- Department of Pediatrics, Saitama Medical Center, Kawagoe, Japan.
Correspondence Address:
Shinya Tomori, Department of Pediatrics, Saitama Medical Center, Kawagoe, Japan.
DOI:10.25259/SNI_994_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shinya Tomori, Seigo Korematsu, Shoyo Tanikawa, Yasuko Urushihara, Koichi Moriwaki. Paraspinal muscle abscesses in children – A case report and review of the literature. 06-Jan-2023;14:3
How to cite this URL: Shinya Tomori, Seigo Korematsu, Shoyo Tanikawa, Yasuko Urushihara, Koichi Moriwaki. Paraspinal muscle abscesses in children – A case report and review of the literature. 06-Jan-2023;14:3. Available from: https://surgicalneurologyint.com/surgicalint-articles/12097/
Abstract
Background: Few pediatric cases with myositis and abscesses of the paraspinal muscles have been previously reported.
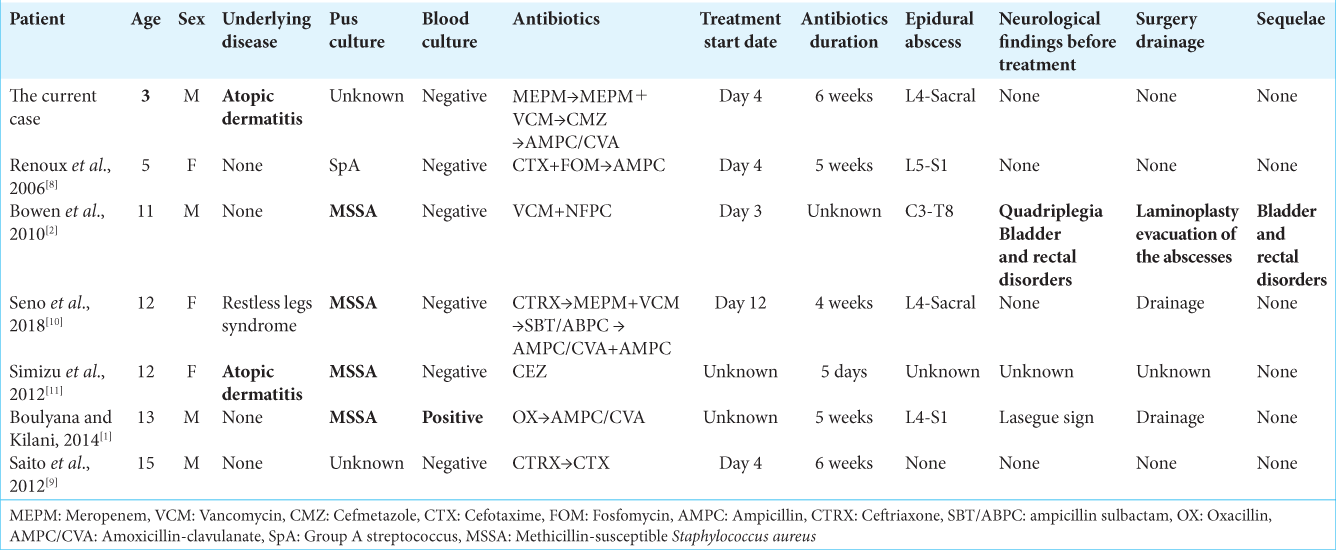
Case Description: We herein report on a 3-year-old patient who developed an epidural abscess in a paraspinal muscle abscess, after a complication of infectious impetigo due to atopic dermatitis. The child improved through the administration of an antibacterial drug. The median age of seven patients with a history of paraspinal muscle inflammation and muscle abscess was 12 years old (3–15-years-old), few of which had underlying diseases, with methicillin-sensitive Staphylococcus aureus being the main causative agent. Although the prognosis was well in many cases following the administration of antibacterial agents, there were also cases in which extensive lesions were found and neurological sequelae remained.
Conclusion: The current case was the youngest case ever reported of a paraspinal muscle abscess. Although pediatric cases are rare, in the episode of a fever of unknown origin and difficulty walking, paraspinal muscle abscesses should be cited as a differential diagnosis and appropriate early diagnostic imaging and treatment should be performed.
Keywords: Abscess, Epidural abscess, Low back pain, Paraspinal muscles
INTRODUCTION
Pyomyositis often develops in the tropics, with approximately 30% of such cases being children.[
CASE DESCRIPTION
A 3-year-old boy born to healthy Japanese parents. He has been suffered from atopic dermatitis and bronchial asthma. He had no history of repeated and severe infectious diseases. He had been suffering from infectious impetigo on both legs and his trunk since 1 month before admission. Five days before, infectious impetigo worsened in his right knee fossa and 3 days before, he complained of back pain in his right lower back and difficulty walking. Because he developed a fever of 38°C on the day of admission, he was referred by a local doctor and thus was admitted to our hospital.
His consciousness was clear at the time of admission. His body temperature was 37.8°C, but there was no respiratory distress or tachycardia. Impetigo was scattered throughout his right popliteal fossa, limbs, and trunk. Although the psoas sign was positive, there was no spinal strike pain. There were no abnormalities in other physical findings. The results of a clinical examination found 19,200/μL of leukocytes, of which 85.4% were neutrophils. Fibrinogen increased to 1,027 mg/ dL, D-dimer increased to 2.31 μg/dL, and C-reactive protein (CRP) increased to 16.48 mg/dL. Despite the increase of Immunoglobulin E (IgE) 595 IU/mL, the rest was normal with Immunoglobulin G (IgG) 834 mg/dL, Immunoglobulin A (IgA) 168 mg/dL, Immunoglobulin M (IgM) 67 mg/dL, CD4 32.1%, and CD8 36.8%. Because he had asthma, a computed tomography (CT) examination was performed without contrast, thus indicating no ascite retention and no high absorption areas in the organs.
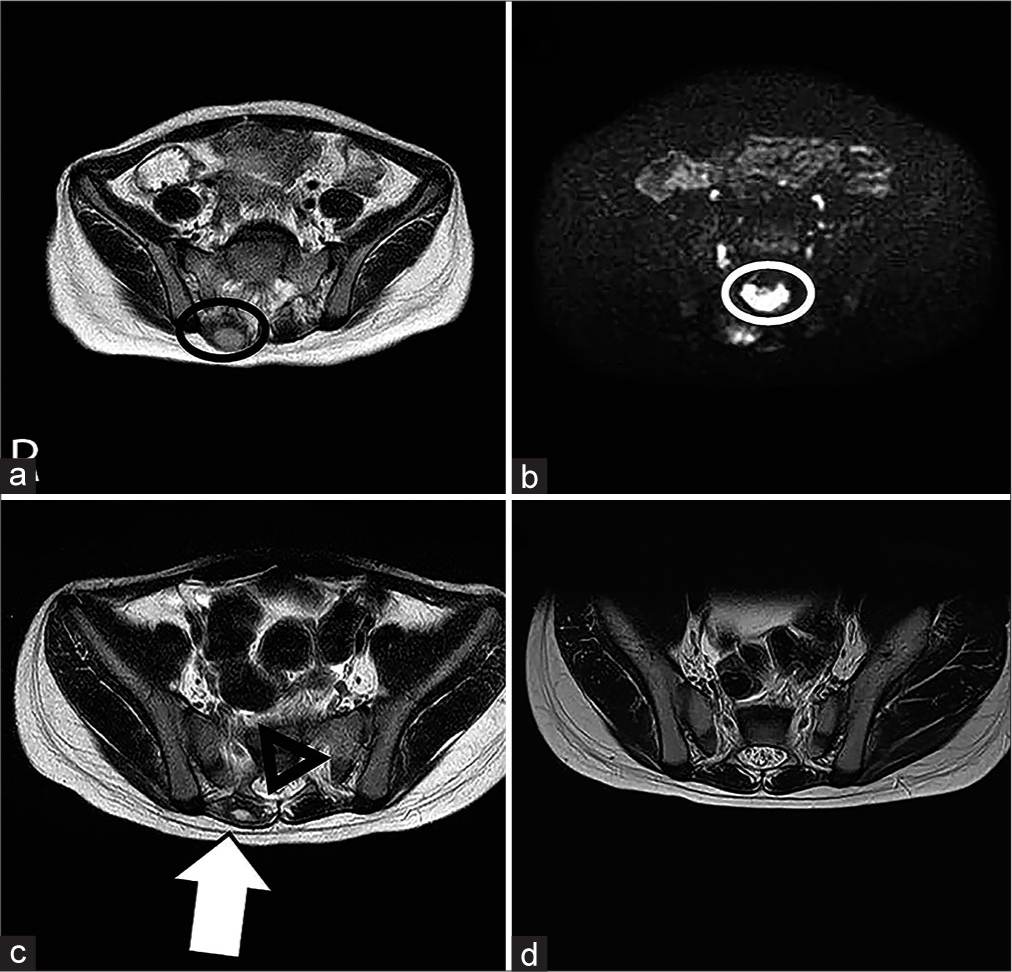
The administration of meropenem was initiated and he underwent a simple lumbar-pelvic magnetic resonance imaging (MRI) scan on the 6th day of illness. The T2-enhanced image indicated hyperintensity of marginalization at 2 cm in the right erector spinae muscle, while the diffusion-enhanced image indicated hyperintensity in the posterior to the spinal canal from L4 vertebral body to the sacral region [
Figure 1:
Lumbar to pelvic simple MRI images were taken of (a) and (b) on the 6th day of illness, (c) on the 13th day of illness, and (d) 1 month after discharge.(a) T2-emphasized image: A hyperintensity of marginalization is observed at 2 cm in the right erector spinae muscle (black circle). (b) Diffusion-weighted image: hyperintensity is observed in the posterior to the spinal canal from L4 vertebral body to the sacral region (white circle), (c) T2-enhanced image: paraspinal muscle abscess (white arrow) and epidural abscess (black triangle) tend to shrink, and (d) T2- emphasized image: it is confirmed that the image has completely disappeared.
Due to possible development from impetigo, he additionally received vancomycin, targeting methicillin-resistant Staphylococcus aureus (MRSA), on the 9th day of illness. His fever receded and his back pain improved the following day. Because the blood culture and the culture of the impetigo site were negative, it was considered that the possibility of MRSA was low, so his treatment was changed to cefazolin. He was discharged from the hospital on the 33rd hospital day, following the intravenous injection of antibacterial agents for a total of 4 weeks and a change to the oral administration of ampicillin and clavulanic acid. Subsequently, he progressed without any sequelae such as walking and neurological abnormal findings. A simple MRI of the lumbar spine to pelvic was taken on the 13th day of onset, confirming the reduction of the abscess [
DISCUSSION
This paper describes a paraspinal muscle abscess in an infant with an epidural abscess. While the causative bacteria were not identified, the illness improved with antibacterial agents.
Because the causative organisms of pyogenic myositis and muscle abscesses are S. aureus and Group A beta-streptococcus and beta-lactamase inhibitor combination penicillin and first- and second-generation cephems are generally the drugs of choice as empirical therapy.[
However, in this case, epidural or muscle abscess was also raised as a differential diagnosis due to unexplained fever and back pain, but it was difficult to differentiate it from other diseases until MRI imaging, and since the lesion and causative organism were unknown, meropenem, a broad-spectrum antibacterial agent, was used. Because of the possibility that the disease could have developed from impetigo, an additional dose of vancomycin targeting MRSA was administered. This case is also complicated by an epidural abscess. It is recommended that a broad-spectrum antimicrobial agent be the treatment of choice for epidural abscesses, and if MRSA is suspected, vancomycin may also need to be administered.[
The recommended treatment for muscle abscesses is antimicrobials alone for mild cases and incisional drainage in addition to antimicrobials for moderate cases. In addition to antimicrobial agents and incisional drainage, treatment for various complications is required for patients with severe cases.[
Zheng et al. reported that myositis and abscesses of the paraspinal muscles account for 4–6% of pyomyositis even in adults.[
The median age of these seven cases was 12 years old (range: 3–15-years-old), with this 3-year-old case being the youngest. Although there were few cases with underlying diseases unlike adults, there were two cases with atopic dermatitis, including the current case.[
There were cases in which surgical treatment and sequelae remained even if early treatment was possible.[
This review of the literatures has a limitation. The reason why there were 4 out of 7 Japanese cases may be due to the research being conducted in Japan. It is possible that research could not be conducted on domestic limited journals of other countries. On the other hand, it is possible that there are many cases of diagnosis due to the medical environment in Japan which allows MRI examinations to be performed quickly. Despite this limitations, this is the first report summarizing the clinical features of paraspinal muscle myositis and muscle abscesses in children.
CONCLUSION
In the seven cases of paraspinal muscle myositis and muscle abscess, while there were few underlying diseases and MSSA was high in pus cultures, it seemed to be difficult to detect the causative bacteria in blood cultures. Furthermore, the neurological prognosis of narrow epidural abscesses confined to the thoracolumbar spine was well, similar to reports in adults. The current case is the youngest of a paraspinal muscle abscess ever reported. While pediatric cases are rare, infants might not be able to complain of lower back pain. For this reason, muscle abscesses should be distinguished from medical history including trauma history, fever without fracture, and difficulty walking. Furthermore, paraspinal muscle abscesses are more likely to be associated with epidural abscesses and may have possible to lead neurological complications, so early diagnosis and treatment should be performed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Boulyana M, Kilani MS. Nontropical pyomyositis complicated with spinal epidural abscess in a previously healthy child. Surg Neurol Int. 2014. 16: 119-21
2. Bowen DK, Mitchell LA, Burnett MW, Rooks VJ, Martin JE. Spinal epidural abscess due to tropical pyomyositis in immunocompetent adolescents. J Neurosurg Pediatr. 2010. 6: 33-7
3. Chauhan S, Jain S, Varma S, Chauhan SS. Tropical pyomyositis (myositis tropicans): Current perspective. Postgrad Med J. 2004. 80: 267-70
4. Chiedozi LC. Pyomyositis. Review of 205 cases in 112 patients. Am J Surg. 1979. 137: 255-9
5. Miller NJ, Duncan RD, Huntley JS. The conservative management of primary pyomyositis abscess in children: Case series and review of the literature. Scott Med J. 2011. 56: 181
6. Mitsionis GI, Manoudis GN, Lykissas MG, Sionti I, Motsis E, Georgoulis AD. Pyomyositis in children: Early diagnosis and treatment. J Pediatr Surg. 2009. 44: 2173-8
7. Ravandi B, Cho C. Pediatric spinal epidural abscess: Recognition and management in the emergency department. Pediatr Emerg Med Pract. 2022. 19: 1-16
8. Renoux MC, Guyon G, Rodiere M. Paravertebral streptococcal myositis complicated by an epidural abscess in a 5-year-old girl. Arch Pediatr. 2006. 13: 273-5
9. Saito H, Suzuki R, Kusumoto K, Suzuki D, Takahashi R, Sogi C. A case of paraspinal muscle abscess. Bou sekichu kinniku nai nouyo no ichirei (in Japanese). J Sendai City Hosp. 2012. 32: 65-9
10. Seno S, Ono S, Kaji S. Paraspinal muscle abscess complicated with epidural abscess and intervertebral joint arthritis: A case report. J Pediatr Infect Dis Immunol. 2014. 30: 231-7
11. Simizu U, Oishi T, Suzuki D, Yamamoto K, Banno T. Pyomyositis in children: A report of two cases. Cent. Jpn J Orthop Traumat. 2012. 55: 1435-6
12. Zheng YC, Chen CC, Wei KC, Chen JF, Lee ST, Liao CC. Tropical pyomyositis of erector spinae complicated with spinal epidural abscess. Clin Neurol Neurosurg. 2015. 128: 84-9