Ann Vasc Dis. 2015. 8: 103-5
11. Ranasinghe T, Boo S, Adcock A. Rare phenomenon of limb-shaking TIA, resolved with intracranial wingspan stenting. Neurologist. 2019. 24: 37-9