- Department of Neurosurgery, Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan.
- Department of Neurosurgery, The Aga Khan University Hospital, Karachi, Sindh, Pakistan.
Correspondence Address:
Asad Abbas
Department of Neurosurgery, The Aga Khan University Hospital, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_167_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Farrukh Javeed, Asad Abbas, Lal Rehman, Syed Raza Khairat Rizvi, Ali Afzal, Hafiza Fatima Aziz. Outcome of cranial firearm injuries in civilian population based on a novel classification system. 27-Jun-2020;11:167
How to cite this URL: Farrukh Javeed, Asad Abbas, Lal Rehman, Syed Raza Khairat Rizvi, Ali Afzal, Hafiza Fatima Aziz. Outcome of cranial firearm injuries in civilian population based on a novel classification system. 27-Jun-2020;11:167. Available from: https://surgicalneurologyint.com/surgicalint-articles/10103/
Abstract
Background: Cranial firearm injuries (CFAIs) are expected to be frequent during warfare; however, it is becoming increasingly common among civilian population in our part of the world. These injuries are associated with significant morbidity and mortality in addition to financial loss. The objective of our study is to evaluate the pattern of gunshot injuries to cranium and their outcome.
Methods: The study was conducted on 114 patients presenting with CFAIs to Jinnah Postgraduate Medical Centre, Karachi, Pakistan, between June 2015 and January 2019. Patients were evaluated with respect to age, gender, pattern of injury, Glasgow coma scale on arrival, radiological and clinical assessment, surgical intervention, and Glasgow outcome score measured at 6 months follow-up.
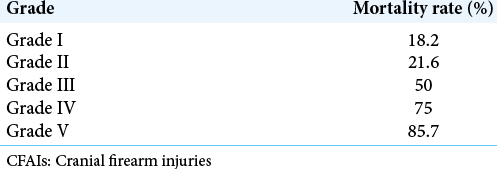
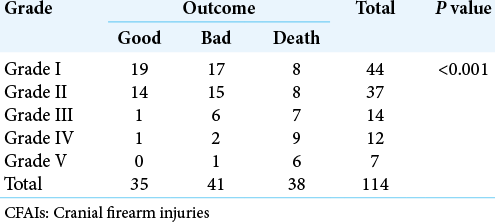
Results: Among patients with cranial gunshot, injuries most were males (76.3%). More than 50% patients aged between 18 and 35 years. About 46.5% of patients presented with moderate traumatic brain injury commonly involving the temporal lobe (36.8%). Of total 114 patients, 84.2% were managed conservatively but wound debridement was done in all patients. At 6 months, the overall mortality in our patients was 33.3%. Patients with good outcome (GOS 4 and 5) were 30.7% and 35.9% patients had bad outcome (GOS 2 and 3). Complication rate was 14.9% and the most common complication was disseminated intravascular coagulation in 5.2%.
Conclusion: Surgical intervention has no significant benefit over conservative management on long-term mortality and should be limited to patients with large intracranial hematomas and intraventricular hematomas causing hydrocephalus.
Keywords: Ballistics, Civilian population, Firearm injuries, Glasgow outcome score, Jinnah classification
INTRODUCTION
Firearm injuries (FAIs) are rare causes of head trauma in civilians; however, its incidence is on the rise worldwide. Being part of the war against terrorism, cranial FAIs (CFAIs) have also increased over the past two decades in Pakistan. This increase is seen not only in the war zones or militarized areas but also in the civilian population. In mortality due to head trauma, the contribution of FAI is about 14% and the most common involved regions are head and neck.[
Damage caused by FAIs depends on the missile velocity. Large and distant tissue damage in the brain is usually caused by the missiles moving at high velocity usually >3000 ft/s. The extend of brain damage does not depend on the track of the missile only but also on the surrounding tissue damage caused by the shockwaves. On the other hand, lesser and limited damage is caused by the missiles moving at low velocity, mainly by direct crushing and laceration of the brain tissue.[
In general, bad prognostic factors for CFAIs are very low GCS score on admission or path of firearm crossing the midline or ventricles.[
MATERIALS AND METHODS
A total of 114 patients of all ages and gender with CFAIs admitted in the department of neurosurgery through emergency department, were enrolled in the study. All patients were followed prospectively from June 2015 to January 2019. Patients with CFAIs who were received dead at the neurosurgery department, patients with no penetration of cranial vault and with FAIs involving other parts of the body and patients who were lost to follow-up, were excluded from the study. Demographic and clinical data were obtained including age, gender, mechanism of firearm, severity of traumatic brain injury, site of brain involvement, type of treatment provided, complications, and outcome.
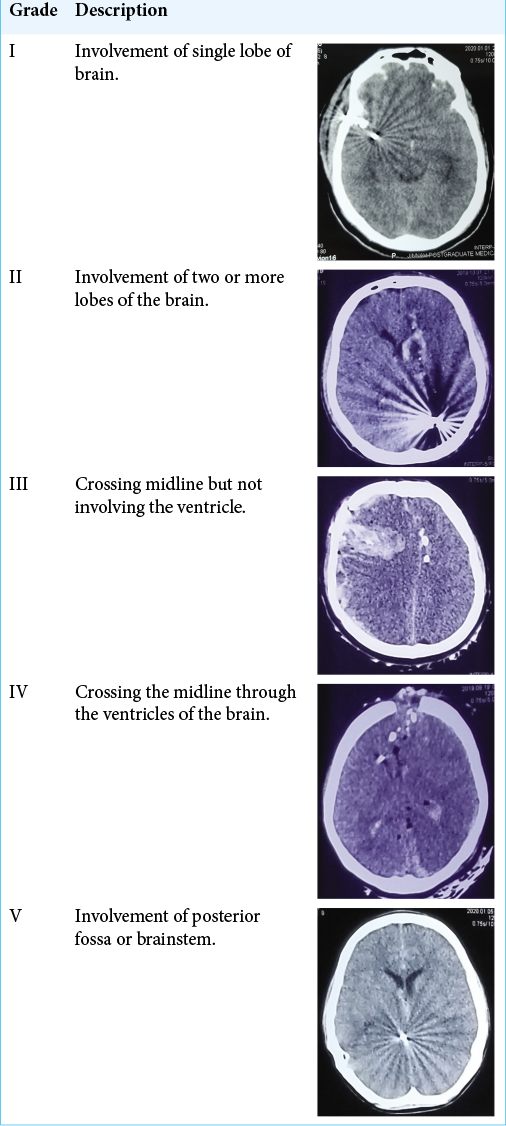
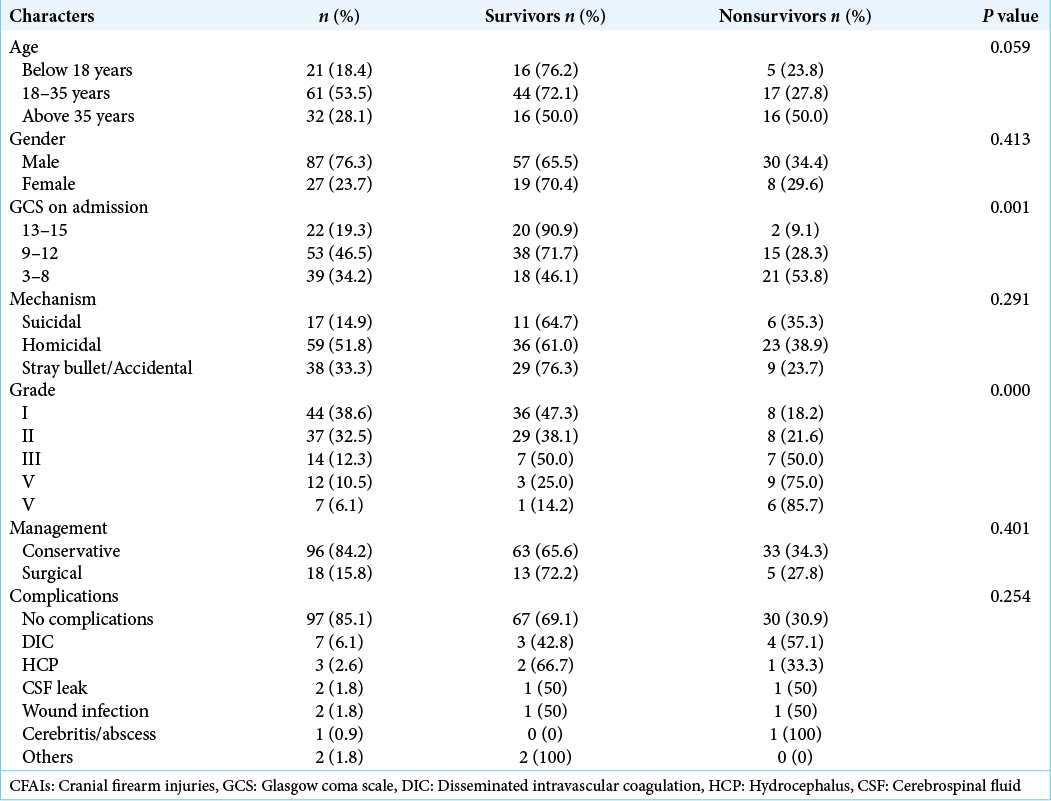
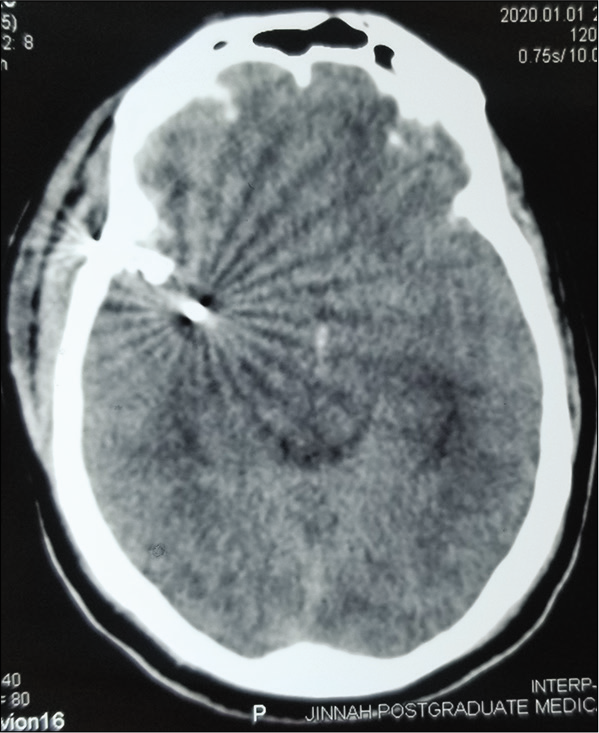
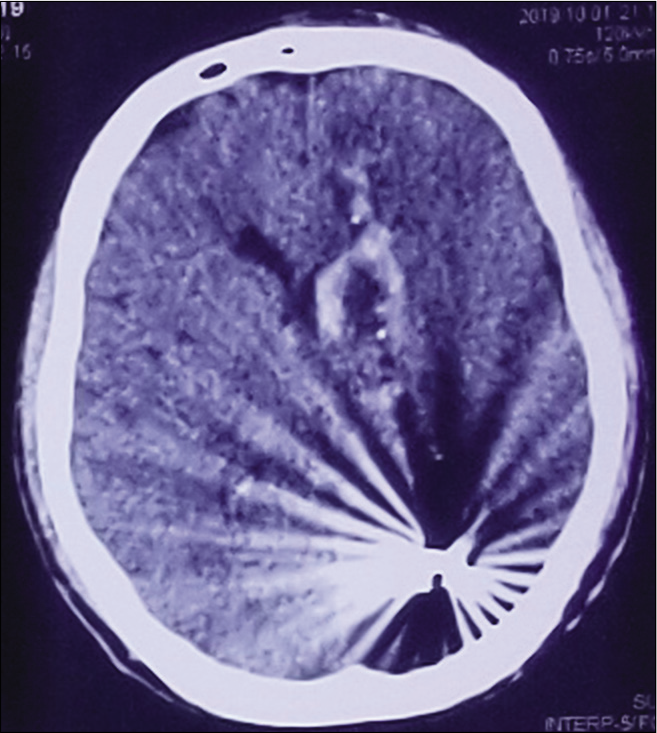
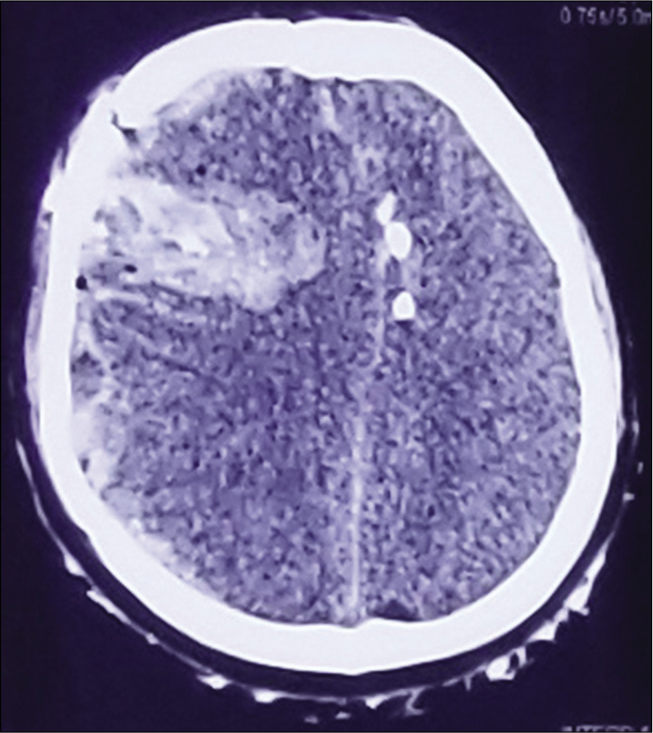
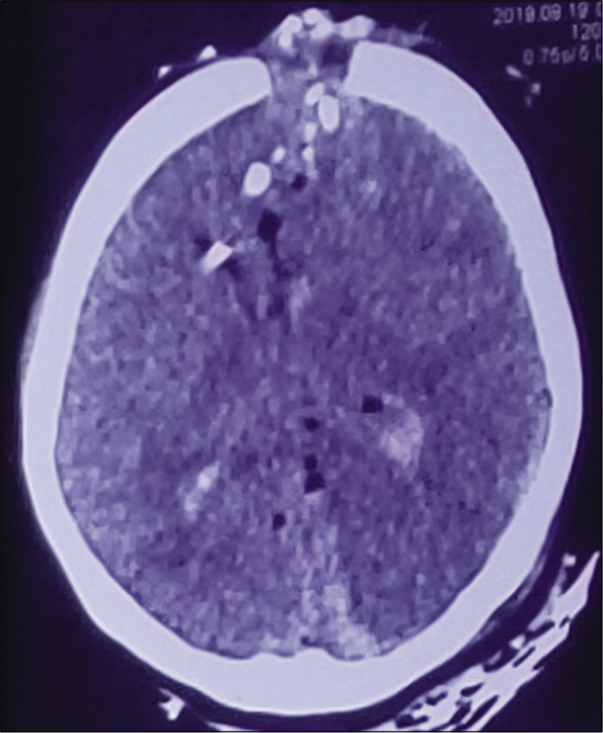
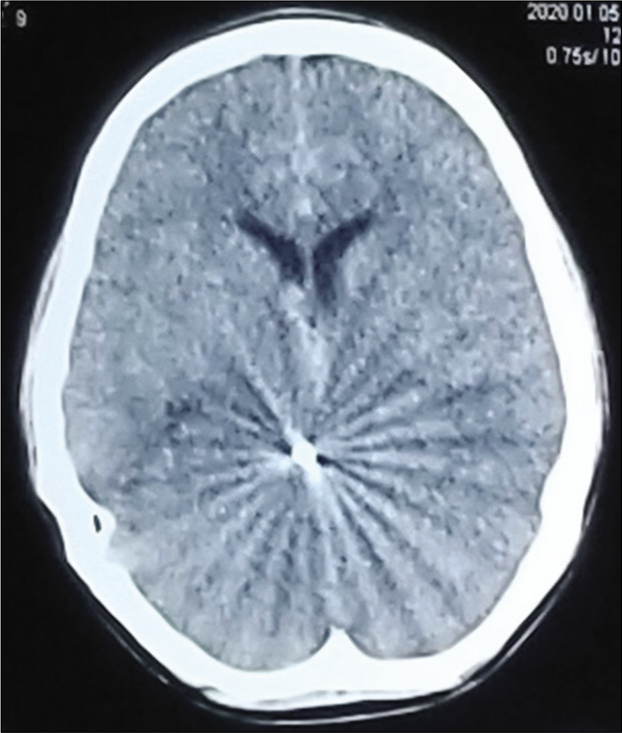
The patients with the CFAIs were categorized into three categories of traumatic brain injury severity according to the GCS; mild (GCS 13–15), moderate (GCS 9–12), and severe (GCS 3–8). The mechanism of firearm was categorized in suicidal, homicidal, and stray/accidental. Computed tomography (CT) scan was performed for all patients before admission and reviewed by two consultant neurosurgeons to identify their injury pattern. All patients were admitted in high dependency unit or intensive care unit. A need for a simple classification system to categorize these CFAIs was felt. To address that we would like to propose a CT scan based classification system for CFAIs (naming after our institute) to grade these injuries in reference to the areas of the brain involved as given in [
Management was divided into conservative and surgical treatment. Conservative treatment was comprised of wound debridement and medical treatment. Hematoma evacuation, placement of external ventricular drain, decompression with removal of missile, and bone fragments were taken as the surgical treatment. All patients who survived with neurological deficit were either discharged to home based nursing care or referred to rehabilitation centers. Follow-up at regular intervals for up to 6 months and outcome analysis was performed on Glasgow outcome score (GOS) at final follow-up. Frequency and types of secondary complication were also noted. SPSS version 23 was used for the statistical analysis. Means were calculated for all continuous variables whereas frequencies and percentages for all categorical variables. Chi-square test was used to assess the outcome with respect to the severity of head trauma, CFAIs grade, and type of management provided (surgical vs. conservative).
RESULTS
In our study, age of patients with CFAIs ranged from 6 years to 58 years but common age group affected was between 18 and 35 years of age [
Most patients (84.2%) were managed conservatively but wound debridement was done in all of them. Good outcome was seen in 35(30.7%) patients with CFAIs and poor outcome (GOS 2–3) in 41 (36.0%) patients. A total of 38 (33.4%) patients brought with the CFAIs died, of which 31 patients died within the hospital during treatment and seven died after the discharge. Mean hospital stay was 9.12 days in our study. Total 17 patients developed complications, most common being the disseminated intravascular coagulation (DIC) in six (5.2%) followed by hydrocephalus (HCP) in four (3.5%) patients.
DISCUSSION
In neurosurgical practice, CFAIs are one of the less common causes of head injuries; however, it carries higher morbidity and mortality. Studies have shown that the common age group admitted with CFAIs is usually patients 20–35-year-old and male.[
Social and cultural factors can be seen as we probe the mechanism of FAIs. The majority of FAIs were homicidal (51.8%) but stray/accidental FAIs also contributed a significant number of cases (33.3%). One formal study showed the similar pattern with 67.2% homicide cases.[
Initial investigation of choice for all the traumatic head injuries including FAIs, is CT scan and it is noted that its findings are correlated to prognosis.[
We observed that Grade I CFAIs (single lobe involvement) was the most common (39%) patients and temporal lobe was the most commonly involved lobe (36.8%). In contrast, one study showed the frontal lobe as the most frequently injured brain region (32.8%).[
There is high variability seen among former studies regarding the mortality rates, one showing very low mortality rates of 7.7% while other having as high as 93% and many falling in between.[
In our study, 17 (14.9%) patient developed complications. Among these patients, the most common complication was DIC in 5.2%, followed by HCP in 3.5% and cerebrospinal fluid leak in 1.8%. In comparison, one formal study showed paresis in 16.8% as the most common complication.[
Formal studies show different results about the prognostic value of the age in CFAIs, with few showing that increasing age is a good prognostic factor while others showing the opposite results.[
Various studies have shown that poor prognosis was seen in CFAIs with interventricular hemorrhages and extent of brain injuries.[
CONCLUSION
FAIs are one of the fatal cranial injuries and need a specialized and prolonged in-hospital and posthospital medical care. Good GCS on admission, low CFAIs grade and selective surgical intervention are the important factors for a good outcome in these patients. Jinnah CFAI classification can be a simple way to classify the CT scan findings and predict the outcome but further work and validation is needed in the form of larger multi-centric studies.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Aarabi B, Tofighi B, Kufera JA, Hadley J, Ahn ES, Cooper C. Predictors of outcome in civilian gunshot wounds to the head. J Neurosurg. 2014. 120: 1138-46
2. Aldrich EF, Eisenberg HM, Saydjari C, Foulkes MA, Jane JA, Marshall LF. Predictors of mortality in severely head-injured patients with civilian gunshot wounds: A report from the NIH traumatic coma data bank. Surg Neurol. 1992. 38: 418-23
3. Aras M, Altaş M, Yilmaz A, Serarslan Y, Yilmaz N, Yengil E. Being a neighbor to Syria: A retrospective analysis of patients brought to our clinic for cranial gunshot wounds in the Syrian civil war. Clin Neurol Neurosurg. 2014. 125: 222-8
4. Bakir A, Temiz C, Umur S, Aydin V, Torun F. High-velocity gunshot wounds to the head: Analysis of 135 patients. Neurol Med Chir (Tokyo). 2005. 45: 281-7
5. Beauthier JP.editors. Trafficking in Legal Medicine. Brussels: Edition DeBoeck University; 2008. p.
6. Brandt F, Roosen K, Weiler G, Grote W. Neurosurgical management of gunshot injuries to the head. Neurochirurgia (Stuttg). 1983. 26: 164-71
7. Brandvold B, Levi L, Feinsod M, George ED. Penetrating craniocerebral injuries in the Israeli involvement in the Lebanese conflict, 1982-1985. Analysis of a less aggressive surgical approach. J Neurosurg. 1990. 72: 15-21
8. Çınar K, Seçer M, Alagöz F, Ulutaş M, Uçkun OM, Yıldırım AE. Outcomes and demostration of cranial firearm injuries: A multicenter retrospective study. Ulus Travma Acil Cerrahi Derg. 2015. 21: 291-6
9. Cirak B, Güven MB, Kiymaz N, Işik S. Cranial gunshot injuries and treatment approaches. Ulus Travma Derg. 2000. 6: 241-3
10. Di Maio VJ.editors. Gunshot Wounds; Practical Aspects of Firearms, Ballistics, and Forensic Techniques. New York, Boca Raton: CRC Press; 1999. p.
11. Fedakar R, Gündoğmuş UN, Türkmen N. Firearm-related deaths in two industrial cities of Turkey and their province. Leg Med (Tokyo). 2007. 9: 14-21
12. Goren S, Subasi M, Tirasci Y, Kemaloglu S. Firearm-related mortality: A review of four hundred-forty four deaths in Diyarbakir, Turkey between 1996 and 2001. Tohoku J Exp Med. 2003. 201: 139-45
13. Grahm TW, Williams FC, Harrington T, Spetzler RF. Civilian gunshot wounds to the head: A prospective study. Neurosurgery. 1990. 27: 696-700
14. Hoppe IC, Kordahi AM, Paik AM, Lee ES, Granick MS. Pediatric facial fractures as a result of gunshot injuries: An examination of associated injuries and trends in management. J Craniofac Surg. 2014. 25: 400-5
15. Kaufman HH, Makela ME, Lee KF, Haid RW, Gildenberg PL. Gunshot wounds to the head: A perspective. Neurosurgery. 1986. 18: 689-95
16. Kim TW, Lee JK, Moon KS, Kwak HJ, Joo SP, Kim JH. Penetrating gunshot injuries to the brain. J Trauma. 2007. 62: 1446-51
17. Levy ML, Rezai A, Masri LS, Litofsky SN, Giannotta SL, Apuzzo ML. The significance of subarachnoid hemorrhage after penetrating craniocerebral injury: Correlations with angiography and outcome in a civilian population. Neurosurgery. 1993. 32: 532-40
18. Martins RS, Siqueira MG, Santos MT, Zanon-Collange N, Moraes OJ. Prognostic factors and treatment of penetrating gunshot wounds to the head. Surg Neurol. 2003. 60: 98-104
19. Miller JD, Butterworth JF, Gudeman SK, Faulkner JE, Choi SC, Selhorst JB. Further experience in the management of severe head injury. J Neurosurg. 1981. 54: 289-99
20. Nagib MG, Rockswold GL, Sherman RS, Lagaard MW. Civilian gunshot wounds to the brain: Prognosis and management. Neurosurgery. 1986. 18: 533-7
21. Önder A, Kadıoğlu HH, Aydın İH. Craniocerebral firearm injuries. Atatürk Üniv Medical Bulletin. 1991. 23: 201-10
22. Özkan U, Kemaloglu MS, Özates M, Aydin MD. Analysis of 107 civilian craniocerebral gunshot wounds. Neurosurg Rev. 2002. 25: 231-6
23. Paret G, Dekel B, Yellin A, Hadani M, Weissman D, Vardi A. Pediatric craniocerebral wounds from plastic bullets: Prognostic implications, course, and outcome. J Trauma. 1996. 41: 859-63
24. Quatrehomme G, Iscan MY. Analysis of bevelling in gunshot entrance wounds. J Forensic Sci Int. 1998. 93: 45-60
25. Quatrehomme G, Iscan MY. Bevelling in exit gunshot wounds in bones. Forensic Sci Int. 1997. 89: 93-101
26. Quatrehomme G, Iscan MY. Characteristics of gunshot wounds in the skull. J Forensic Sci. 1999. 44: 568-76
27. Quatrehomme G, Iscan MY. Gunshot wounds to the skull: Comparison of entries and exits. Forensic Sci Int. 1998. 94: 141-6
28. Raul JS, Deck C, Meyer F, Geraut A, Willinger R, Ludes B. A finite element model investigation of gunshot injury. Int J Legal Med. 2007. 121: 143-6
29. Shoung HM, Sichez JP, Pertuiset B. The early prognosis of craniocerebral gunshot wounds in civilian practice as an aid to the choice of treatment. A series of 56 cases studied by the computerized tomography. Acta Neurochir (Wien). 1985. 74: 27-30
30. Stone JL, Lichtor T, Fitzgerald LF. Gunshot wounds to the head in civilian practice. Neurosurgery. 1995. 37: 1104-12
31. Williams AJ, Ling GS, Tortella FC. Severity level and injury track determine outcome following a penetrating ballistic-like brain injury in the rat. Neurosci Lett. 2006. 408: 183-8
32. Yaman O, Dağlı AT, Güvercin AR, Kuzeyli K. Gunshot wound to head. Sinir Sistemi Cerrahisi Derg. 2014. 4: 69-73