- Department of Neurosurgery, Research Institute i+12-CIBERESP, Hospital Universitario 12 de Octubre, Universidad Complutense de Madrid, Avda Cordoba SN, Madrid, Spain.
DOI:10.25259/SNI_597_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ana M. Castaño-Leon, Jose F. Alen, Alfonso Lagares. Opening of unusual vascular collaterals leads to early recanalization of a giant intracavernous carotid artery aneurysm following common carotid artery occlusion: A Case report and literature review. 04-Apr-2020;11:62
How to cite this URL: Ana M. Castaño-Leon, Jose F. Alen, Alfonso Lagares. Opening of unusual vascular collaterals leads to early recanalization of a giant intracavernous carotid artery aneurysm following common carotid artery occlusion: A Case report and literature review. 04-Apr-2020;11:62. Available from: https://surgicalneurologyint.com/surgicalint-articles/9943/
Abstract
Background: Parent artery occlusion (PAO) with or without bypass surgery is a feasible treatment for large intracavernous carotid artery (ICCA) aneurysms. The ideal occlusion site (internal or common carotid artery [CCA]) and ischemic complications after PAO have received special attention since the description of the technique. Unfrequently, some patients can also develop unusual external carotid artery-internal carotid artery collateral pathways distal to the ligation site that can explain the failure to aneurysm size reduction.
Case Description: We describe a rare case of delayed refilling of a large ICCA aneurysm partially thrombosed which early recanalized after surgical ligation of the cervical CCA through an unusual collateral pathway.
Conclusion: Based on our experience, we recommend periodic long-term follow-up neuroimaging, especially in those cases where potential collateral branches have not been clearly identified in the preoperative studies.
Keywords: Aneurysm, Collateral pathways, Intracavernous carotid artery, Parent artery occlusion
INTRODUCTION
Intracavernous carotid artery (ICCA) aneurysms account for 3–5% of all intracranial aneurysms.[
In most centers, due to the challenging exposition of ICCA, these aneurysms are considered not amenable for clipping, and their management usually consists in coiling or flow-diverter placement. Parent artery occlusion (PAO) is a feasible alternative in those cases with intra-aneurysm or internal carotid artery (ICA) thrombosis, none or very wide neck, age or medical condition of the patient, and after failure of endovascular techniques. There are a number of alternatives according to the location (ICA or common carotid artery [CCA]), timing (abrupt ligation or prolonged closure with temporal clamps),[
The reported mortality and morbidity rates of surgical PAO range from 6–20% to 4–12%, respectively.[
Here, we present a rare case of a partially thrombosed ICCA aneurysm which early recanalized after surgical ligation of the cervical CCA via an unusual collateral pathway.
CASE REPORT
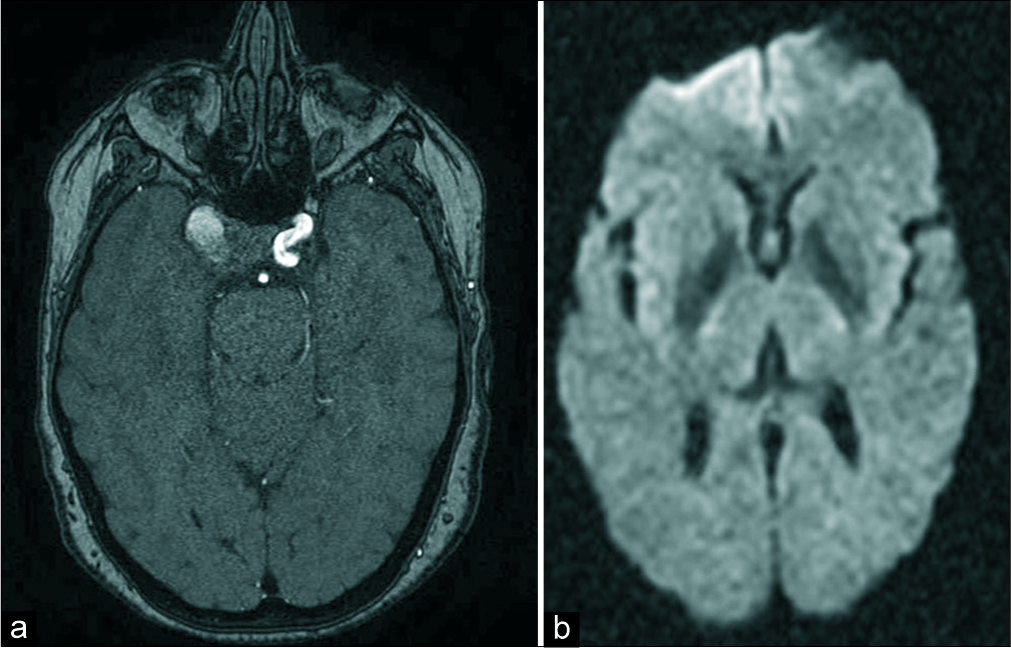
A 63-year-old woman, with arterial hypertension as the only relevant medical history, presented with a sudden binocular diplopia. Right 6th nerve palsy was evidenced on physical examination at admission. AngioCT revealed a right ICCA aneurysm with signs of partial thrombosis without evidence of rupture [
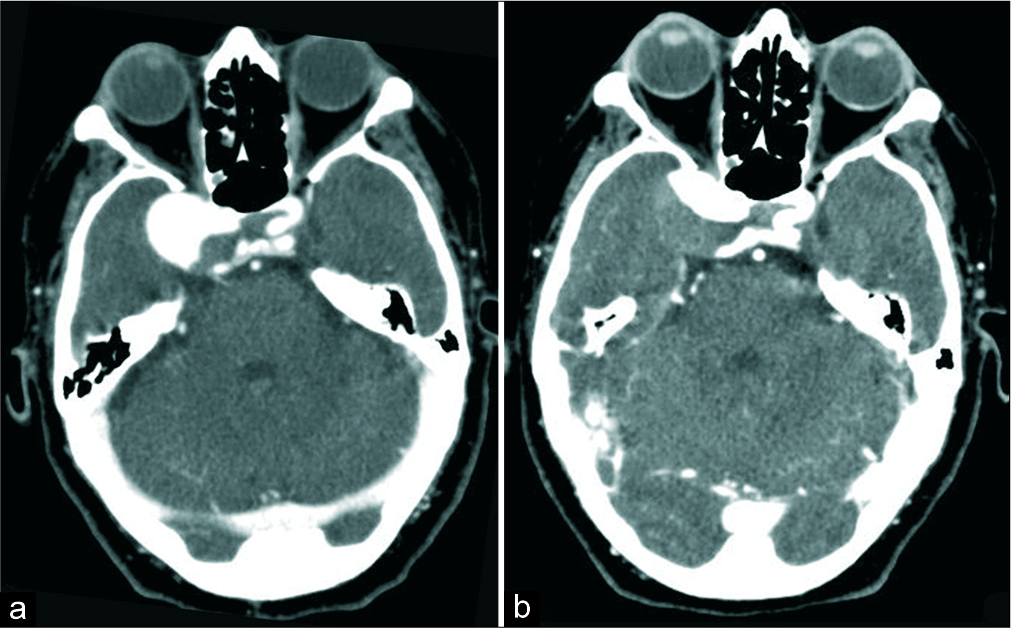
Figure 1:
Admission AngioCT revealed a right intracavernous carotid artery (ICCA) aneurysm with signs of partial thrombosis without evidence of rupture (a). The patient experienced complete cavernous sinus syndrome in relation to progression of thrombosis of the ICCA aneurysm as a new AngioCT showed (b).
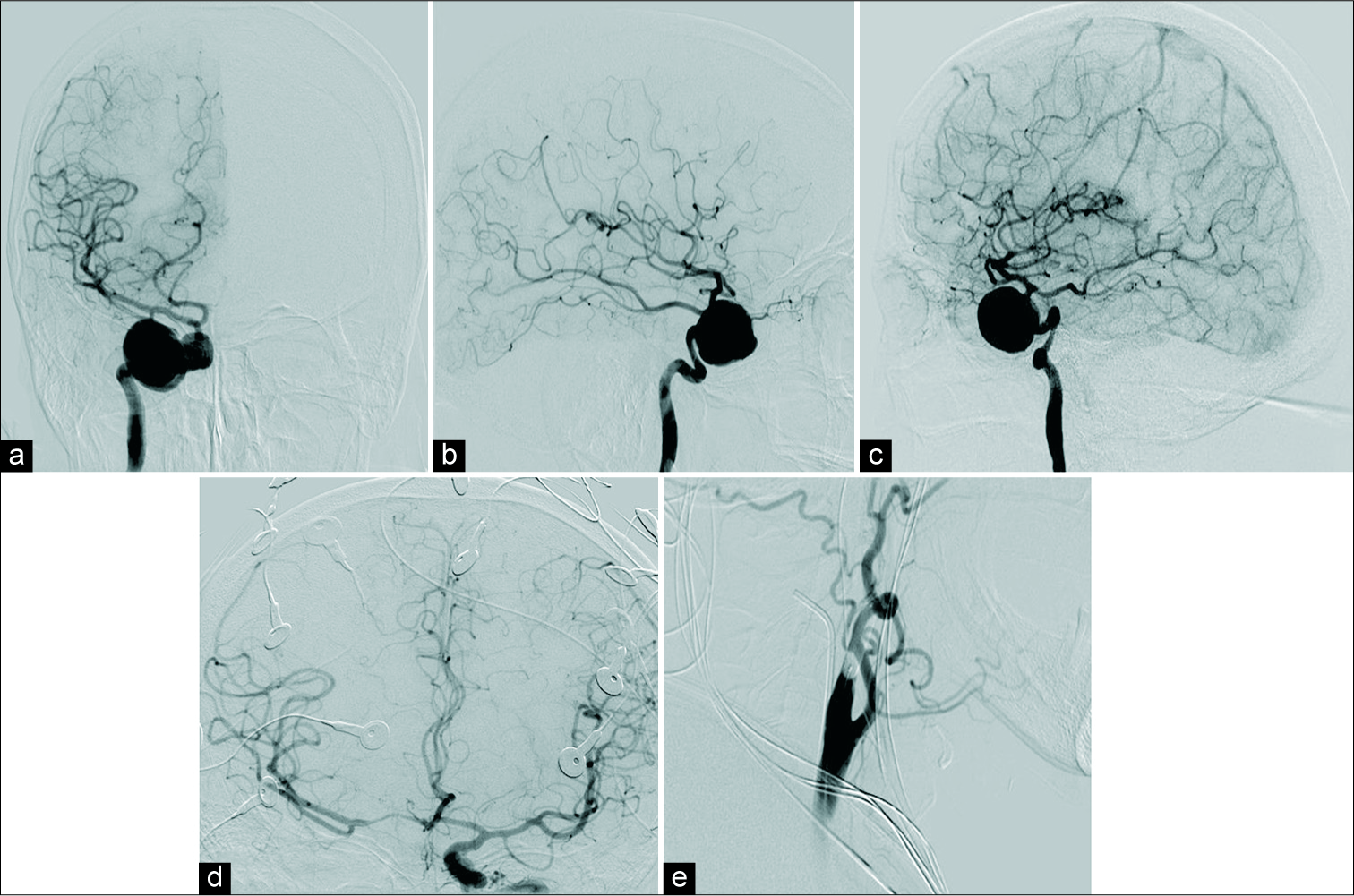
Figure 2:
Right carotid angiography, anteroposterior (a) lateral (b) and oblique (c) projections, indicates a giant aneurysm (25 mm of main diameter, 9 mm neck width) at the cavernous segment of the right ICA. Left carotid angiography, anteroposterior projection, showing adequate collateral reserve via anterior communicating artery (d) and the aneurysm without filling of contrast after balloon occlusion at the proximal portion of the right ICA (e).
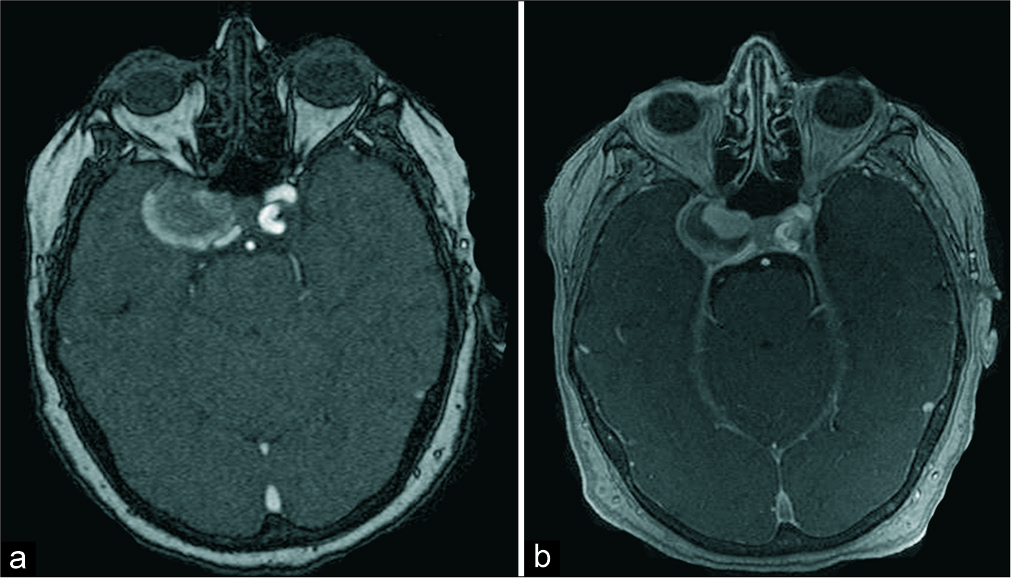
Nine months later, and without new neurological symptoms, signs of aneurysm growth were detected in a serial MRA [
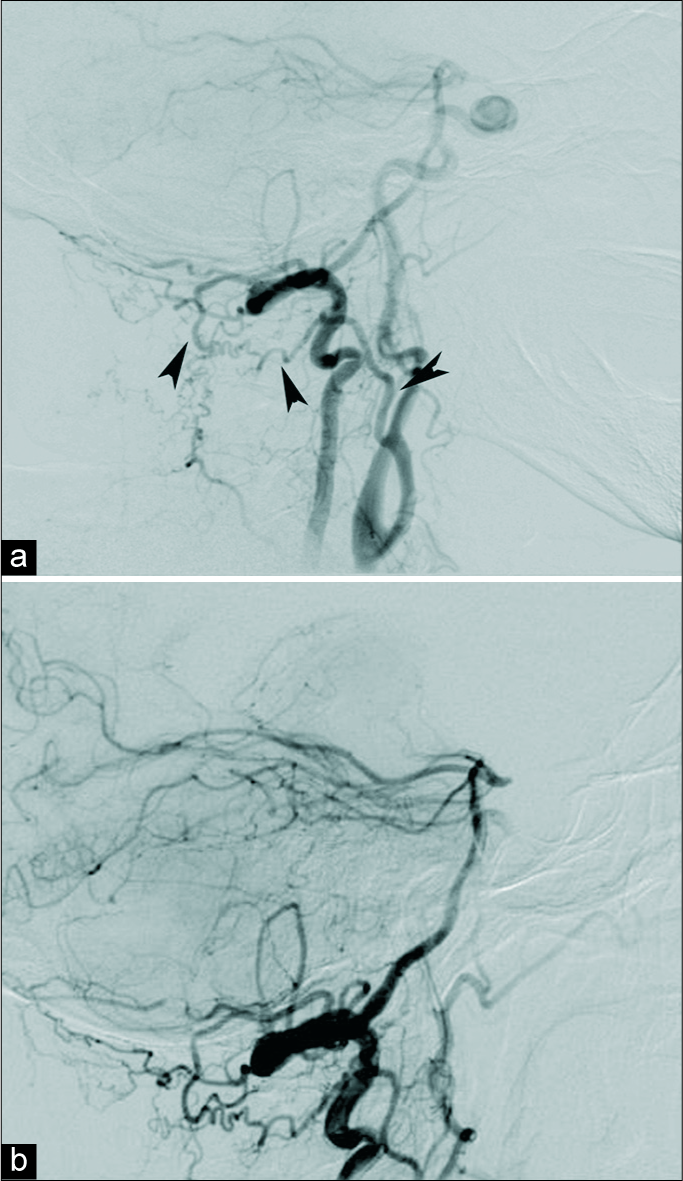
Figure 4:
Nine months after common carotid artery ligation, a right vertebral angiography (lateral projection) showed partial recanalization of the intracavernous carotid artery (ICCA) aneurysm (a). Collateral supply was explained from external carotid artery through the occipital artery with an inverse flow to the internal carotid artery (ICA) (arrowheads). After cervical ICA surgical ligation, a new right vertebral angiography confirmed total occlusion of the ICCA aneurysm (b).
DISCUSSION
In ICCA aneurysms, due to the small number and caliber of branching vessels, PAO is a feasible option for treatment.[
Even when similar rates of success have been reported, there is controversy about the best site of PAO.[
Although ischemic and thromboembolic complications after PAO have received the attention, delayed refilling of ICCA aneurysm could happen. Conventionally, collateral pathway development is based on the proliferation of vasa vasorum induced by neoangiogenic factors after progressive atherothrombotic ICA occlusion.[
According to the previous data, two main types of recanalization after PAO may occur:
Retrograde recanalization: backflow of the ophthalmic artery,[ Anterograde recanalization: vasa vasorum and collateral embryonal pathways between the ICA and ECA (in the case of CCA, meningohypophyseal branches, and inferior lateral trunk). Recently, Wang[
In our opinion, some of the mechanisms that explain the lower risk of thromboembolism and ischemia after CCA occlusion are the same that influence the opening of unusual collaterals. The importance of the evaluation of proximal intracranial ICA branches during the planification of the site of PAO was described by Allen.[
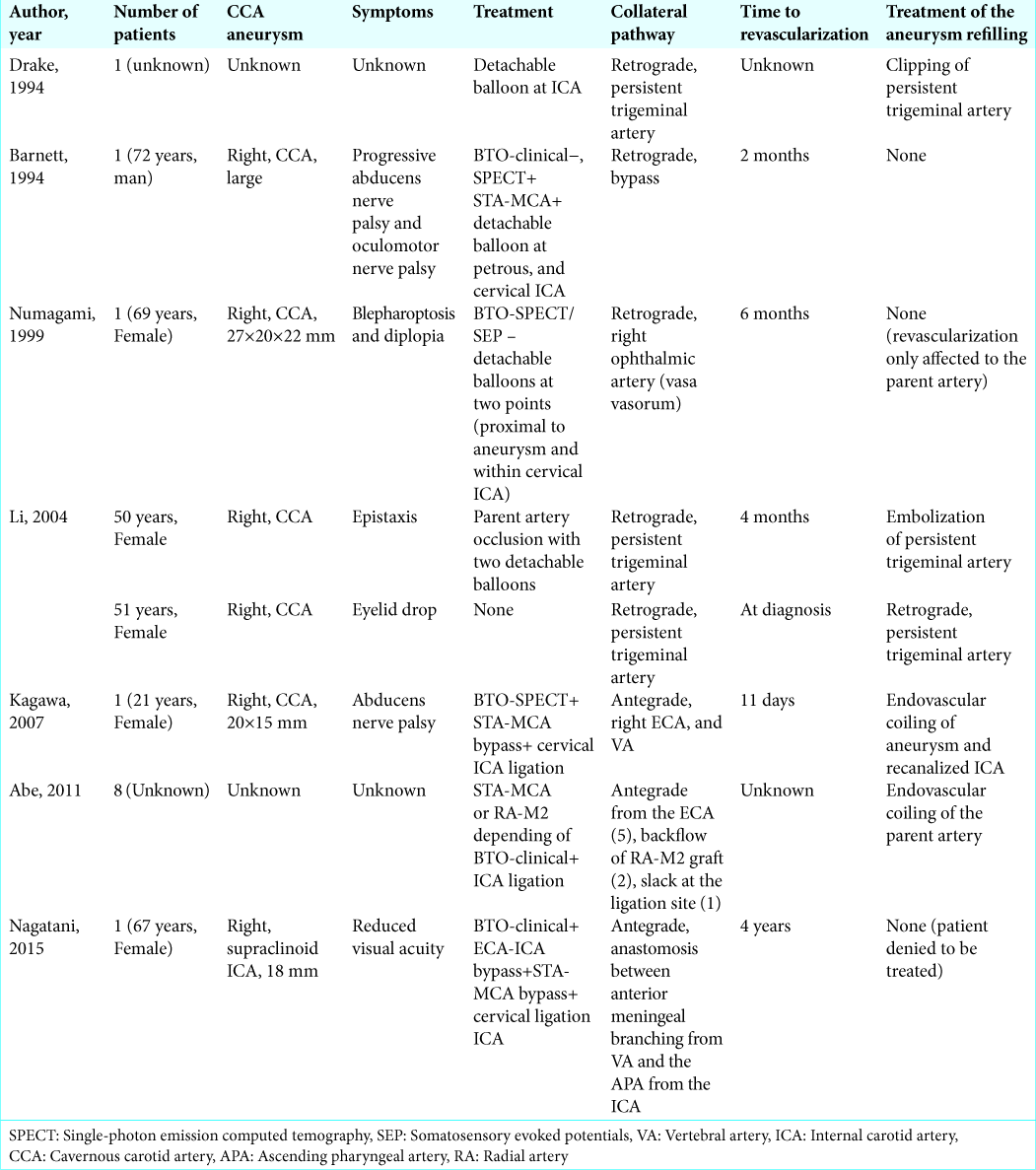
Even with the mentioned multiple sources recanalization of ICCA aneurysms after PAO is a rare complication. If we review the literature of previously reported cases, we identify only seven studies [
CONCLUSION
Delayed refilling of ICCA aneurysms based on unusual collateral pathway opening after PAO may occur. Periodic long-term follow-up by neuroimaging is recommended, especially in those cases where potential collateral branches of have not been clearly identified in the preoperative studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abe H, Takemoto K, Higashi T, Inoue T. Surgical treatment for aneurysms in the cavernous-petrous portion of the internal carotid artery. Acta Neurochir Suppl. 2011. 112: 77-83
2. Allen JW, Alastra AJ, Nelson PK. Proximal intracranial internal carotid artery branches: Prevalence and importance for balloon occlusion test. J Neurosurg. 2005. 102: 45-52
3. Ambekar S, Madhugiri V, Sharma M, Cuellar H, Nanda A. Evolution of management strategies for cavernous carotid aneurysms: A review. World Neurosurg. 2014. 82: 1077-85
4. Barnett DW, Barrow DL, Joseph GJ. Combined extracranial-intracranial bypass and intraoperative balloon occlusion for the treatment of intracavernous and proximal carotid artery aneurysms. Neurosurgery. 1994. 35: 92-7
5. Countee RW, Vijayanathan T. External carotid artery in internal carotid artery occlusion. Angiographic, therapeutic, and prognostic considerations. Stroke. 1979. 10: 450-60
6. Drake CG, Peerless SJ, Ferguson GG. Hunterian proximal arterial occlusion for giant aneurysms of the carotid circulation. J Neurosurg. 1994. 81: 656-65
7. Elhammady MS, Wolfe SQ, Farhat H, Ali Aziz-Sultan M, Heros RC. Carotid artery sacrifice for unclippable and uncoilable aneurysms: Endovascular occlusion vs common carotid artery ligation. Neurosurgery. 2010. 67: 1431-6
8. Ezura M, Takahashi A, Yoshimoto T. Combined intravascular parent artery and ophthalmic artery occlusion for giant aneurysms of the supraclinoid internal carotid artery. Surg Neurol. 1997. 47: 360-3
9. Field M, Jungreis CA, Chengelis N, Kromer H, Kirby L, Yonas H. Symptomatic cavernous sinus aneurysms: Management and outcome after carotid occlusion and selective cerebral revascularization. AJNR Am J Neuroradiol. 2003. 24: 1200-7
10. Fox AJ, Viñuela F, Pelz DM, Peerless SJ, Ferguson GG, Drake CG. Use of detachable balloons for proximal artery occlusion in the treatment of unclippable cerebral aneurysms. J Neurosurg. 1987. 66: 40-6
11. Fox JL. Cerebral arterial revascularization: The value of repeated angiography in selection of patients for operation. Neurosurgery. 1978. 2: 205-9
12. Fujiwara S, Fujii K, Fukui M. De novo aneurysm formation and aneurysm growth following therapeutic carotid occlusion for intracranial internal carotid artery (ICA) aneurysms. Acta Neurochir (Wien). 1993. 120: 20-5
13. Giannotta SL, McGillicuddy JE, Kindt GW. Gradual carotid artery occlusion in the treatment of inaccessible internal carotid artery aneurysms. Neurosurgery. 1979. 5: 417-21
14. Heros RC. Thromboembolic complications after combined internal carotid ligation and extra-to-intracranial bypass. Surg Neurol. 1984. 21: 75-9
15. Higashida RT, Halbach VV, Dowd C, Barnwell SL, Dormandy B, Bell J. Endovascular detachable balloon embolization therapy of cavernous carotid artery aneurysms: Results in 87 cases. J Neurosurg. 1990. 72: 857-63
16. Hongo K, Horiuchi T, Nitta J, Tanaka Y, Tada T, Kobayashi S. Double-insurance bypass for internal carotid artery aneurysm surgery. Neurosurgery. 2003. 52: 597-602
17. Kagawa K, Shimizu H, Matsumoto Y, Watanabe M, Tominaga T. Rapid revascularization after therapeutic parent artery occlusion for a large intracavernous carotid artery aneurysm. Neurol Med Chir (Tokyo). 2007. 47: 559-63
18. Kak VK, Taylor AR, Gordon DS. Proximal carotid ligation for internal carotid aneurysms. A long-term follow-up study. J Neurosurg. 1973. 39: 503-13
19. Kemény V, Droste DW, Nabavi DG, Schulte-Altedorneburg G, Schuierer G, Ringelstein EB. Collateralization of an occluded internal carotid artery via a vas vasorum. Stroke. 1998. 29: 521-3
20. Kupersmith MJ, Hurst R, Berenstein A, Choi IS, Jafar J, Ransohoff J. The benign course of cavernous carotid artery aneurysms. J Neurosurg. 1992. 77: 690-3
21. Kurokawa R, Kuroshima Y, Yoshida K, Kawase T. Spontaneous thrombosis of intracavernous internal carotid artery aneurysm and parent artery occlusion in patients with positive balloon test occlusion two case reports. Neurol Med Chir (Tokyo). 2001. 41: 436-41
22. Linskey ME, Sekhar LN, Hirsch W, Yonas H, Horton JA. Aneurysms of the intracavernous carotid artery: Clinical presentation, radiographic features, and pathogenesis. Neurosurgery. 1990. 26: 71-9
23. Linskey ME, Sekhar LN, Horton JA, Hirsch WL, Yonas H. Aneurysms of the intracavernous carotid artery: A multidisciplinary approach to treatment. J Neurosurg. 1991. 75: 525-34
24. Little JR, Rosenfeld JV, Awad IA. Internal carotid artery occlusion for cavernous segment aneurysm. Neurosurgery. 1989. 25: 398-404
25. Meguro T, Muraoka K, Terada K, Hirotsune N, Nishino S. Recanalisation of the internal carotid artery via the vasa vasorum after coil occlusion. Br J Radiol. 2011. 84: e23-6
26. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005. 366: 809-17
27. Nagatani K, Tsuzuki N, Kageyama H, Shima K. Recanalization of a large supraclinoid carotid aneurysm via elicited vertebral artery-internal carotid artery anastomosis: A case report. Turk Neurosurg. 2015. 25: 154-7
28. Nakase H, Shin Y, Kanemoto Y, Ohnishi H, Morimoto T, Sakaki T. Long-term outcome of unruptured giant cerebral aneurysms. Neurol Med Chir (Tokyo). 2006. 46: 379-84
29. Niiro M, Shimozuru T, Nakamura K, Kadota K, Kuratsu J. Long-term follow-up study of patients with cavernous sinus aneurysm treated by proximal occlusion. Neurol Med Chir (Tokyo). 2000. 40: 88-96
30. Numagami Y, Ezura M, Takahashi A, Yoshimoto T. Antegrade recanalization of completely embolized internal carotid artery after treatment of a giant intracavernous aneurysm: A case report. Surg Neurol. 1999. 52: 611-6
31. Puffer RC, Piano M, Lanzino G, Valvassori L, Kallmes DF, Quilici L. Treatment of cavernous sinus aneurysms with flow diversion: Results in 44 patients. AJNR Am J Neuroradiol. 2014. 35: 948-51
32. Raper DM, Ding D, Peterson EC, Crowley RW, Liu KC, Chalouhi N. Cavernous carotid aneurysms: A new treatment paradigm in the era of flow diversion. Expert Rev Neurother. 2017. 17: 155-63
33. Roski RA, Spetzler RF, Nulsen FE. Late complications of carotid ligation in the treatment of intracranial aneurysms. J Neurosurg. 1981. 54: 583-7
34. Shimizu K, Imamura H, Mineharu Y, Adachi H, Sakai C, Tani S. Endovascular parent-artery occlusion of large or giant unruptured internal carotid artery aneurysms. A long-term single-center experience. J Clin Neurosci. 2017. 37: 73-8
35. Stiebel-Kalish H, Kalish Y, Bar-On RH, Setton A, Niimi Y, Berenstein A. Presentation, natural history, and management of carotid cavernous aneurysms. Neurosurgery. 2005. 57: 850-7
36. Taki W, Nishi S, Yamashita K, Sadatoh A, Nakahara I, Kikuchi H. Selection and combination of various endovascular techniques in the treatment of giant aneurysms. J Neurosurg. 1992. 77: 37-42
37. Tatemichi TK, Chamorro A, Petty GW, Khandji A, Oropeza LA, Duterte DI. Hemodynamic role of ophthalmic artery collateral in internal carotid artery occlusion. Neurology. 1990. 40: 461-4
38. Turfe ZA, Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular coiling versus parent artery occlusion for treatment of cavernous carotid aneurysms: A meta-analysis. J Neurointerv Surg. 2015. 7: 250-5
39. van der Schaaf IC, Brilstra EH, Buskens E, Rinkel GJ. Endovascular treatment of aneurysms in the cavernous sinus: A systematic review on balloon occlusion of the parent vessel and embolization with coils. Stroke. 2002. 33: 313-8
40. van Rooij WJ. Endovascular treatment of cavernous sinus aneurysms. AJNR Am J Neuroradiol. 2012. 33: 323-6
41. Wang J, Zheng C, Hou B, Huang A, Zhang X, Du B. Four collateral circulation pathways were observed after common carotid artery occlusion. BMC Neurol. 2019. 19: 201-
42. Wiebers DO, Whisnant JP, Huston J, Meissner I, Brown RD, Piepgras DG. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003. 362: 103-10