- Department of Neurosurgery, Salford Royal NHS Foundation Trust, Salford, Greater Manchester, United Kingdom.
Correspondence Address:
Ahmed Zanaty, Department of Neurosurgery, Salford Royal NHS Foundation Trust, Salford, Greater Manchester, United Kingdom.
DOI:10.25259/SNI_371_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Zanaty, K. Joshi George. Outcomes and efficiency of managing patients admitted for surgery for spinal metastases. 22-Jul-2022;13:312
How to cite this URL: Ahmed Zanaty, K. Joshi George. Outcomes and efficiency of managing patients admitted for surgery for spinal metastases. 22-Jul-2022;13:312. Available from: https://surgicalneurologyint.com/surgicalint-articles/11738/
Abstract
Background: This study evaluated the current pathways for dealing with patients admitted for surgery to address spinal metastases.
Methods: In this retrospective analysis (2016–2021), the following variables were studied admission, demographics, length of stay, critical care admission, hospital costs, primary cancer, and average survival.
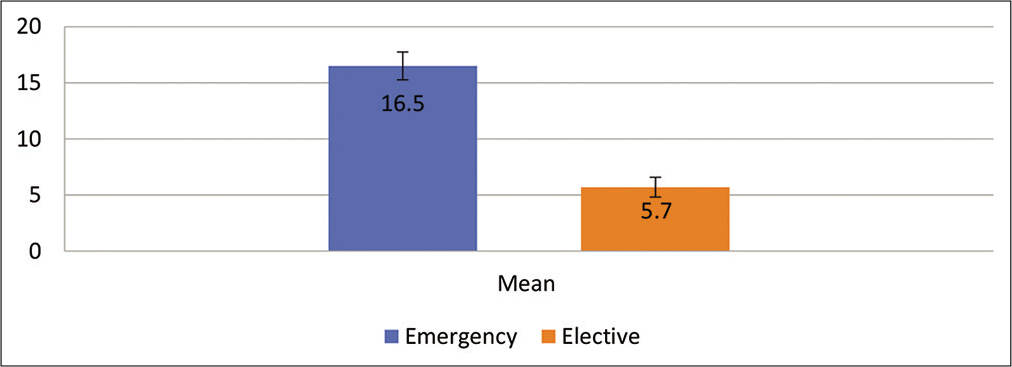
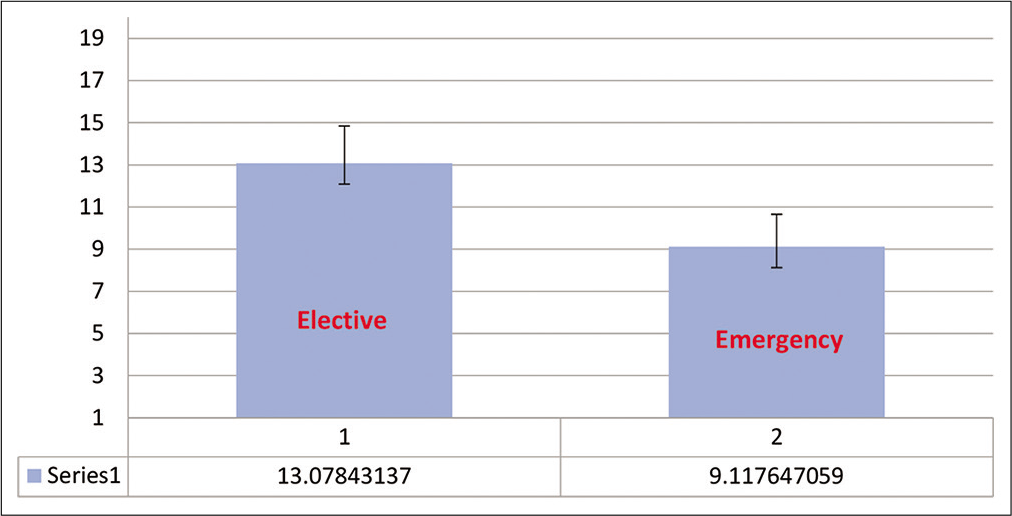
Results: There were 306 patients admitted from 2016 to 2021; 66 were planned admissions, 203 were emergency admissions, and 37 were day case admission. Patients averaged 65.4 years old. About 75% (203) were emergently admitted, while 25% (66) had planned elective admissions. Their respective lengths of stay were 16.5 versus 5.74 days. Interestingly, nearly half of the emergency admissions (46.3%) did not have surgery during that admission. The most common level for metastatic disease was the thoracic spine in both groups (53% in the elective vs. 62% emergency groups). The most common primary lesions included lung, breast, and prostate in both groups. The average survival in the emergency admission group was 9.1 months and the planned admission group was 13.07 months. Notably, the costs of emergent care were much higher than planned admissions.
Conclusion: The pathway for spinal metastases is unique in that though there is a pathway for late-stage disease, there is not one for early disease. As a result, the majority of patients admitted for surgery for spinal metastases come in as an emergency rather than as a planned admission. Yet, close to half do not end up having surgery during that emergency admission to the spinal center. The cost of emergency care is significantly higher versus planned elective care for spinal metastatic disease. A service transformation is suggested to combat these problems with a pathway for managing all spinal metastases, rather than just metastatic spinal cord compression.
Keywords: Metastatic spinal cord compression, Spinal metastasis, Surgical decompression
INTRODUCTION
Metastatic spinal cord compression (MSCC) is an oncological emergency and debilitating complication of cancer that occurs in 5–14% of patients.[
Patients with a life expectancy of more than 3–6 months may require surgical decompression ± stabilization of the spine. Most primary tumors (60–70%) arise from the lung, breast, or prostate. Interestingly, in 20–35% of cases, MSCC is the first presentation of systematic cancer.[
Although there is a unified pathway for managing end-stage disease (MSCC) disease, no such pathways exist for treating early-stage disease. Therefore, most patients with spinal metastases requiring surgery present as an emergency. Here, we evaluated whether outcomes, length of stay (LOS), costs, etc., would be improved/better if patients with spinal metastases requiring surgery could be identified earlier and undergo elective admissions/treatment.
MATERIALS AND METHODS
Data were retrospectively collected for metastatic spinal disease from 2016 to 2021 using CODE for bony metastases ICD10 C795. Patients were admitted to Spinal Surgery/ Neurosurgery Care.
The day case admissions were discarded as they were mainly for diagnosis.
RESULTS
Patient population
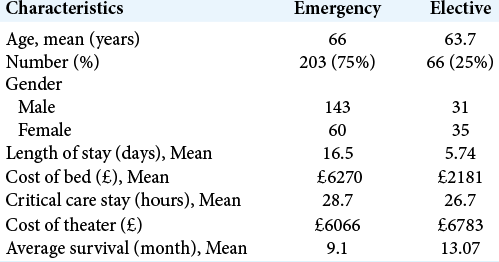
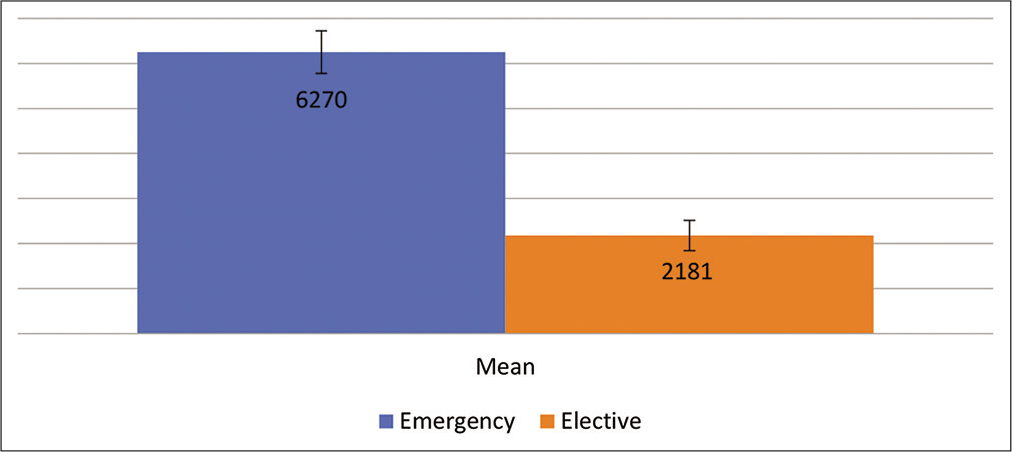
Patients were divided into two groups according to admission types: there were 66 (25%) elective admissions, while 203 (75%) were emergently admitted for considering surgery for spinal metastases. The mean age was similar in both groups; 63.74 years for elective versus 66 years for the emergency group [
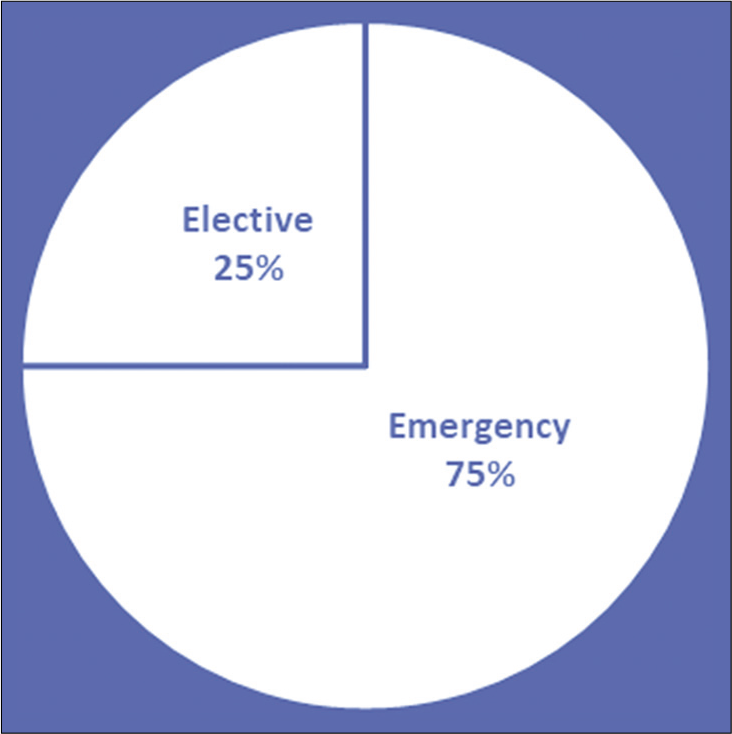
Source of elective versus emergent hospital admissions
Most of the elective admissions came through the city’s cancer center or the spinal surgery center’s outpatient clinic. However, the emergency admissions were from several different routes but mostly from other hospitals. Average survival for patients in the elective group was 13.07 months while for the emergency group was 9.1 months.
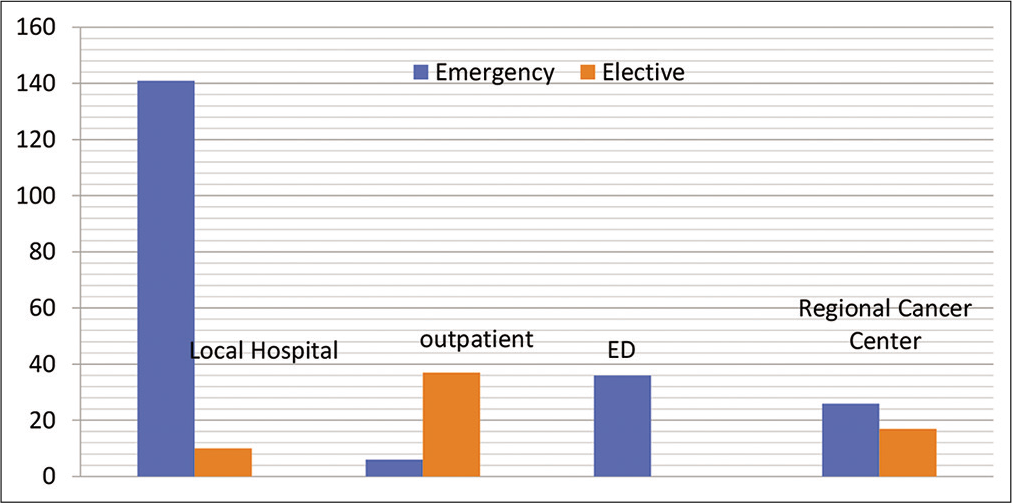
Relative costs of elective versus emergent hospitalization
The average cost of a bed in our neurosurgery/spinal department is approximately 380 pounds/day. The emergency group had a mean LOS of 16.5 days. Therefore, the emergency group had a mean bed cost of 6270 pounds while the elective group had 5.74 days mean stay and had a mean bed cost of 2181 pounds. The average duration of surgery was 364 min in the emergency group and 407 min in the elective group. The operative cost for 1-h in our operating room was £1000; therefore, the average cost for the emergency group for theater time was £6066 and for the elective group was £6783.
Statistical analysis
Data analysis was done using SPSS software 28 using descriptive statistics.
DISCUSSION
In this system review, we are evaluating the outcome and efficiency of the current pathway for managing spinal metastases which require surgery. The most common primary tumor sites were lung, breast, and prostate compromising about 54.2% and the thoracic spine was a common site for metastasis comprising about 60%. About 75% of our patients were admitted as an emergency and only a quarter had a planned elective admission [
This suggests poor utilization of beds in a tertiary center. Elective patients were mostly admitted through referral from the regional cancer center or the spinal center’s outpatient clinic, while emergency patients were admitted through a wide variety of health-care settings, but mostly from other hospitals [
Greater utilization/costs/LOS for emergencies
Greater LOS increased the average cost of emergency admission in terms of bed utilization to £6270 versus the mean elective cost of £2181 [
Similar time spent in theater and in ICU reflected similar complexity of cases in both the emergency and planned groups. The most common routes of admission in the elective group were from the outpatient clinic in the spine center and through the regional cancer center and for the emergency group, it was through the emergency departments in the local hospitals as well as the spine center. This suggests that earlier recognition of symptomatic spinal metastases can lead to a planned admission and late recognition leads to an emergency admission.
The data suggest that a planned admission for surgical management of spinal metastases is much better in resource utilization than an emergency admission despite the two groups undergoing a similar complexity of the surgery. Because of these findings, we propose a service transformation in which all spinal metastases, not just MSCC be referred through a unified portal, like what happens for brain metastases. This should enable earlier referrals for surgery in appropriate patients, enabling a planned admission.
The average survival in the planned elective group was 13.07 months and, in the emergency, group was 9.1 months [
CONCLUSION
The cost of caring for patients with spinal metastatic disease who come in as an emergency is much higher than for those who are admitted as an elective. Less than half of these patients have spinal surgery during that index emergency admission. Based on these findings, we propose a service transformation and a unified pathway for managing all spinal metastases rather than just one for managing MSCC.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Husband DJ. Malignant spinal cord compression: Prospective study of delays inreferral and treatment. BMJ. 1998. 317: 18-21
2. Lee CH, Kwon JW, Lee J, Hyun SJ, Kim KJ, Jahng TA. Direct decompressive surgery followed by radiotherapy versus radiotherapy alone for metastatic epidural spinal cord compression: A meta-analysis. Spine (Phila Pa 1976). 2014. 39: E587-92
3. Nemelc RM, Stadhouder A, van Royen BJ, Jiya TU. The outcome and survival of palliative surgery in thoracolumbar spinal metastases: Contemporary retrospective cohort study. Eur Spine J. 2014. 23: 2272-8
4. Schiff D, O’Neill BP, Suman VJ. Spinal epidural metastasis as the initial manifestation of malignancy: Clinical features and diagnostic approach. Neurology. 1997. 49: 452-6
5. Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases: Indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996. 199: 241-7