- Department of Neurosurgery, University of Buenos Aires, Buenos Aires,
- Neurointervention Section, Hospital El Cruce, Florencio Varela,
- Neurointervention Section, Sanatorio Anchorena, San Martín.
Correspondence Address:
Javier Goland
Department of Neurosurgery, University of Buenos Aires, Buenos Aires,
DOI:10.25259/SNI_569_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Javier Goland1,2,3, Gustavo Doroszuk2,3, Paula Ypa1,3, Paula Leyes2, Silvia Garbugino1. Outpatient treatment of cerebral aneurysms: A case series. 18-Nov-2020;11:400
How to cite this URL: Javier Goland1,2,3, Gustavo Doroszuk2,3, Paula Ypa1,3, Paula Leyes2, Silvia Garbugino1. Outpatient treatment of cerebral aneurysms: A case series. 18-Nov-2020;11:400. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10403
Abstract
Background: Major advances in the endovascular treatment of cerebral aneurysms have reduced the incidence of intra- and postprocedural complications. The length of stay after treatment for incidental aneurysms remains between early next-day discharge and 2 days. We hypothesized that discharging patients the same day would not be associated with any increase in the rate of postdischarge adverse events.
Methods: We retrospectively reviewed the charts of patients who underwent an elective coiling procedure between 2015 and 2020 at three centers and were discharged from hospital on the same day as the procedure. Patients were clinically evaluated 6 h, 1 week, and 6 months after the procedure, with repeat cerebral angiography performed 1 year after the procedure.
Results: Eleven eligible patients underwent outpatient treatment of 12 aneurysms treated through the wrist. No complications were identified within 1 week of the procedure. Clinical evaluation 6 months after treatment also failed to reveal any complication associated with the procedure. Only one of the seven patients who underwent 1 year angiography required retreatment.
Conclusion: It is possible to safely perform coiled embolization of cerebral aneurysms in select outpatients with unruptured cerebral aneurysms.
Keywords: Aneurysm, Distal radial approach, Outpatient treatment, Transradial approach, Ulnar approach
INTRODUCTION
Endovascular treatment of cerebral aneurysms has been shown to be both effective and associated with less morbidity than surgical treatment.[
In some studies, the ulnar artery has been used for percutaneous coronary interventions. It has even been shown that, when faced with a failed radial puncture, employing the ulnar artery in the same forearm is safe and with lower complications.[
Many of the complications associated with the femoral approach during percutaneous cardiac interventions can be avoided with any of wrist approaches, as has been shown in multiple comparative studies assessing both complications and patient’s quality of life.[
The endovascular treatment of nonruptured cerebral aneurysms with coils has a very low rate of complications, and most of them occur either during the procedure or within 6 h of its completion. There are no significant differences in the incidence of complications at 30 days between those patients discharged at 48 h and those who remain hospitalized longer.[
Performing the intervention through wrist artery access in select patients, we sought to determine whether we could shorten the postoperative observation time after endovascular aneurysms interventions to 6 h postprocedure.
MATERIALS AND METHODS
Informed consent was obtained from each patient before enrolling them in the study. All procedures were performed at one of three hospitals, all in Argentina: Hospital El Cruce, Hospital de Clínicas UBA, and Sanatorio Anchorena San Martín. Patient information was extracted from each hospital’s medical records database.
We enrolled in analysis all patients treated for cerebral aneurysms over the past 5 years at any of the three above-noted centers. To be eligible for inclusion, patients had to have had the intervention performed through the wrist as the first option for endovascular treatment and had to have been discharged from the hospital on the same day as their procedure.
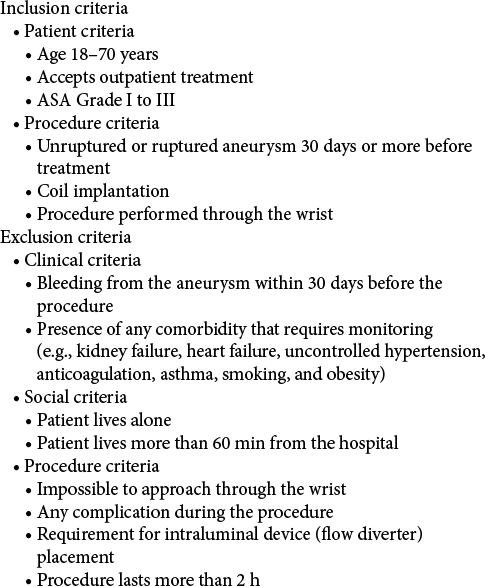
To determine which patients were eligible for discharge on the same day as treatment, we used a table of inclusion and exclusion criteria which had been used in a prospective multicenter study conducted in France for ambulatory coronary angioplasty, published in 2013.[
All patients in this series were admitted to the hospital on the morning of their procedure. The procedures were performed under general anesthesia. The technique we used, described in previous publications, consisted of puncturing the radial artery between 2 and 4 cm proximal to the wrist, or in the anatomical snuffbox for the distal radial approach. Ulnar puncture was performed between 2 and 4 cm proximal to the wrist when the previously mentioned approaches were considered impossible.[
At the end of each procedure, the patient was transferred to the inpatient day unit and allowed to resume ambulation after 2 h of bed rest. Then, 6 h after the procedure, a neurological examination and EKG were performed by an internist. Patients were cleared for discharge if they had no puncture site complications, neurological deficits, or electrocardiographic changes during the observation period. Patients were instructed to contact the surgical team in case of any complications overnight using a contact telephone number. One week after the procedure, the patients underwent neurological and puncture site evaluations. They then were followed up at 6 months clinically and at 1 year after the procedure with cerebral angiography, after which studies were repeated every 3 years.
RESULTS
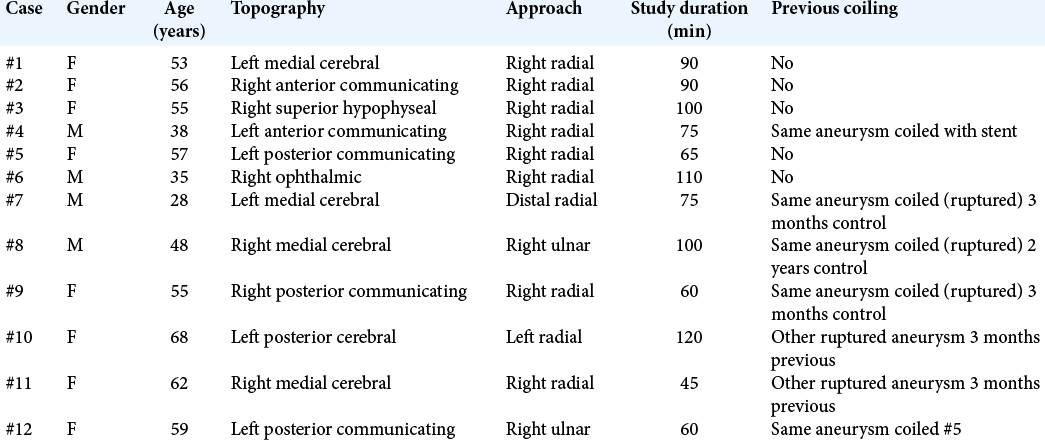
Between June 1, 2015, and March 31, 2020, radial, distal radial, or ulnar access were used to treat 212 aneurysms at our institutions. Among these cases, 12 aneurysms in 11 patients were selected for outpatient treatment [
The average patient age was 51 years. Four aneurysms had been coiled previously and one had been treated with a stent plus coils. One of the recoiled aneurysms (case #12) represents retreatment of a previously treated aneurysm of this series (case #5) which was slated for recanalization due to coil compaction detected during 1-year follow-up angiography. Two patients in the series had had another aneurysm coiled previously. Five aneurysms in the series were incidental with no other aneurysm treated.
All patients were treated as scheduled, remained under observation for 6 h, and were discharged on the same day as the procedure. The average duration of the procedure was 82 min. Seven of the 12 embolized aneurysms were assessed by follow-up angiography through wrist access 1 year after treatment. The remaining five have not yet reached their 1-year follow-up assessment. In terms of aneurysm location, four were in the medial cerebral artery, three the posterior communicating segment, two the anterior communicating artery, two the ophthalmic segment, and one the posterior cerebral artery. The distribution of approaches was: eight right radial, one distal right radial, one left radial, and two ulnar.
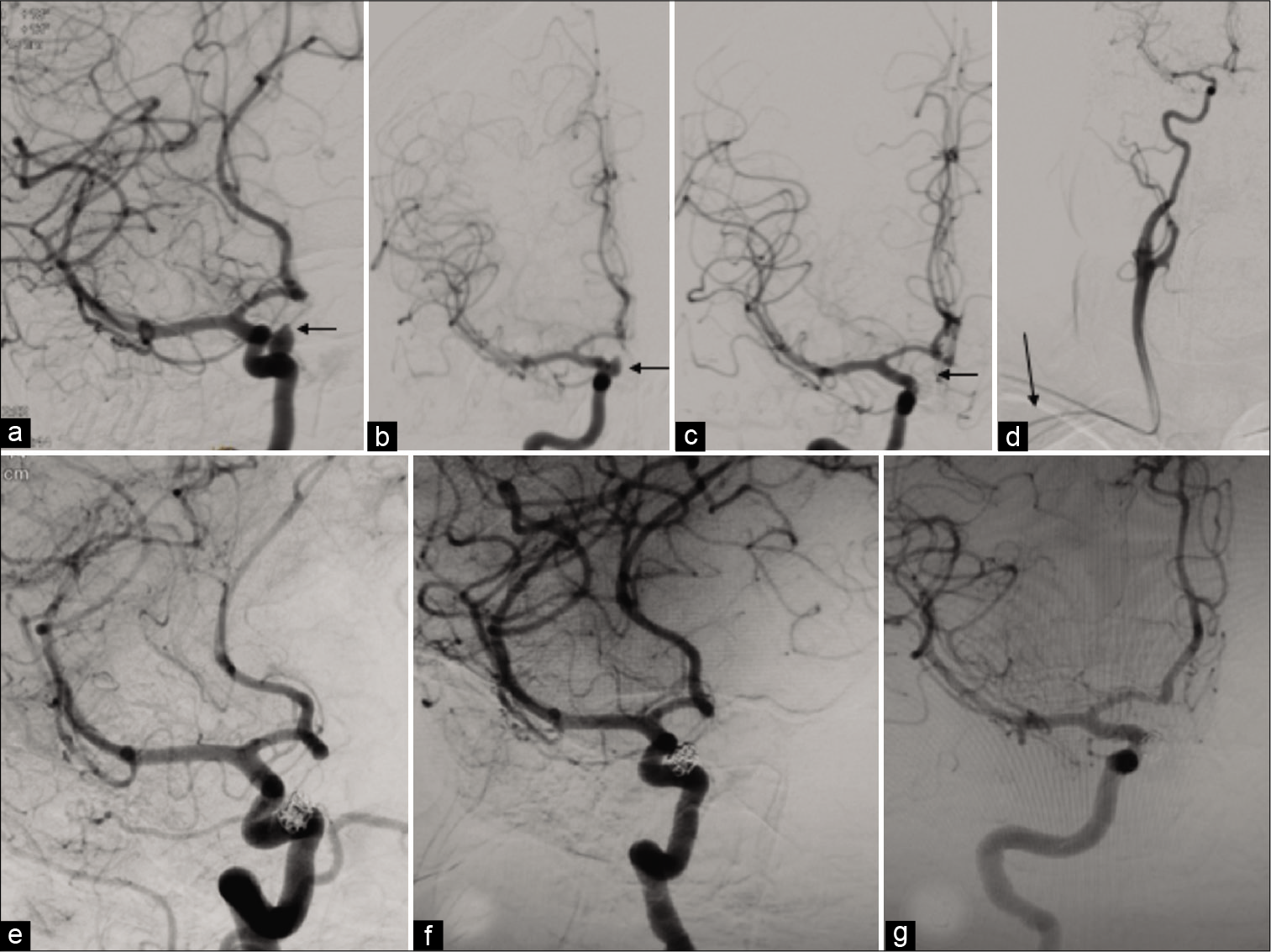
None of the patients experienced periprocedural complications or required readmission once discharged. Clinical follow-up 6 months postprocedure again revealed no complications associated with treatment. Six of the seven 1-year angiographies were considered satisfactory and not warranting retreatment [
Figure 1:
Case #3 (a) Right internal carotid angiogram, left oblique view. Incidental right superior hypophyseal aneurysm (arrow). (b) Anteroposterior view shows the same aneurysm. (c) Postembolization evaluation of the right internal carotid angiogram in an anteroposterior view shows the aneurysm totally occluded. (d) Final follow-up angiogram, in which the panoramic anteroposterior view shows the aneurysm totally occluded. The arrow indicates the approach. (e) One-year angiogram, left oblique view, reveals a totally occluded aneurysm. (f) Four-year follow-up left oblique view shows occlusion of the aneurysm. (g) Right oblique view in the same follow-up angiogram.
Case #5 presented with coil compaction, which was retreated on an outpatient basis as Case #12.
DISCUSSION
At present, outpatient surgery is elective for many procedures, reducing risks associated with hospitalization. Outpatient treatments are associated with greater comfort for patients, decreased morbidity, lower treatment costs, and faster reintegration of the patient into their daily life. To perform a procedure on an outpatient basis, however, it is necessary to evaluate both patient-related and procedure-related factors.[
With regard to the embolization of unruptured aneurysms, the most serious complications associated with treatment occur during the intervention and consist of rupture and thromboemboli. If such complications occur, it is unreasonable to consider a purely outpatient procedure. However, the immediacy of these events makes them easy to diagnose and, thereby, avoids early discharge of these patients.
In one prospective study, assessing unruptured aneurysms treated by the endovascular route (ATENA), the incidence of thromboembolic complications was 7.1%, including an aneurysm rupture rate of 2.6% and complications associated with implanted devices observed in 2.9%. A total of 48 thromboembolic complications occurred during or immediately after embolization. Only two events occurred late and they were between 7 and 11 days postprocedure. The mortality rate over the 1st month was 1.4%, while the morbidity rate was 1.7%.[
In a retrospective study that evaluated 311 unruptured aneurysms treated through the endovascular route to identify perioperative complications and, thereby, determine how necessary the patient’s stay in intensive care was, the complication rate was 6.4%. The authors concluded that, in 99.4% of cases, nonimmediate complications could be prevented by avoiding the femoral approach and avoiding the use of stents for aneurysms larger than 20 mm.[
In another study that analyzed perioperative complications that did not occur during the procedure, such as aneurysmal rupture and thromboembolism, 678 procedures were assessed for unruptured aneurysms in patients who had received double antiplatelet therapy 5 days earlier. Complications occurred in 36 procedures (5.31%). Of these, nine were hemorrhagic or thromboembolic events that occurred during the procedure, while 27 events (4%) were postintervention. Twenty of these 27 complications were diagnosed during the first 4 h posttreatment. The authors of this large single-center case series concluded that serious complications requiring urgent treatment are rare after the first 4 h postelective endovascular treatment of brain aneurysms.[
When the investigators compared complication rates at 30 days between patients discharged at 24 h and those discharged later in a study of 97 patients, they failed to identify any significant differences.[
Coil treatment of unruptured brain aneurysms approached through the wrist allows for the rapid ambulation of patients and reduces the rate of significant puncture-site hemorrhage. This is the reason we consider the approach as an important factor to take into account when deciding to treat endovascular aneurysms on an outpatient basis. The approach has already been shown to be effective and safe and is the first-line approach in our centers.[
To choose the right patient, each patient’s level of risk must be evaluated using different scales. One important measure of risk is anesthesia risk, which is determined using a scale established by the American Association of Anesthesiologists (ASA). Using this scale, a Grade III score is generally considered the upper limit beyond which outpatient procedures should be avoided. Other factors that must be evaluated include comorbid illnesses, some of which could be a contraindication for procedures of this type.[
To date, reports of short stays after embolization of unruptured brain aneurysms have generally been between next day and 2.4 days of hospitalization.[
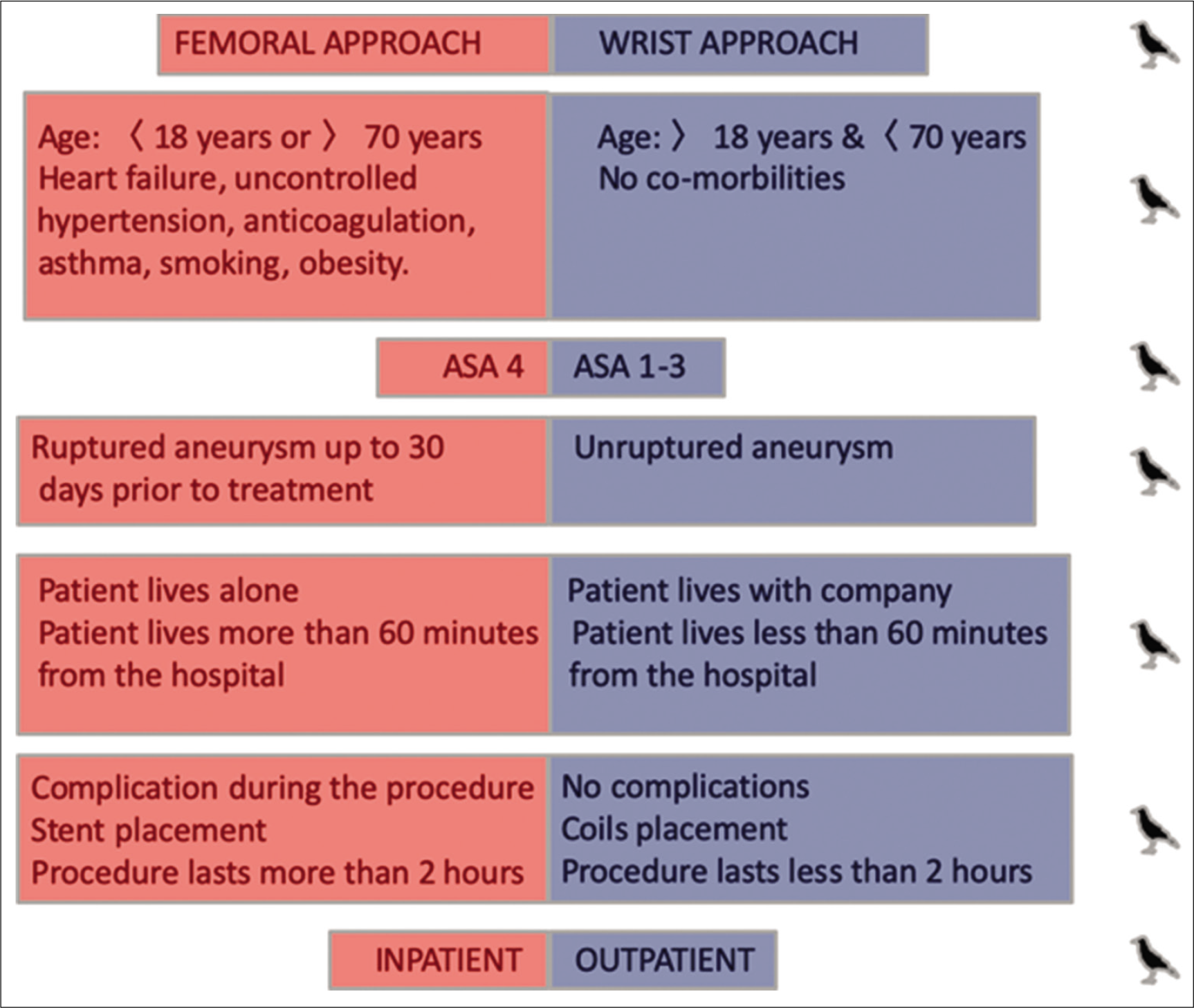
In this way, eliminating the risk of retroperitoneal hematoma and late complications due to stent thrombosis, we strictly choose patients whom we consider eligible for outpatient treatment. Of the 212 embolization procedures performed through the wrist at our three centers over the observation period of the current study, only 12 were deemed of low enough risk for the procedure to be performed on an outpatient basis. None of these 12 selected patients suffered complications or required readmission. We believe that patient selection was a very important determinant of our treatment success. In [
CONCLUSION
This study describes our experiences with a small cohort of patients with brain aneurysms who were treated as outpatients. We are convinced that observation in the hospital for 24 hours may not be necessary for all patients, but also that determining which patients are eligible for this short stay is crucial.
The transition from femoral to wrist access has rendered outpatient percutaneous cardiovascular interventions much safer and more feasible, largely by avoiding the risks of groin hematomas and retroperitoneal hematomas. To date, however, no experiences of cerebral aneurysms treatment using this outpatient approach have been published. Our series, although small, shows that it is possible to safely perform this type of therapy on an outpatient basis under certain circumstances.
Limitations of the work include the retrospective nature of data collection and small case sample. This prevents any evaluation of the influence of different factors on the results. We believe that our results provide sufficient cause to proceed with prospective studies to evaluate the safety of same-day discharge following endovascular interventions for certain unruptured aneurysms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agostoni P, Biondi-Zoccai GG, De Benedictis ML, Rigattieri S, Turri M, Anselmi M. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004. 44: 349-56
2. Agostoni P, Zuffi A, Faurie B, Tosi P, Samim M, Belkacemi A. Same wrist intervention via the cubital (ulnar) artery in case of radial puncture failure for percutaneous cardiac catheterization or intervention: The multicenter SWITCH registry. Int J Cardiol. 2013. 169: 52-6
3. Arias E, Patel B, Cross DT, Moran C, Dacey R, Zipfel G. Timing and nature of in-house postoperative events following uncomplicated elective endovascular aneurysm treatment. J Neurosurg. 2014. 121: 1063-70
4. Connolly ES, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American heart association/ American stroke association. Stroke. 2012. 43: 1711-37
5. Cooper CJ, El-Shiekh RA, Cohen DJ, Blaesing L, Burket MW, Basu A. Effect of transradial access on quality of life and cost of cardiac catheterization: A randomized comparison. Am Heart J. 1999. 138: 430-6
6. Cuisinier A, Albaladejo P. Management of comorbidity and preoperative treatment in ambulatory surgery?. Presse Med. 2014. 43: 283-90
7. Eichhöfer J, Horlick E, Ivanov J, Seidelin PH, Ross JR, Ing D. Decreased complication rates using the transradial compared to the transfemoral approach in percutaneous coronary intervention in the era of routine stenting and glycoprotein platelet IIb/IIIa inhibitor use: A large single-center experience. Am Heart J. 2008. 156: 864-70
8. Goland J, Domitrovic L, Doroszuk G, Garbugino S, Ypa P. Distal radial approach for neurointerventional diagnosis and therapy. Surg Neurol Int. 2019. 10: 211
9. Goland J, Doroszuk G. Transradial approach for endovascular diagnosis and treatment of ruptured cerebral aneurysms: A descriptive study. Surg Neurol Int. 2019. 10: 87
10. Goland J, Doroszuk GF, Garbugino SL, Ypa MP. Transradial approach to treating endovascular cerebral aneurysms: Case series and technical note. Surg Neurol Int. 2017. 8: 73
11. Ihn YK, Shin SH, Baik SK, Choi IS. Complications of endovascular treatment for intracranial aneurysms: Management and prevention. Interv Neuroradiol. 2018. 24: 237-45
12. Jeong YG, Kim EH, Hwang SM, Lee GY, Kim JW, Choi YJ. Outpatient (Same-day care) neuroangiography and neurointervention. Neurointervention. 2012. 7: 17-22
13. Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): A randomised, parallel group, multicentre trial. Lancet. 2011. 377: 1409-20
14. Kameda-Smith MM, Klurfan P, Van Adel BA, Larrazabal R, Farrokhyar F, Bennardo M. Timing of complications during and after elective endovascular intracranial aneurysm coiling. J Neurointerv Surg. 2018. 10: 374-9
15. Le Corvoisier P, Gellen B, Lesault PF, Cohen R, Champagne S, Duval AM. Ambulatory transradial percutaneous coronary intervention: A safe, effective, and cost-saving strategy. Catheter Cardiovasc Interv. 2013. 81: 15-23
16. Pierot L, Spelle L, Vitry F, ATENA Investigators. Immediate clinical outcome of patients harboring unruptured intracranial aneurysms treated by endovascular approach: Results of the ATENA study. Stroke. 2008. 39: 2497-504
17. Qadir N, Smith I. Day surgery: How far can we go and are there still any limits?. Curr Opin Anaesthesiol. 2007. 20: 503-7
18. Roghani-Dehkordi F, Mansouri R, Khosravi A, Mahaki B, Akbarzadeh M, Kermani-Alghoraishi M. Transulnar versus transradial approach for coronary angiography and angioplasty: Considering their complications. ARYA Atheroscler. 2018. 14: 128-31
19. Stetler WR, Griauzde J, Saadeh Y, Wilson TJ, Al-Holou WN, Chaudhary N. Is intensive care monitoring necessary after coil embolization of unruptured intracranial aneurysms?. J NeuroIntervent Surg. 2017. 9: 756-60
20. Terashima M, Meguro T, Takeda H, Endoh N, Ito Y, Mitsuoka M. Percutaneous ulnar artery approach for coronary angiography: A preliminary report in nine patients. Catheter Cardiovasc Interv. 2001. 53: 410-4
21. Thompson BG, Brown RD, Amin-Hanjani S, Broderick JP, Cockroft KM, Connolly ES. Guidelines for the management of patients with unruptured intracranial aneurysms: A guideline for healthcare professionals from the American heart association/ American stroke association. Stroke. 2015. 46: 2368-400
22. Zakhari N, Lum C, Quateen A, Iancu D, Lesiuk H. Next day discharge after elective intracranial aneurysm coiling: Is it safe?. J Neurointerv Surg. 2016. 8: 983-6
23. Zalocar LA, Doroszuk G, Goland J. Transradial approach and its variations for neurointerventional procedures: Literature review. Surg Neurol Int. 2020. 11: 248