- Division of Neurosurgery, City of Hope National Medical Center, Los Angeles, California, United States,
- Halmos College of Natural Sciences and Oceanography, Nova Southeastern University, Fort Lauderdale, Florida, United States,
- Department of Neurological Surgery, Hospital Del Nino, Murillo, Bolivia
- Department of Pediatric Neurosurgery, University of California San Diego, San Diego, California, United States.
Correspondence Address:
Rahul Jandial, Division of Neurosurgery, City of Hope National Medical Center, 1500 East Duarte Road, Los Angeles - 91010, California, United States.
DOI:10.25259/SNI_241_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rahul Jandial1, Pranay Narang2, Jorge Daniel Brun3, Michael L. Levy4. Optimizing international neurosurgical outreach missions: 15-year appraisal of operative skill transfer in Lima, Peru. 24-Aug-2021;12:425
How to cite this URL: Rahul Jandial1, Pranay Narang2, Jorge Daniel Brun3, Michael L. Levy4. Optimizing international neurosurgical outreach missions: 15-year appraisal of operative skill transfer in Lima, Peru. 24-Aug-2021;12:425. Available from: https://surgicalneurologyint.com/surgicalint-articles/11057/
Abstract
Background: While several medical outreach models have been designed and executed to alleviate the unmet need for international neurosurgical care, disparate strategies have evolved. There is a need to determine the optimal pediatric neurosurgical outreach model through which resources are efficiently utilized while imparting the largest possible impact on global health. This study evaluates the efficacy of an international pediatric neurosurgery outreach model at transferring operative skill in a sustainable and scalable manner in Lima, Peru over a 15-year duration.
Methods: Three 1-week neurosurgical missions were carried out (2004–2006) in Lima, Peru to teach neuroendoscopic techniques and to provide equipment to host neurosurgeons, equipping the hosts to provide care to indigent citizens beyond the duration of the missions. Follow-up data were obtained over a 15 year span, with collaboration maintained over email, two in-person visits, and video-conferencing services.
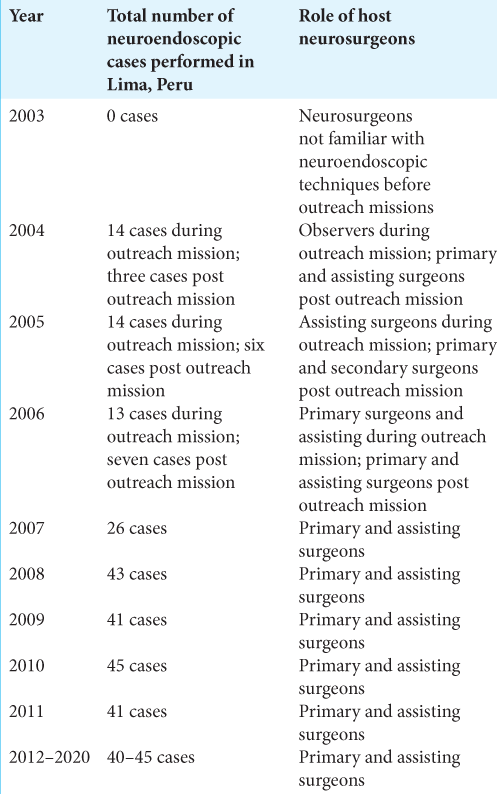
Results: Since the outreach missions in 2004–2006, the host neurosurgeons demonstrated sustainability of the neuroendoscopic instruction by independently performing neuroendoscopic operations on a growing caseload: at baseline, 0 cases were performed in 2003, but since 2012 and onwards, 40–45 cases have been performed annually. Scalability is illustrated by the fact that the institution established a rigorous neuroendoscopy training program to independently pass on the techniques to resident physicians.
Conclusion: The described international pediatric neurosurgical outreach model, centered around teaching operative technique as opposed to solely providing care to citizens, allowed operative skill to be sustainably transferred to surgeons in Lima, Peru. Having served the neuroendoscopic needs of hundreds of citizens, the strategic design is replicable and should be mirrored by future medical endeavors seeking to substantially impact the deficit in global surgical care.
Keywords: Didactic model, International outreach, Pediatric neurosurgery, Surgical missions, Sustainable surgical care
INTRODUCTION
With the medical establishment having felt a series of clinical and technological breakthroughs over the past 100 years, the human life expectancy has been extended by 30 years in many developed countries.[
According to the World Health Organization, 5 billion people currently do not have access to safe, timely, and affordable surgical care and anesthesia worldwide.[
Since the publication of Global Surgery 2030, which reported that 28–32% of the global burden of disease can be attributed to surgically treatable conditions,[
In accordance with the fourth category of humanitarian surgical outreach, it is expected that the optimal framework for neurosurgical outreach, and outreach for most specialties, must be founded on a mission objective to teach surgical skills such that operations can be continuously performed by local providers after visiting surgeons depart. This model must be comprehensively designed, ensuring that the logistics of neurosurgical care are established at the neurosurgical site, securing fluid, and thorough communication between visiting and host providers, and empowering host neurosurgeons to take on increasingly challenging cases with a refined skill set and equipment that can be sustainably utilized for improved neurosurgical care. Having designed and employed such a model through three 1-week targeted pediatric neurosurgical outreach missions from 2004 to 2006 in Lima, Peru, the intent of this paper is to present a 15-year follow-up, assessing the degree to which operative skill was transferred as the fundamentally important feature of sustainable international surgical care.[
While the model was recognized for its effectiveness after a 5-year follow-up study that encompassed promising data,[
MATERIALS AND METHODS
Mission objective
With the objective of implementing a replicable model by which international neurosurgical care enhancements can be made and sustained, three targeted 1-week missions were undertaken from 2004 to 2006. Following correspondence with South American neurosurgical societies, the Maria Auxiliadora Hospital [
Site evaluation
The first step to the pediatric neurosurgical outreach missions was to evaluate the site in person. After establishing contact through telephone and email, a site evaluation took place in 2003 to verify that the perceived “need” warranted an outreach mission, and to make sense of the severity of the need. Insights from the site evaluation influenced the design of the mission. Ethically, the evaluation also ensured that the host neurosurgical team was genuinely dedicated to improving the quality of care delivered to indigent populations. This evaluation established in-person contact with the host neurosurgeons and with hospital leadership. Establishing such support was critical for the cooperation of the other surgeons, many of whom had to relinquish operating days during the missions, and for the nurses, who were ultimately prepped for the increased case volume and postoperative needs.
For future medical outreach missions, it should be recognized that a thorough site evaluation conducted before the inaugural outreach is of paramount importance. Without an in-person site evaluation corroborating the need, the dedicated resources may be suboptimally allocated as the mission design will not be centered around the specific needs of the institution.
Strategic mission design for international pediatric neurosurgical outreach in Lima, Peru
Following verification of the need for neurosurgical care enhancements at the hospital in Lima, Peru, the three-mission outreach was executed between 2004 and 2006, with one 1-week mission taking place per year. During the inaugural mission, the mission’s foundation was officially cemented; the host team was able to demonstrate their capacity to successfully coordinate and execute the logistics of neurosurgical care: patient selection, operative schedule management, obtaining approval for anesthesia, nursing, and beds, and postoperative care. Focusing on endoscopy cases, the visiting team carried out operations interspersed with grand-round style case presentation and discussion. The second mission focused more on didactic elements and was increasingly collaborative. Both the host neurosurgeons and visiting neurosurgeons were paired as primary and assistant neurosurgeons for the trip, and host surgeons took an increasingly important role in operative cases. In accordance with the host surgeons’ level of skill, some began to function as primary surgeons in certain cases. On the third visit, the host team served as the primary surgeons of all cases. Visiting neurosurgeons functioned solely as observers, and the mission team evaluated host team performance in increasingly challenging specialty cases.[
The intent of this structure was to enhance the institution’s capacity to manage neurosurgical care, while gradually empowering the host neurosurgeons to take on increasing responsibility over time; this also ensured that the lessons were retained, mastered, and built upon in the subsequent months between the missions and thereafter. This process secured a deep culture built on trust and high quality collaboration between the two teams, forging relationships and sustaining a high level of engagement to efficiently tackle the mission’s objective.
Sustaining the impact-opportunities in the post COVID-19 hyperdigital world
Through 2004–2006 and for five subsequent years, communication was maintained through email. For the first 5 years, the host team would report the total volume of cases, the time duration for follow-ups, and the patient outcomes, allowing the efficacy of the neurosurgical outreach model to be assessed in terms of sustainability.[
RESULTS
Following the three missions, two local senior faculty neurosurgeons were trained in basic neuroendoscopy, and the institution was provided a portable endoscopy unit and disposable endoscopes that could be paired with a colored television monitor already in possession. Maintaining communication through email for the first 5 subsequent years, it was apparent that the host neurosurgeons were taking on a gradually larger caseload independently over time, as apparent in [
In accordance with the clinical priority to reduce the count of ventriculoperitoneal shunting procedures, the host team treated children with fewer shunts over the first 5 years. Precise data were not available, but the host team estimated that for every three endoscopy cases, two shunts were avoided, with approximately 20% of cases requiring shunting after an endoscopic effort. In the subsequent 10 years, collaboration became need based as the faculty became increasingly adept with complex neuroendoscopic procedures, as apparent from digital collaboration. Through two in-person visits in 2010 and 2015 to assess sustainability, and from sporadic video chat based collaborations through platforms such as FaceTime, Google Meets, and Zoom, sustainability was perpetually assessed to ensure that the impact of the three missions was not lost over time. From the two in person visits in 2010 and 2015, it was apparent that operative skill continued to be successfully transferred: in addition to the faculty that had been trained over the three missions, Maria Auxiliadora Hospital hosted a new robust neuroendoscopy program that equipped each new resident with the technical skill set that had been acquired from the outreach missions. In establishing such a program and successfully passing on the neuroendoscopic lessons through resident classes, it could be seen that the institution’s neurosurgical care was deeply enhanced, sustained, and built on in the ensuing years after the three missions. Shunts were no longer being purchased, and the neuroendoscopic techniques had evolved to even support the physicians in carrying out biopsies, benefitting the patients greatly. From speaking with the faculty, it was seen that the caseload remained constant at between 41 and 45 cases per year after 2012, a significant increase from the three cases that were independently performed in 2004, as illustrated in [
The faculty of Maria Auxiliadora Hospital believed that there was a very high proportion of successful outcomes for each annual neuroendoscopic caseload, with very few complications, improved surgical performance, and more efficient resource utilization. As with the first 5 years, patient follow-ups were limited through the decade.
DISCUSSION
With 15 years having passed since the inaugural mission in Lima, Peru, the insights that have been gleaned from the neurosurgical outreach and the data that have been collected on the number of neuroendoscopic cases conducted per year provides a means of assessing the efficacy and replicability of this outreach model.
Oftentimes, international medical missions are centered around providing direct care to citizens in need; however, these missions are episodic in nature, with the impact of the missions collapsing soon after the visiting surgeons depart from the country. With the emergent nature of neurosurgical care, the goal at hand was to establish a model of systems that would empower host neurosurgeons to effectively and sustainably provide higher quality pediatric neurosurgical care for their citizens,[
Between the three visits, it was apparent that the host team demonstrated excellent surgical skill, an understanding of disease processes and postoperative management strategies, and a capacity to perform routine neuroendoscopic cases. Performing 40–45 cases in 2020, the host team’s improvement in their neurosurgical care was very apparent when compared to their baseline, during which shunts were routinely used since a familiarity with neuroendoscopic protocols was largely absent. With a very high proportion of successful patient outcomes in the subsequent years, as seen in the 5-year follow-up[
Neuroendoscopy is an alternative modality for treating hydrocephalus which avoids placing a shunt in children. Besides the fact that shunting procedures are time consuming, costly, and carry a risk of infection, shunts are susceptible to malfunction, as documented in a large prospective multi-institutional investigation that demonstrated that 40% of patients require a shunt revision within 2 years of the first placement.[
In the past 10 years, the collaboration through digital platforms such as FaceTime, Google Meets, and more recently, Zoom, provided abundant opportunities to further enhance the skill set of the physicians in Lima, Peru. With conversations gradually having progressed from short, concise emails to digital video collaborations, the degree of information that could be extracted from each interaction increased tremendously. The host physicians gained a deeper understanding of the root causes of disease and became more skilled with surgical instruments and technology systems that were less routinely used or unavailable in 2004. While virtual support was significantly augmented during the COVID-19 pandemic, there is room to further capitalize on the available technologies to reduce the international disparities in quality of care. The discipline of neurosurgery has rapidly changed in the past 100 years, though these developments are not evenly distributed between developed and developing nations.[
The COVID-19 pandemic has forced neurosurgeons across the world to familiarize themselves with video-conferencing services (e.g., Zoom Video Communications, Inc., San Jose, California, USA). With most of the neurosurgical community in first world nations now comfortable with these services, the geographical barrier that once isolated physicians in developing nations from those in developed nations has been shattered. Today, a surgeon from Peru can email a surgeon in a developed nation and reasonably expect that recipient to be comfortable joining a virtual call through which an insightful discussion can be facilitated. To understand the extent to which this cultural change can be scaled, it is helpful to look at how academic centers have changed in the last few months: at institutions such as Johns Hopkins, neurosurgical faculty, residents, postdoctoral fellows, and 4th year medical students spent the pandemic regularly presenting on an array of educational topics, including neuroanatomy, case conferences, and journal clubs, with surges in educational session attendance.[
An important consideration for future neurosurgical outreach models is the language barriers that may be faced on arrival at a new region. For these three missions, the senior member of the visiting team was conversant in medical Spanish, effectively resolving this barrier by serving as a communication bridge. To prevent communication from being lost in translation, teaching sessions involved several presentations, with videos of cases and complication management, that provided an opportunity for digital operative collaboration.[
Short-term surgical missions, as described in one investigation, are reputed for not addressing the root cause of health issues and, as a consequence, failing to provide appropriate solutions.[
A major limitation of the investigation is the relatively narrow definition of “operative skill transfer.” As most children (55%) were lost to follow-up and the remaining children had a short term follow-up duration, we do not have a comprehensive assessment to verify whether the operations led to durable results. While in the 5-year follow-up there was a great deal of uncertainty as to whether shunt replacement was avoided in the long run, the qualitative insights that have been gathered from the two visits in 2011 and 2015, as well as the digital communication, serve to indicate that shunts were entirely displaced as neuroendoscopic procedures became more routinely used. That said, we can now extend the conclusion of the original 5-year follow-up: the technical aspects of endoscopic procedures were effectively transferred to host neurosurgeons, and this transfer was clinically effective in Peru, given the minute proportion of surgical complications.
With the evolving economic and political landscape of Peru, a number of concerns remain. As faculty retire or move to other institutions, the acquired neuroendoscopic skill should continue to be passed on to junior surgeons to sustain the impact and ensure that sufficient neurosurgical care is available. Second, as equipment deteriorates, there may be a need for funding that is not available – to address this, the visiting and host teams should remain in touch to ensure that safeguards are in place to replace worn equipment and preserve the skill set and neuroendoscopic capacity of the institution. In parallel with the promising results of the 5-year follow-up, the results of the 15-year follow-up illustrate the efficacy and replicability of the described pediatric neurosurgery outreach model at positively shaping the landscape of global surgical care. It is expected that over time, as technology becomes increasingly utilized for international collaboration, the deficit in neurosurgical care will be reduced, especially when complemented with similar neurosurgical outreach missions. To further assess the efficacy and replicability of this model, data over the next decade will be examined. If operative skill can continue to be transferred to junior surgeons, a conclusion can be made as to whether the neurosurgical outreach missions left an impact that can be generationally felt, evolving the surgical skill set of the region in a self-sustaining manner.
CONCLUSION
With the major deficit in surgical care plaguing developing regions, it is essential that efforts devoted towards enhancing international surgical care be optimized such that allocated resources are most effectively and efficiently delivered. The didactic framework described above provides a means of empowering developing regions with the capacity to resolve emergent situations in the scope of pediatric neurosurgery, and can also be applied to enhance non-emergent medical care and elective care. In accordance with the data and previous success in Kiev, Ukraine using a similar framework, it should be recognized that the proposed international medical outreach design is replicable and should be built upon by future missions to impart a durable and substantial impact on developing regions. Utilizing the video-conferencing tools of the post COVID-19 hyperdigital age and centering outreach missions around the transmission of surgical knowledge, the skill set of host surgeons can be advanced in a fashion that can impact the region generationally. Shifting the focus of such missions from the provision of episodic, direct care from visiting surgeons to indigent citizens towards the provision of knowledge - passed along over time between resident classes at the host institution and sustained beyond the duration of the mission - provides a means of closing enormous gaps in accessibility to care and quality of care.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Commentary
In 1803, King Charles IV of Spain was persuaded by Dr. Balmis to organize an expedition to immunize against smallpox the children of America and the Philippines. What was then Spain is now a conglomerate of academic institutions, government agencies, and non-governmental organizations, all of these endeavors gathered under the code-name of Global Health.
Today, the prospect of cooperation on health issues between high-income countries (HIC) and low and middle-income countries (LMIC) changed. Nonetheless, a fundamental concept persists, the metropolis stores, control, and spreads knowledge. Not by coincidence, even in the XXI century, the preeminent schools of Tropical Medicine are in London, Paris, and Antwerp.
While we live in a time that reminds us of the importance of transmissible diseases, the unalterable fact is that once the current pandemic wave is controlled, and it will be, we will notice, again, that neurological disorders represent the most significant number of Days Living with Disability in any region but Sub-Saharan Africa.
Clinical neuroscientists in general and neurosurgeons in particular from academic institutions in high-income countries responded to the call with an enviable spirit of international cooperation. For a long while, numerous surgical missions from HIC visited LMIC to perform surgical procedures, often with minimal participation by colleagues from the host nations. A well-intentioned model that does not address structural issues such as continuity of care, technical development adequate to the reality of the specific country, and, damagingly to Global Health, the mission model of cooperation ignores the insight and wealth of empirical knowledge of the host neurosurgeon. In publications about the experience gathered in such ventures authored by the visiting team from a HIC, the local physicians are minimally represented in the author’s roster. Seldom, if ever, the relevance of the health care workers LMIC have been emphasized as a matter of concern by the Global Health planners. Of note, upon arriving in the Americas, Dr. Balmis discovered that local physicians, aware of Jenner’s work, started a vaccination program.
This paper embraces the concept that charity is vertical and solidarity is horizontal. Implicit in the intention of the authors is a profound respect for their colleagues.
Surgical Neurology International is a pioneer in providing a platform for the contributions of colleagues from all regions of the world. I am confident that the whole body of neurosurgery will profit from the flow of ideas, innovations as well as tacit and empirical clinical pearls that will come from our Peruvian and Ukrainian colleagues.
Jorge Lazareff, MD
University of California at Los Angeles
Los Angeles, CA, USA
JLazareff@mednet.ucla.edu
References
1. Anderson FW, Wansom T. Beyond medical tourism: Authentic engagement in global health. Virtual Mentor. 2009. 11: 506-10
2. Blankstein U, Dakurah T, Bagan M, Hodaie M. Structured online neurosurgical education as a novel method of education delivery in the developing world. World Neurosurg. 2011. 76: 224-30
3. Bosenberg AT. Pediatric anesthesia in developing countries. Curr Opin Anaesthesiol. 2007. 20: 204-10
4. Dewan MC, Rattani A, Fieggen G, Arraez MA, Servadei F, Boop FA. Global neurosurgery: The current capacity and deficit in the provision of essential neurosurgical care. Executive Summary of the Global neurosurgery initiative at the program in global surgery and social change. J Neurosurg. 2019. 130: 1055-64
5. Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery. 1998. 43: 294-303
6. Duenas VJ, Hahn EJ, Aryan HE, Levy MV, Jandial R. Targeted neurosurgical outreach: 5-year follow-up of operative skill transfer and sustainable care in Lima, Peru. Childs Nerv Syst. 2012. 28: 1227-31
7. Emergency and Essential Surgical Care. Available from: https://www.who.int/surgery/en [Last accessed on 2020 Dec 10].
8. Furr MC, Larkin E, Blakeley R, Albert TW, Tsugawa L, Weber SM. Extending multidisciplinary management of cleft palate to the developing world. J Oral Maxillofac Surg. 2011. 69: 237-41
9. Goyal N, Venkataram T, Dash C, Chandra PP.editors. Letter to the editor regarding: Impact of COVID-19 on an academic neurosurgery department: The Johns Hopkins experience. World Neurosurg. 2020. 143: 599-600
10. Hayden MG, Hughes S, Hahn EJ, Aryan HE, Levy ML, Jandial R. Maria Auxiliadora Hospital in Lima, Peru as a model for neurosurgical outreach to international charity hospitals. Childs Nerv Syst. 2011. 27: 145-8
11. Hollier LH, Sharabi SE, Koshy JC, Schafer ME, O’Young J, Flood TW. Surgical mission (not) impossible-now what?. J Craniofac Surg. 2010. 21: 1488-92
12. Kato Y, Liew BS, Sufianov AA, Rasulic L, Arnautovic KI, Dong VH. Correction to: Review of global neurosurgery education: Horizon of neurosurgery in the developing countries. Chin Neurosurg J. 2020. 6: 30
13. Kynes J, Zeigler L, Mcqueen K. Surgical outreach for children by international humanitarian organizations: A review. Children (Basel). 2017. 4: 53
14. Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA. Global surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015. 386: 569-624
15. Montgomery LM. Short-term medical missions: Enhancing or eroding health?. Missiology. 1993. 21: 333-41
16. Riviello R, Lipnick MS, Ozgediz D. Medical missions, surgical education, and capacity building. J Am Coll Surg. 2011. 213: 572
17. Sneag DB, Schaaf HS, Cotton MF, Zar HJ. Failure of chemoprophylaxis with standard antituberculosis agents in child contacts of multidrug-resistant tuberculosis cases. Pediatr Infect Dis J. 2007. 26: 1142-6
18. Suchdev P, Ahrens K, Click E, Macklin L, Evangelista D, Graham E. A model for sustainable short-term international medical trips. Ambul Pediatr. 2007. 7: 317-20
19. Warf BC, Alkire BC, Bhai S, Hughes C, Schiff SJ, Vincent JR. Costs and benefits of neurosurgical intervention for infant hydrocephalus in Sub-Saharan Africa. J Neurosurg Pediatr. 2011. 8: 509-21
20. Warf BC, Dagi AR, Kaaya BN, Schiff SJ. Five-year survival and outcome of treatment for postinfectious hydrocephalus in Ugandan infants. J Neurosurg Pediatr. 2011. 8: 502-8
21. Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR. An estimation of the global volume of surgery: A modelling strategy based on available data. Lancet. 2008. 372: 139-44
22. Won E, Ancona M, Carrigan K, Laverty B, Rhee P. Humanitarian aid mission in East Timor: Experiences of U.S. Naval medical services. Mil Med. 2006. 171: 29-36
23. Global Health Observatory (GHO) Data-Under-Five Mortality. Available from: http://www.who.int/gho [Last accessed on 2016 Dec 12].
24. Zeitler DM. Education paramount in surgical missions to developing countries. Otolaryngol Head Neck Surg. 2011. 144: 298