- Department of Surgery, Division of Neurosurgery, College of Medicine, King Saud University, Riyadh, Saudi Arabia.
Correspondence Address:
Sarah Basindwah, Department of Surgery, Division of Neurosurgery, College of Medicne, King Saud University, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_1071_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulrazag Ajlan1, Rawan Alwadee1, Sarah Basindwah1, Badriah Alsabbagh1, Mohammed Hamad Alhumud1, Abdulaziz M. Alaskar1. Outcomes and complications of microscopic transcallosal colloid cyst resection: A single institution experience. 17-Mar-2023;14:88
How to cite this URL: Abdulrazag Ajlan1, Rawan Alwadee1, Sarah Basindwah1, Badriah Alsabbagh1, Mohammed Hamad Alhumud1, Abdulaziz M. Alaskar1. Outcomes and complications of microscopic transcallosal colloid cyst resection: A single institution experience. 17-Mar-2023;14:88. Available from: https://surgicalneurologyint.com/surgicalint-articles/12199/
Abstract
Background: Colloid cysts have always provoked the interest of neurosurgeons due to their benign histology, wide variety of clinical presentations, and differences in reported surgical outcomes. Although recent studies have reported favorable outcomes with different surgical resection approaches, the transcallosal approach remains the most popular approach to date. In this series, we report the clinical and radiological outcomes of the transcallosal approach for the resection of third ventricle colloid cysts in 12 patients.
Methods: We present a case series of 12 patients who were radiologically diagnosed with a third ventricle colloid cyst who underwent transcallosal resection by a single surgeon in one center over a 6-year period. Clinical, radiological, and surgical data were collected, and surgical outcomes and complications were analyzed.
Results: Of the 12 patients diagnosed with colloid cysts, 10 (83%) presented with headache, and five (41%) presented with memory disturbance. All 12 patients showed improvement or resolution of their symptoms following resection. Nine patients (75%) presented with hydrocephalus on radiology. All the patients required preoperative or intraoperative external ventricular drain insertion. Four patients (33%) experienced transient postoperative complications. None of the patients required long-term cerebrospinal fluids shunting. One (8%) of 12 patients experienced transient memory loss. No mortality was recorded during the follow-up.
Conclusion: Transcallosal resection of colloid cysts has a favorable prognosis. It allows for complete resection of the cyst with minimal transient postoperative complications. Most patients with postoperative complications show complete resolution of symptoms, with no long-term morbidity.
Keywords: Colloid cyst, Microsopic resection, Third ventricle tumor, Transcallosal approach
INTRODUCTION
Colloid cysts are benign lesions that originate from neuroectodermal tissue.[
MATERIALS AND METHODS
Study design and patient selection
Patients (n = 12) with third ventricle colloid cysts who underwent microscopic interhemispheric transcallosal resection of the colloid cyst between January 2015 and December 2021 by a single surgeon at one institution were enrolled. Patients who were managed by observation and serial follow-up, and those who underwent a different surgical approach were excluded from the study.
Data collection
We conducted a retrospective analysis of all neurosurgical operative records from King Saud University Medical City from January 2015 to December 2021. All medical and surgical records were accessed from the hospital electronic database. Demographic data, clinical presentation, surgical details, preoperative and postoperative neurological status, and radiological studies were collected and analyzed. The diagnosis of colloid cysts in all 12 patients was confirmed by expert histopathologists following surgical resection, and official reports of preoperative imaging and radiological follow-up were written by expert neuroradiologists. Postoperative outcomes were assessed at discharge, follow-up, and by telephone interviews. The mean follow-up period was 3.5 years.
Surgical approach
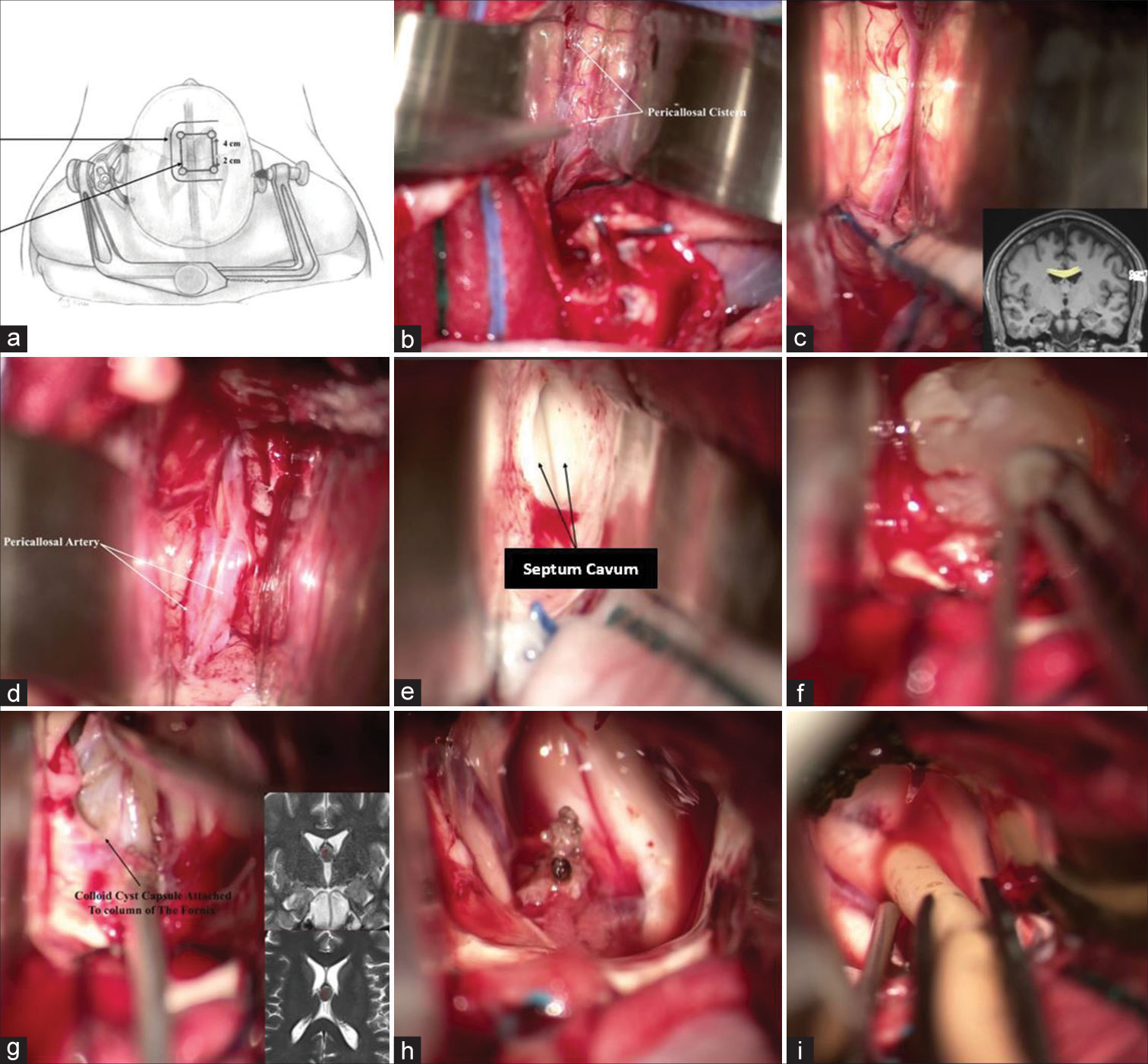
All surgeries were aided with magnetic resonance neuronavigation. The patient was placed in the supine position and the head was secured with a 3-point Mayfield head clamp and positioned neutrally in the sagittal plane with the neck flexed at 20° [
Figure 1:
Transcallosal approach to third ventricle colloid cyst resection. (a) Patient is laying supine with head fixed on a Mayfield clamp in neutral position showing the horseshoe incision and the craniotomy site, (b) Separation of the two hemispheres using malleable retractors to expose pericallosal cisterns, (c) Corpus callosum. (d) Pericallosal arteries, (e) Septum cavum, (f) Colloid cyst capsule excision, (g) Colloid cyst capsule attached to the column of the fornix, (h) Surgical field after cyst removal, (i) Insertion of external ventricular drains to clear postoperative debris.
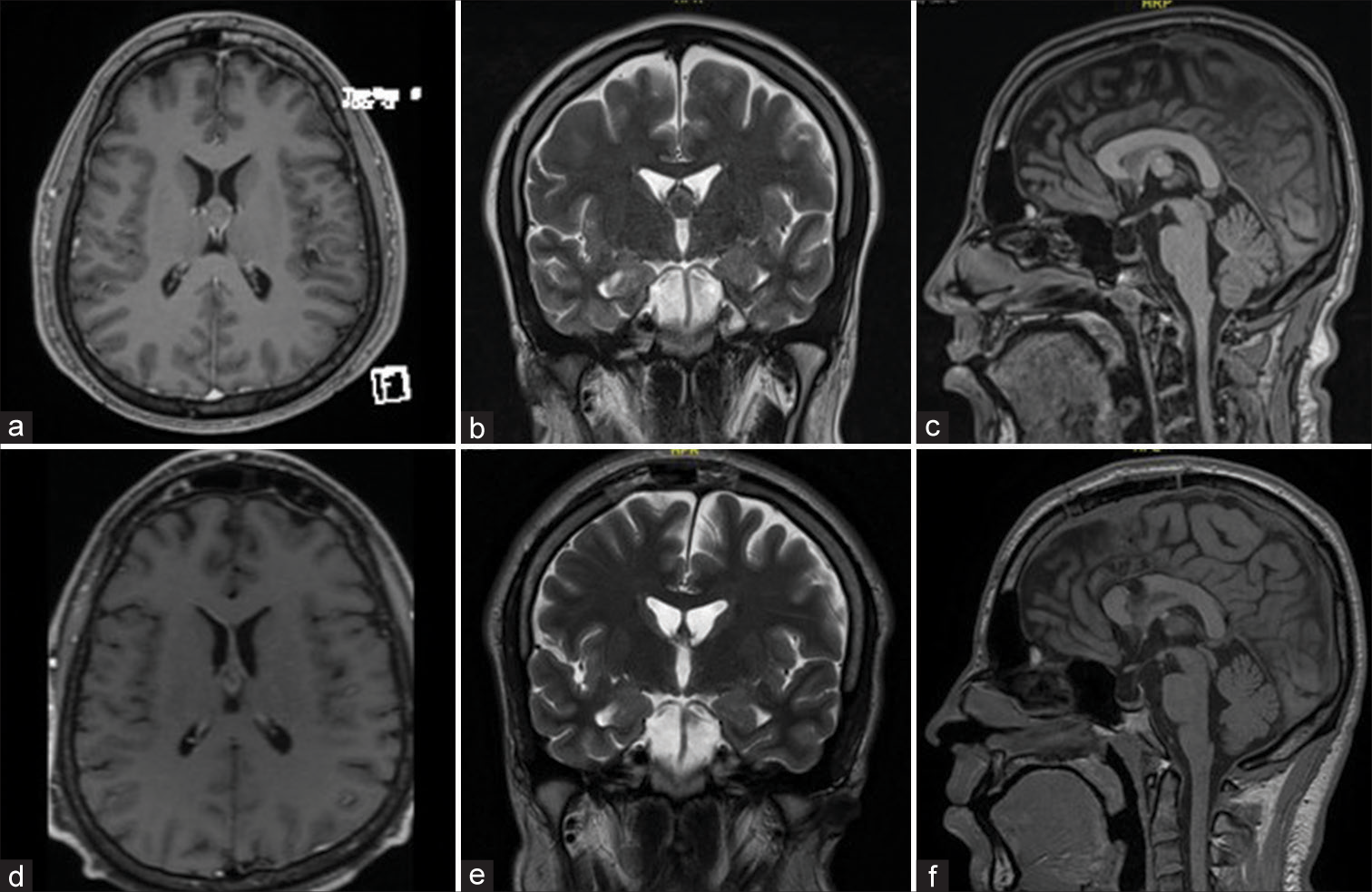
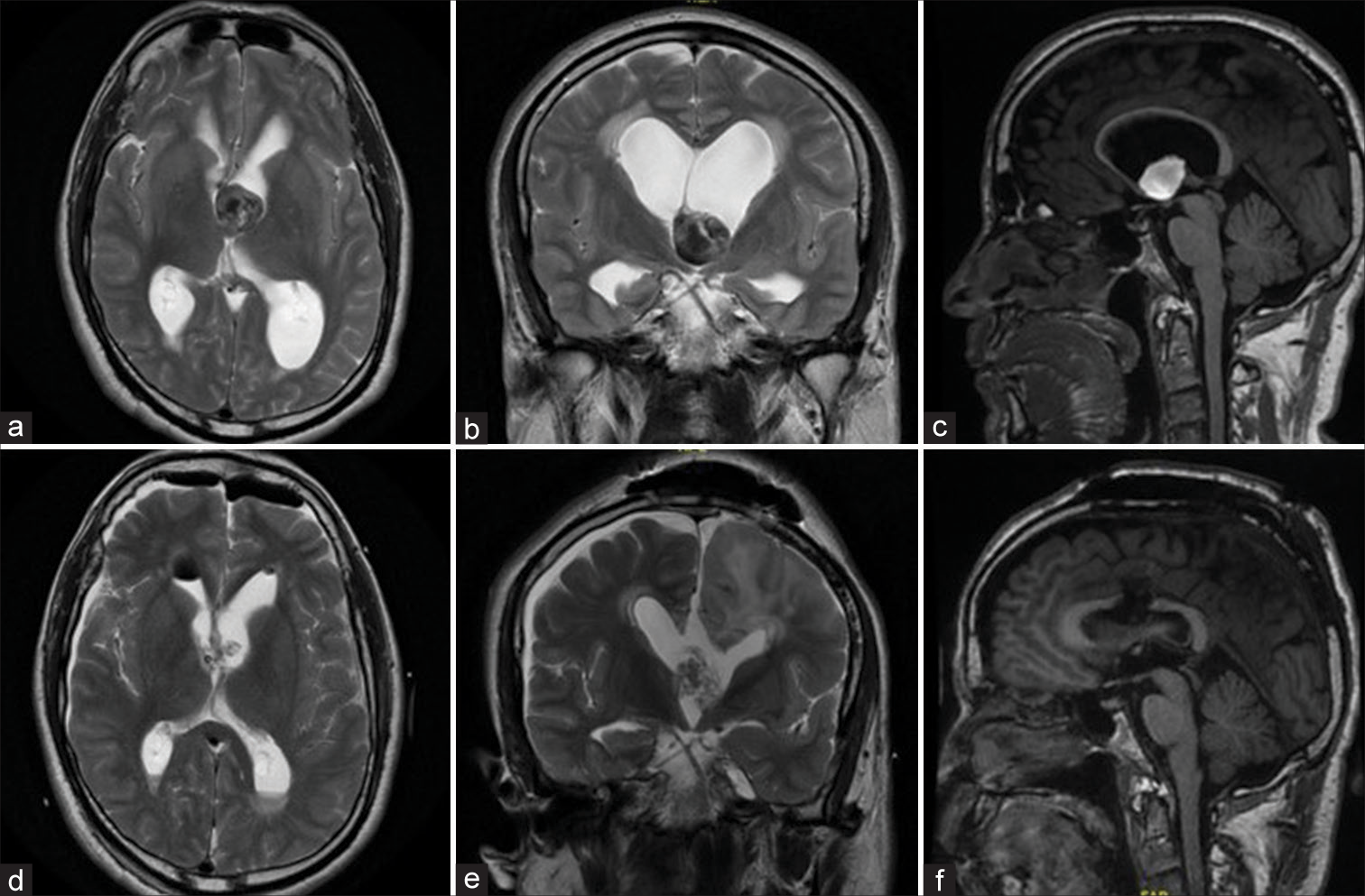
Figure 2:
(a) Axial T1-weighted image with contrast, (b) Coronal T2-weighted image, (c) Sagittal T1 weighted image of a third ventricle colloid cyst in a 22-year-old patient who presented with chronic headache and high ICP symptoms. (d) Axial T1-weighted image with contrast, (e) Coronal T2- weighted imgae, (f) Sagittal T1-weighted magnetic resonance imaging post transcallosal resection of the colloid cyst with resolution of the presenting symptoms.
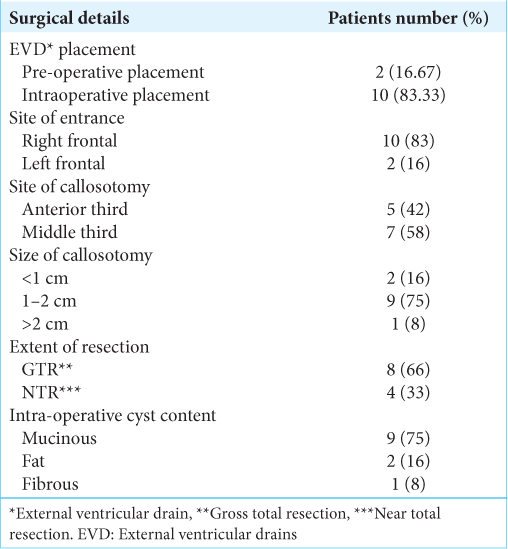
Neuronavigation was used to facilitate the best position for craniotomy and to protect the parasagittal bridging veins. The bone flap was made by placing four paramedian burr holes 1 cm lateral to the midline on either the right or left side and 2 cm lateral to the midline, exposing the superior sagittal sinus (SSS) to avoid risk of injury. The dura was then dissected from the inner table of the calvarium, taking special care of the exposed sinuses and was opened using a U-shaped flap based on the sagittal sinus. The sinus was pushed laterally to expand the interhemispheric fissure. A few small bridging veins may be sacrificed, but larger ones are preserved. The interhemispheric fissure was then opened and the Pericallosal Cistern dissection continued to deepen the exposure. Gentle retraction is applied using retractors to aid visualization and avoid retraction of the frontal lobe by more than 10–15 mm. After identifying the cingulate gyrus, it was sharply dissected both anteriorly and posteriorly. The ipsilateral callosomarginal artery was traced along the midline to the cingulum level. Pericallosal arteries were identified and carefully separated on each side of the midline avascular plane using the tip of micro-scissors. Furthermore, arachnoid dissection exposes the white corpus callosum. The callosotomy was then created with suction and bipolar cautery under low power in the midline between the paired pericallosal arteries. A fenestration of the septum pellucidum on the side of entry was performed to connect the ventricular systems. The opening was widened using a dissector and suction. Once satisfactory exposure is achieved, coagulation of the choroid plexus is performed to control bleeding. After identifying the capsule and attachment sites of the cyst, it was removed safely. Gross total resection was attempted in all cases where the capsule was completely removed. In a few cases where the capsule was attached to the contralateral fornix, a small part of the capsule was left to prevent neurocognitive deficits. The field was then thoroughly irrigated and hemostasis was achieved. All patients had a ventricular catheter inserted to clear debris that may be seen in the postoperative period which was removed on postoperative day 2. The dura was then closed in a watertight fashion taking care of the SSS, the bone flap was secured, and the galea and skin were closed as routine.
Data analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 24.0 software (SPSS Inc., Chicago, IL, USA). We calculated the frequencies and percentages of all nominal variables.
RESULTS
Presentation
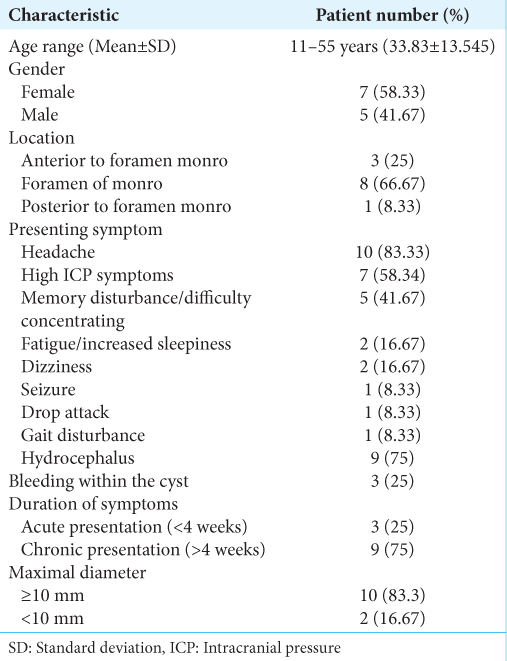
Twelve patients (aged 11–55 years old) were included in the case series. Seven patients (58%) were females and 5 patients (42%) were males [
Radiological findings
Three patients had blood in their colloid cysts. The size of the colloid cyst was >2 cm in all three patients, while the other nine patients had a colloid cyst size of ≤2 cm. All three patients presented with signs of high Intracranial pressure (ICP) and hydrocephalus on imaging.
Surgical approach
Two patients presented with acute onset headache, papilledema, and active hydrocephalus, requiring emergency placement of external ventricular drains (EVDs) to relieve the obstruction. They underwent the same surgical approach as the other ten patients and had a similar postoperative course, with removal of the EVD before discharge. Gross total resection was achieved in 8 (66%) of the 12 patients, 4 (33%) patients had a near total resection with a small (<2 mm) attachment of the capsule to the contralateral corpus callosum [
Postoperative outcome
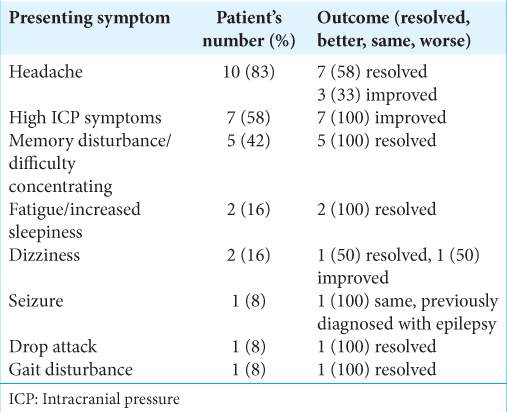
The patients’ follow-up periods ranged from 1 to 6 years (mean 3.5 years). In all 12 patients, 100% of the presenting symptoms attributed to the colloid cyst were either significantly improved or completely resolved at their postoperative follow-ups. Only three patients continued to have mild headaches, which significantly improved after surgery [
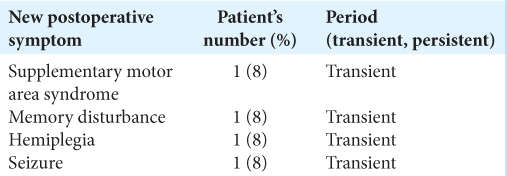
One patient developed supplementary motor area (SMA) syndrome manifesting as akinesia and mutism [
Figure 3:
(a-c) T2-weighted axial and coronal and sagittal T1-weighted magnetic resonance imaging (MRI) of 55-year-old gentleman presenting with vague headache, memory disturbance showing a large hemorrhagic third ventricle colloid cyst with obstructive hydrocephalus. (d-f) Postoperative follow-up axial and coronal T2-weighted and sagittal T1-weighted MRI showing significant encephalomalacia on the side of entry (right). The patient developed immediate postoperative mutism, hemiplegia, and seizure. His symptoms resolved few weeks postoperatively.
Another patient, who presented with acute high Intracranial pressure (ICP) symptoms, developed one episode of postoperative seizures. The patient underwent a 1.83 cm anterior third callosotomy. On follow-up, the patient was symptom-free and had no further episodes. A third patient developed new onset postoperative short-term memory disturbance and difficulty concentrating which was resolved by her first follow-up. Another patient had a transient left facial nerve upper motor neuron palsy and left hemiplegia. Postoperative images showed no obvious vascular insults, and a middle third callosotomy measuring 1.34 cm in length. Her symptoms improved on discharge and completely resolved on follow-up [
There was no mortality, meningitis, wound infection, SSS tearing or thrombosis, pericallosal artery injury, or disconnection syndrome. On postoperative imaging, there was no evidence of traction edema, infarction, or encephalomalacia in 11 of 12 patients. One patient had left-sided encephalomalacia apparent on MRI, which correlated with transient postoperative SMA syndrome.
DISCUSSION
Colloid cysts have always provoked the interest of neurosurgeons due to their benign histology, difficult anatomical location, variant clinical presentation, and relatively favorable prognosis. Throughout history, there has been a wide array of treatment options available for third ventricle colloid cysts.[
Over the past few decades, there has been a consensus regarding the complete resection of symptomatic colloid cysts. Asymptomatic colloid cysts are frequently resected because of the fear of acute ventricular obstruction and sudden death.[
The optimal surgical approach to reach and resect a third ventricle colloid cyst remains debatable.[
The transcallosal approach was first described in 1949 by Greenwood.[
A meta-analysis by Elshamy et al.[
Presenting symptoms
Colloid cysts are located in the anterior two-thirds of the third ventricle or foramen of Monro in 80% of patients.[
Postoperative outcome
The prognosis for colloid cysts after surgical excision is favorable.[
In our series, 1 patient (8%) developed SMA syndrome in the form of hemiparesis and mutism that completely resolved a few weeks after surgery. Mutism has been reported in the transcallosal approach and has not been attributed to partial callosotomy but to damage to surrounding structures such as the cingulate gyrus, wall of the third ventricle, and supplementary motor cortex.[
For callosotomy, the corpus callosum was incised in the midline between the pericallosal arteries for a length of 1.5–2.5 cm in the sagittal plane in the anterior corpus callosum. Larger incisions may impair interhemispheric functions and cause disconnection-like syndrome.[
Our series was limited by its retrospective nature and small sample size. Many of the postoperative symptoms in the transcallosal approach affect more complex functions of the brain, which are difficult to measure. In this series, physical examination and subjective observations from patients during follow-up and phone interviews were used to evaluate symptom improvement, which may be susceptible to recall bias. Neurocognitive function testing was not performed in this patient group given the retrospective study design. A larger patient sample with more precise examination tools to measure postoperative outcomes is required.
CONCLUSION
Transcallosal resection of colloid cysts has a favorable prognosis. It allows for complete resection of the cyst with minimal transient postoperative complications. Most patients with postoperative complications show complete resolution of symptoms, with no long-term morbidity.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alkhaibary A, Baydhi L, Alharbi A, Alshaikh AA, Khairy S, Abbas M. Endoscopic versus open microsurgical excision of colloid cysts: A comparative analysis and state-of-theart review of neurosurgical techniques. World Neurosurg. 2021. 149: e298-308
2. Beaumont TL, Limbrick DD, Rich KM, Wippold FJ, Dacey RG. Natural history of colloid cysts of the third ventricle. J Neurosurg. 2016. 125: 1420-30
3. Bellotti C, Pappada G, Sani R, Oliveri G, Stangalino C. The transcallosal approach for lesions affecting the lateral and third ventricles. Acta Neurochir (Wien). 1991. 111: 103-7
4. Boogaarts HD, Decq P, Grotenhuis JA, Le Guérinel C, Nseir R, Jarraya B. Long-term results of the neuroendoscopic management of colloid cysts of the third ventricle: A series of 90 cases. Neurosurgery. 2011. 68: 179-87
5. Brain WR. Diseases of the Nervous System. London: Oxford University Press; 1951. 389: 10-20
6. Camacho A, Abernathey CD, Kelly PJ, Laws ER. Colloid cysts: Experience with the management of 84 cases since the introduction of computed tomography. Neurosurgery. 1989. 24: 693-700
7. Chibbaro S, Champeaux C, Poczos P, Cardarelli M, Di Rocco F, Iaccarino C. Anterior trans-frontal endoscopic management of colloid cyst: An effective, safe, and elegant way of treatment. Case series and technical note from a multicenter prospective study. Neurosurg Rev. 2014. 37: 235-41
8. Dandy WE. Diagnosis, localization and removal of tumors of the third ventricle. Bull Johns Hopkins Hosp. 1922. 33: 188-9
9. Desai KI, Nadkarni TD, Muzumdar DP, Goel AH. Surgical management of colloid cyst of the third ventricle-a study of 105 cases. Surg Neurol. 2002. 57: 295-302
10. Elshamy W, Burkard J, Gerges M, Erginoglu U, Aycan A, Ozaydin B. Surgical approaches for resection of third ventricle colloid cysts: Meta-analysis. Neurosurg Rev. 2021. 44: 3029-38
11. Greenwood J. Paraphysial cysts of the third ventricle: With report of eight cases. J Neurosurg. 1949. 6: 153-9
12. Hernesniemi J, Leivo S. Management outcome in third ventricular colloid cysts in a defined population: A series of 40 patients treated mainly by transcallosal microsurgery. Surg Neurol. 1996. 45: 2-14
13. Hernesniemi J, Romani R, Dashti R, Albayrak BS, Savolainen S, Ramsey C. Microsurgical treatment of third ventricular colloid cysts by interhemispheric far lateral transcallosal approach-experience of 134 patients. Surg Neurol. 2008. 69: 447-53
14. Horn EM, Feiz-Erfan I, Bristol RE, Lekovic GP, Goslar PW, Smith KA. Treatment options for third ventricular colloid cysts: Comparison of open microsurgical versus endoscopic resection. Neurosurgery. 2007. 60: 613-20
15. Konovalov AN, Pitskhelauri DI, Shkarubo M, Buklina SB, Poddubskaya AA, Kolycheva M. Microsurgical treatment of colloid cysts of the third ventricle. World Neurosurg. 2017. 105: 678-88
16. Little JR, MacCarty CS. Colloid cysts of the third ventricle. J Neurosurg. 1974. 40: 230-5
17. Nair S, Gopalakrishnan CV, Menon G, Easwer HV, Abraham M. Interhemispheric transcallosal transforaminal approach and its variants to colloid cyst of third ventricle: Technical issues based on a single institutional experience of 297 cases. Asian J Neurosurg. 2016. 11: 292-7
18. Nakasu Y, Isozumi T, Nioka H, Handa J. Mechanism of mutism following the transcallosal approach to the ventricles. Acta Neurochir (Wien). 1991. 110: 146-53
19. Sethi A, Cavalcante D, Ormond DR. Endoscopic versus microscopic transcallosal excision of colloid cysts: A systematic review in the era of complete endoscopic excision. World Neurosurg. 2019. 132: e53-8
20. Sheikh AB, Mendelson ZS, Liu JK. Endoscopic versus microsurgical resection of colloid cysts: A systematic review and meta-analysis of 1278 patients. World Neurosurg. 2014. 82: 1187-97
21. Symss NP, Ramamurthi R, Kapu R, Rao SM, Vasudevan MC, Pande A. Complication avoidance in transcallosal transforaminal approach to colloid cysts of the anterior third ventriclen: An analysis of 80 cases. Asian J Neurosurg. 2014. 9: 51-7
22. Symss NP, Ramamurthi R, Rao SM, Vasudevan MC, Jain PK, Pande A. Management outcome of the transcallosal, transforaminal approach to colloid cysts of the anterior third ventricle: An analysis of 78 cases. Neurol India. 2011. 59: 542-7