- Department of Neurosurgery, Kanazawa University, Kanazawa, Ishikawa Prefecture, Japan.
- Department of Endocrinology and Metabolism, Kanazawa University, Kanazawa, Ishikawa Prefecture, Japan.
- Department of Neurosurgery, Fukui Prefectural Hospital, Fukui, Japan.
- Department of Neurosurgery, Kanazawa Medical University, Kahoku Gun, Ishikawa Prefecture, Japan.
- Department of Neurosurgery, Ishikawa Prefectural Central Hospital, Kanazawa, Ishikawa Prefecture, Japan.
Correspondence Address:
Kouichi Misaki, Department of Neurosurgery, Kanazawa University, Kanazawa, Ishikawa Prefecture, Japan.
DOI:10.25259/SNI_548_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nozomu Oikawa1, Kouichi Misaki1, Daisuke Aono2, Iku Nambu3, Yasuhiko Hayashi4, Naoyuki Uchiyama5, Mitsutoshi Nakada1. Panhypopituitarism caused by an unruptured giant cavernous internal carotid artery aneurysm compressing the pituitary gland treated with a flow-diverting stent: A case report. 26-Aug-2022;13:378
How to cite this URL: Nozomu Oikawa1, Kouichi Misaki1, Daisuke Aono2, Iku Nambu3, Yasuhiko Hayashi4, Naoyuki Uchiyama5, Mitsutoshi Nakada1. Panhypopituitarism caused by an unruptured giant cavernous internal carotid artery aneurysm compressing the pituitary gland treated with a flow-diverting stent: A case report. 26-Aug-2022;13:378. Available from: https://surgicalneurologyint.com/surgicalint-articles/11833/
Abstract
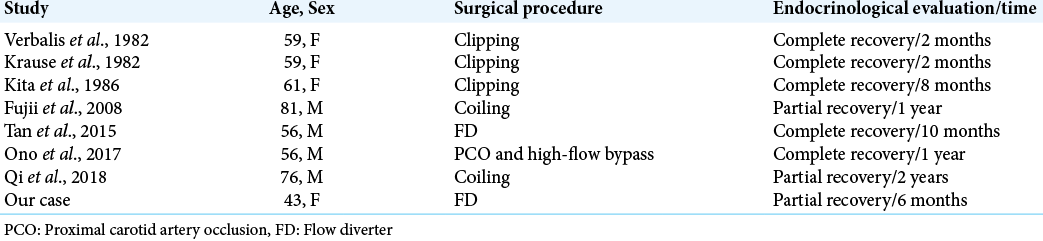
Background: Internal carotid artery (ICA) aneurysms extending into the intrasellar region that mimics pituitary tumors and leads to pituitary dysfunction are relatively rare. The treatment for aneurysms includes surgery and endovascular procedures. However, functional recovery of the pituitary gland is difficult.
Case Description: We report a case of a 43-year-old woman who presented with severe headaches and generalized malaise. Magnetic resonance imaging (MRI) revealed a giant unruptured cavernous ICA aneurysm that pushed the pituitary stalk contralaterally. A baseline endocrinological examination suggested panhypopituitarism. Hypopituitarism was treated with hormone replacement therapy, which improved the patient’s symptoms of headaches and malaise after 4 days. The aneurysm was treated using a pipeline flow-diverting stent. Two years later, the aneurysm had reduced to half of its maximum diameter, and the pituitary stalk was visible on MRI. Hormone loading tests 1 week postoperatively showed almost no response. At postoperative 6 months, there was a trend toward improvement.
Conclusion: Flow-diverting stent deployment is useful for large or giant carotid artery aneurysms with pituitary gland compression.
Keywords: Cavernous internal carotid artery aneurysm, Flow-diverting stent, Panhypopituitarism
INTRODUCTION
It is relatively rare for internal carotid artery (ICA) aneurysms to extend into the sella and leads to pituitary dysfunction. However, it can occur with large or giant aneurysms. Mechanical compression and pulsation of aneurysms, and disruption of microvascular supply can cause hormone depletion.[
CASE DESCRIPTION
A 43-year-old woman presented with severe headaches and generalized malaise for 5 days. Endocrine investigation revealed hypopituitarism with markedly decreased levels of early morning cortisol, thyroid hormone with low thyroid-stimulating hormone, growth hormone, and insulin-like growth factor 1. Physical examination was unremarkable. There were no visual deficits on ophthalmological examination. MRI and magnetic resonance angiography showed a significant mass effect on the pituitary gland, with a giant right cavernous ICA thrombotic aneurysm measuring 26.4 mm at the largest diameter [
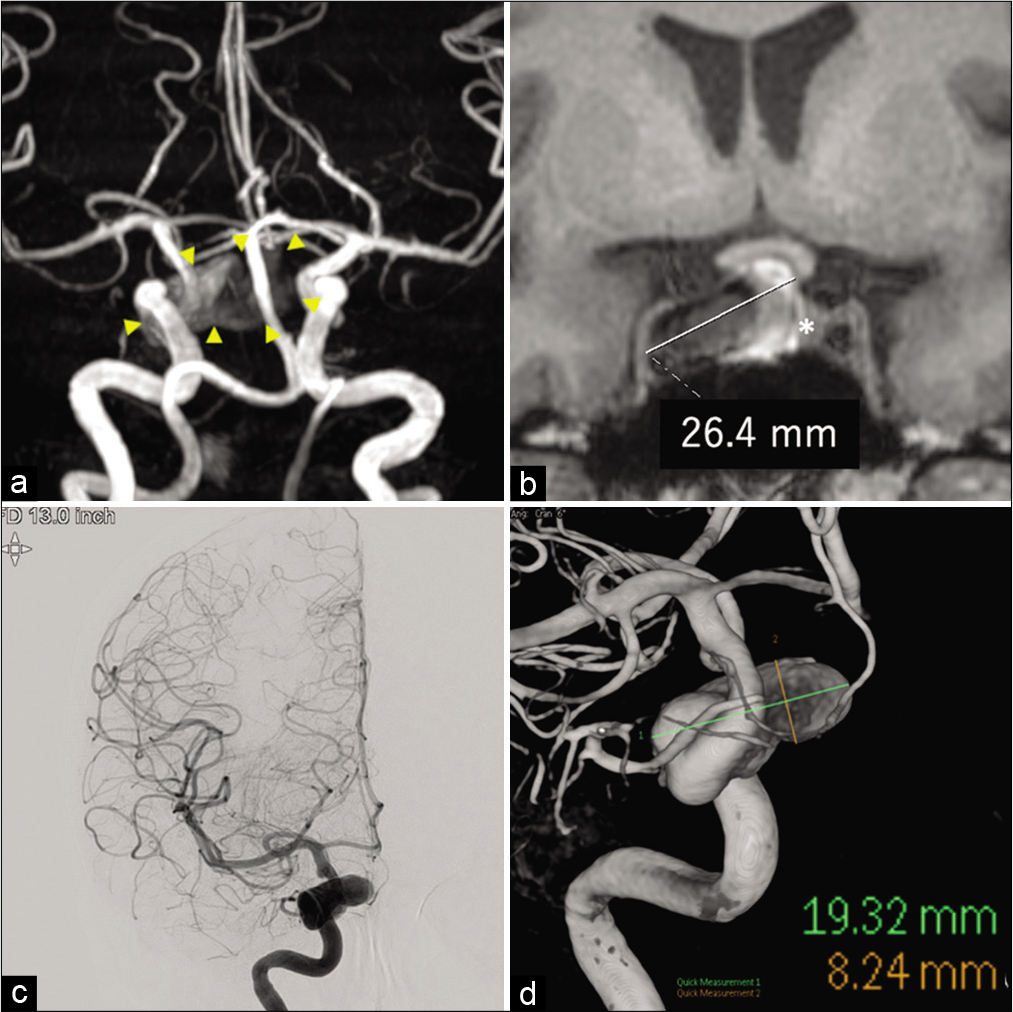
Figure 1:
(a) Magnetic resonance angiography showing a giant right cavernous internal carotid artery (ICA) aneurysm. The aneurysm is surrounded by arrowheads. (b) T1-weighted coronal magnetic resonance imaging showing a thrombotic aneurysm measuring 26.4 mm at the largest diameter, as indicated by white line. The asterisk refers to the pituitary gland that is ablated by an aneurysm. (c) Digital subtraction angiography shows the right cavernous ICA aneurysm. (d) 3D rotational angiography shows aneurysm excluded thrombosis measuring at 19.3 mm at largest diameter, as indicated by green line. The height of the aneurysm is 8.2 mm, indicated by the orange line.
Figure 2:
(a) The working angle of digital subtraction angiography (DSA) before flow diverter deployment is presented. (b) DSA immediately after deployment of the flow-diverting stent for the aneurysm showing an eclipse sign. (c) A flow-diverting stent was deployed and radiographs were taken. The flow diverter was confirmed to cover the neck of the aneurysm. Arrowheads indicate flow-diverting stents.
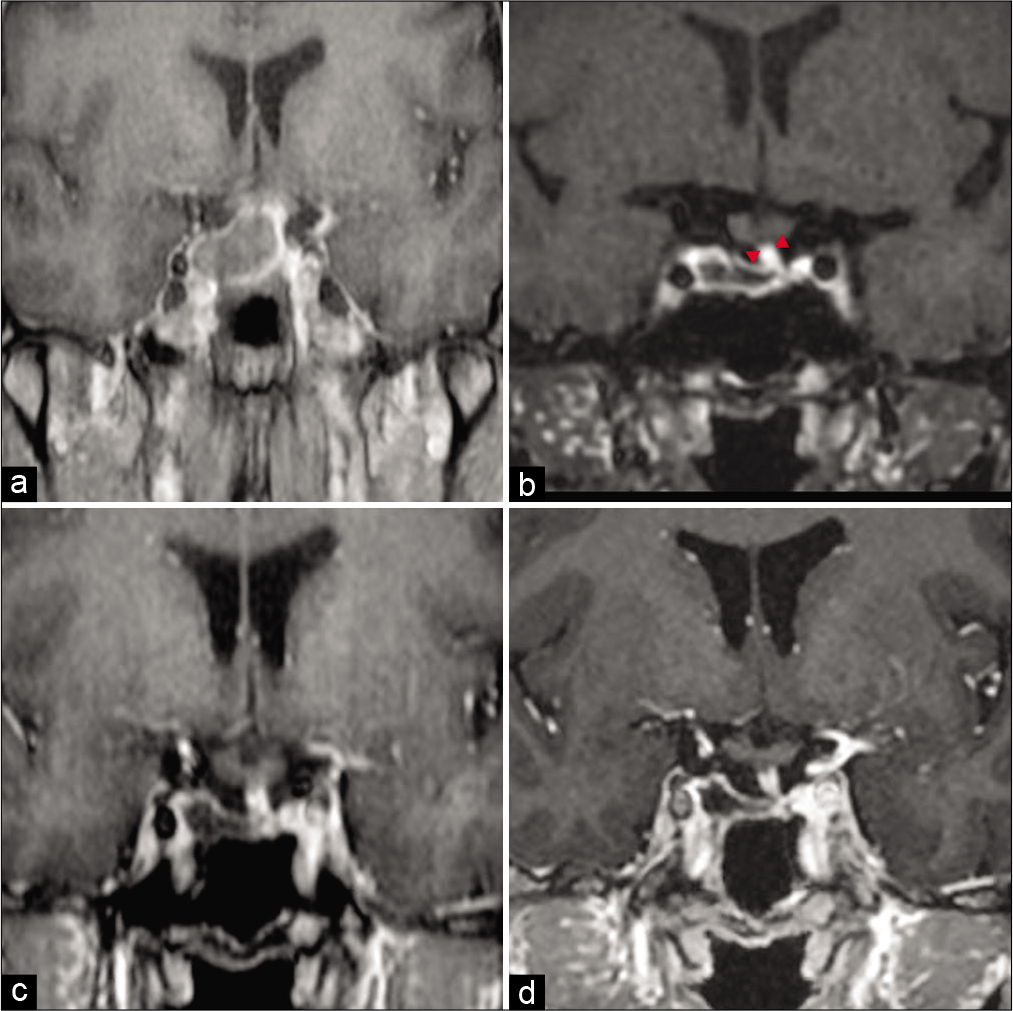
Figure 3:
(a) Contrast-enhanced T1-weighted imaging 1 week after endovascular surgery is presented. It shows a tendency toward thrombosis, but the pituitary gland is compressed and cannot be seen clearly. (b) Contrast-enhanced T1-VISTA imaging performed 9 months after the endovascular surgery. The aneurysm shrank significantly. The pituitary stalk, circled by arrowheads, can now be observed. (c) Contrast-enhanced T1-weighted image 16 months after endovascular surgery the aneurysm was further reduced compared to 9 months after endovascular surgery. (d) Contrast-enhanced T1-weighted image 24 months after endovascular surgery. The aneurysm was generally unchanged in size 16 months after endovascular surgery.
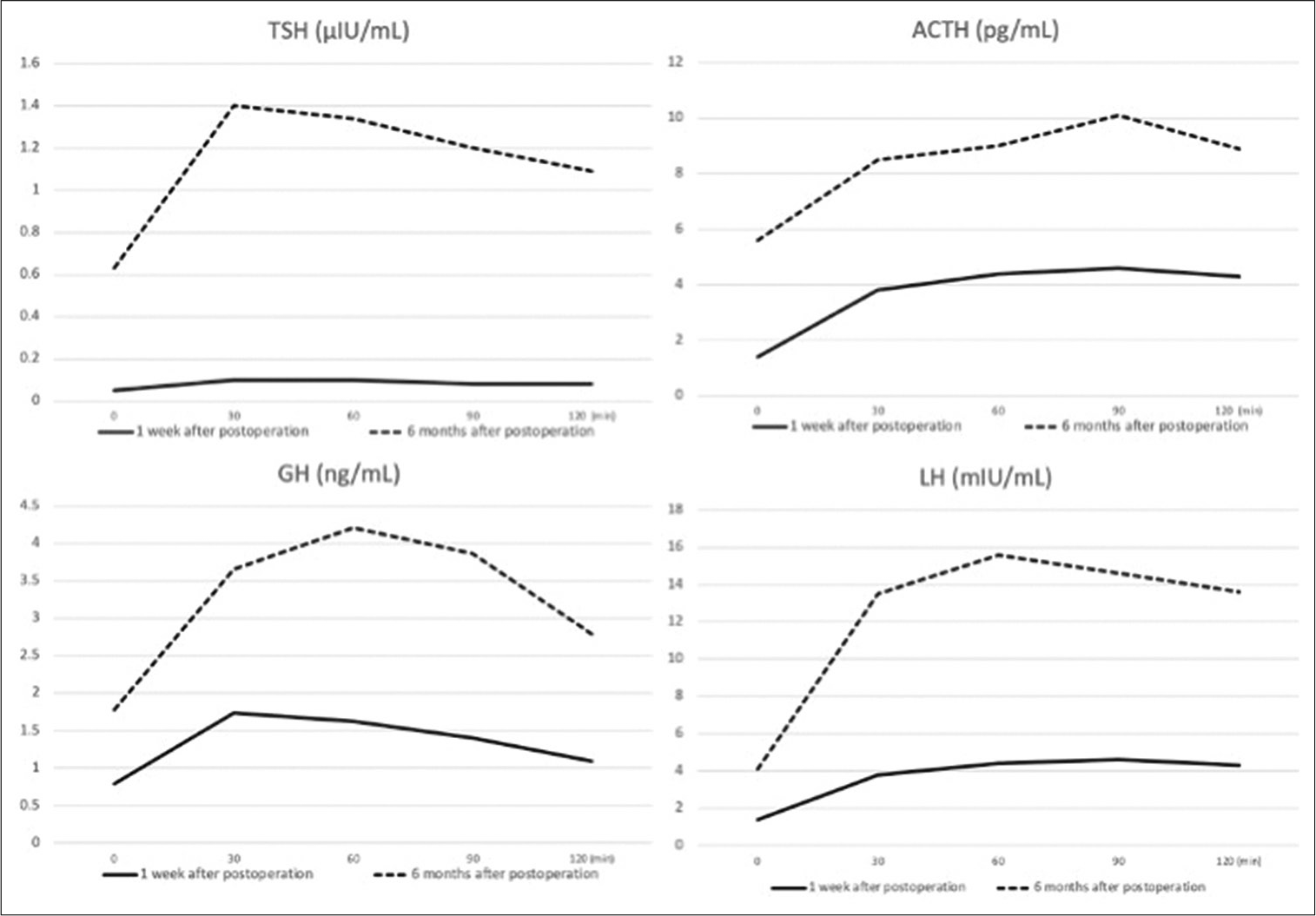
Figure 4:
Time series graphs of hormone load tests. The solid and dotted lines indicate the date 1 week and 6 months after the operation, respectively. In the thyrotropin-releasing hormone loading test, the normal maximum thyroid-stimulating hormone level was more than 6 μIU/mL, but the measured value did not reach the normal value at 1 week and 6 months after surgery. In the corticotropin-releasing hormone loading test, the normal apex value of adrenocorticotropic hormone is more than twice the preloading value at more than 30 pg/mL, but the measured value did not reach the normal value at 1 week and 6 months after surgery. In the growth hormone-releasing peptide-2 loading test, the normal maximum growth hormone level is more than 9 ng/mL, but the measured value did not reach the normal value at 1 week and 6 months after surgery. In the follicle-stimulating hormone loading test, the normal maximum luteinizing hormone level is more than 5 times the preloading value, but the measured value did not reach the normal value at 1 week and 6 months after surgery. However, there is an improvement in responsiveness in all loading tests at 6 months compared to 1 week postoperatively.
DISCUSSION
This is the first case to demonstrate that deployment of a flow-diverting stent for a cerebral aneurysm associated with hypopituitarism resulted in mass reduction on MRI and improved hormonal response over time. Pituitary dysfunction is estimated to have an annual incidence of 4.2 cases/100,000 and a prevalence of 45.5/100,000.[
CONCLUSION
We treated a panhypopituitarism-associated cerebral aneurysm with flow-diverting stent deployment. Postoperatively, the aneurysm was significantly reduced in size, and the response of pituitary function improved. Flow-diverting stent deployment may be an option for patients with large or giant ICA aneurysms which cause pituitary insufficiency.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ding D, Mehta GU, Liu KC. Pituitary insufficiency from large unruptured supraclinoid internal carotid artery aneurysm. Br J Neurosurg. 2014. 28: 290-2
2. Fujii M, Tone O, Tomita H, Tamaki M, Akimoto H, Shigeta K. Endosaccular embolization of an intrasellar aneurysm with hypopituitarism: Case report. No Shinkei Geka. 2008. 36: 329-37
3. Heshmati HM, Fatourechi V, Dagam SA, Piepgras DG. Hypopituitarism caused by intrasellar aneurysms. Mayo Clin Proc. 2001. 76: 789-93
4. Kita Y, Kawato M, Nakabayashi H, Takeda R, Usukura N, Hasatani K. A case of reversible hypopituitarism with hyperprolactinemia caused by a large suprasellar aneurysm. Nihon Naika Gakkai Zasshi. 1986. 75: 1756-63
5. Krauss HR, Slamovits TL, Sibony PA, Verbalis JG, Nelson PB. Carotid artery aneurysm simulating pituitary adenoma. J Clin Neuroophthalmol. 1982. 2: 169-74
6. Ono H, Inoue T, Tanishima T, Tamura A, Saito I, Saito N. High-flow bypass with radial artery graft followed by internal carotid artery ligation for large or giant aneurysms of cavernous or cervical portion: Clinical results and cognitive performance. Neurosurg Rev. 2018. 41: 655-65
7. Qi M, Ye M, Li M, Zhang P. Pituitary dysfunction from an unruptured ophthalmic internal carotid artery aneurysm with improved 2-year follow-up results: A case report. Open Med (Wars). 2018. 13: 137-41
8. Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E. Hypopituitarism. Lancet. 2007. 369: 1461-70
9. Tan LA, Sandler V, Todorova-Koteva K, Levine L, Lopes DK, Moftakhar R. Recovery of pituitary function following treatment of an unruptured giant cavernous carotid aneurysm using Surpass flow-diverting stents. J Neurointerv Surg. 2015. 7: e20
10. Tungaria A, Kumar V, Garg P, Jaiswal AK, Behari S. Giant, thrombosed, sellar-suprasellar internal carotid artery aneurysm with persistent, primitive trigeminal artery causing hypopituitarism. Acta Neurochir (Wien). 2011. 153: 1129-33
11. Verbalis JG, Nelson PB, Robinson AG. Reversible panhypopituitarism caused by a suprasellar aneurysm: The contribution of mass effect to pituitary dysfunction. Neurosurgery. 1982. 10: 604-11