- Department of Neurosurgery, Hospital Promater, Federal University of Rio Grande do Norte, Brazil.
- Department of Neurosurgery and Neurology, Hospital Onofre Lopes, Federal University of Rio Grande do Norte, Brazil.
- Department of Medicine, Medical School, Universidade Potiguar, Natal, Rio Grande do Norte, Brazil.
Correspondence Address:
André Corsino da Costa, Department of Neurosurgery, Hospital Promater, Natal, Rio Grande do Norte, Brazil.
DOI:10.25259/SNI_629_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: André Corsino da Costa1, Nilson Pinheiro Júnior2, Clecio Godeiro Junior2, Ana Clara Aragão Fernandes3, Cítara Trindade de Queiroz3, Anaís Concepcion Marinho Andrade de Moura3, Carlos Eduardo França de Aquino3, Marianne de Araújo Rego3. Parkinsonism secondary to ventriculoperitoneal shunt in a patient with hydrocephalus. 30-Aug-2021;12:432
How to cite this URL: André Corsino da Costa1, Nilson Pinheiro Júnior2, Clecio Godeiro Junior2, Ana Clara Aragão Fernandes3, Cítara Trindade de Queiroz3, Anaís Concepcion Marinho Andrade de Moura3, Carlos Eduardo França de Aquino3, Marianne de Araújo Rego3. Parkinsonism secondary to ventriculoperitoneal shunt in a patient with hydrocephalus. 30-Aug-2021;12:432. Available from: https://surgicalneurologyint.com/surgicalint-articles/11077/
Abstract
Background: Parkinsonism secondary to the treatment of obstructive hydrocephalus due to stenosis of the cerebral aqueduct, with implantation of a ventricular peritoneal (VP) shunt is a rare complication, still poorly described and disseminated in the literature.
Case Description: A 38-year-old male presented a history of moderate-intensity daily headache, which deteriorated 2 months before admission, with no changes in the neurological examination. Magnetic resonance imaging showed hypertensive hydrocephalus associated with cerebral aqueduct stenosis. A VP shunt was performed, an adjustable pressure valve was successfully inserted, and he was discharged asymptomatic. However, months later, he progressed with important symptoms of hypo- and hyper-drainage, which persisted after valve pressure adjustments and even its exchange, culminating into an endoscopic third ventriculostomy (ETV). But soon after, severe Parkinsonian syndrome appeared. Therapy with levodopa and bromocriptine was initiated, revealing a slow response initially but good evolution within 6 months. At present, he presents low-intensity residual tremor, which is well controlled with medications, and has regained independence for daily activities, with minimal motor limitation and no cognitive changes.
Conclusion: There is still no mechanism that explains the occurrence of Parkinsonian syndrome in these cases. It is suggested that the rostral portion of the midbrain was injured due to abrupt changes in the transtentorial gradient pressure after the ventricular shunt, along with various adjustments in the valve pressure. ETV and early introduction of levodopa therapy in patients who developed postventriculoperitoneal shunt Parkinsonism seems to be the most effective combination, with satisfactory clinical response in the medium/long term.
Keywords: Hydrocephalus, Secondary Parkinson disease, Ventriculoperitoneal shunt
INTRODUCTION
Parkinsonism secondary to the treatment of obstructive hydrocephalus due to cerebral aqueduct stenosis, with ventricular peritoneal (VP) shunt implantation, is a rare complication,[
CASE REPORT
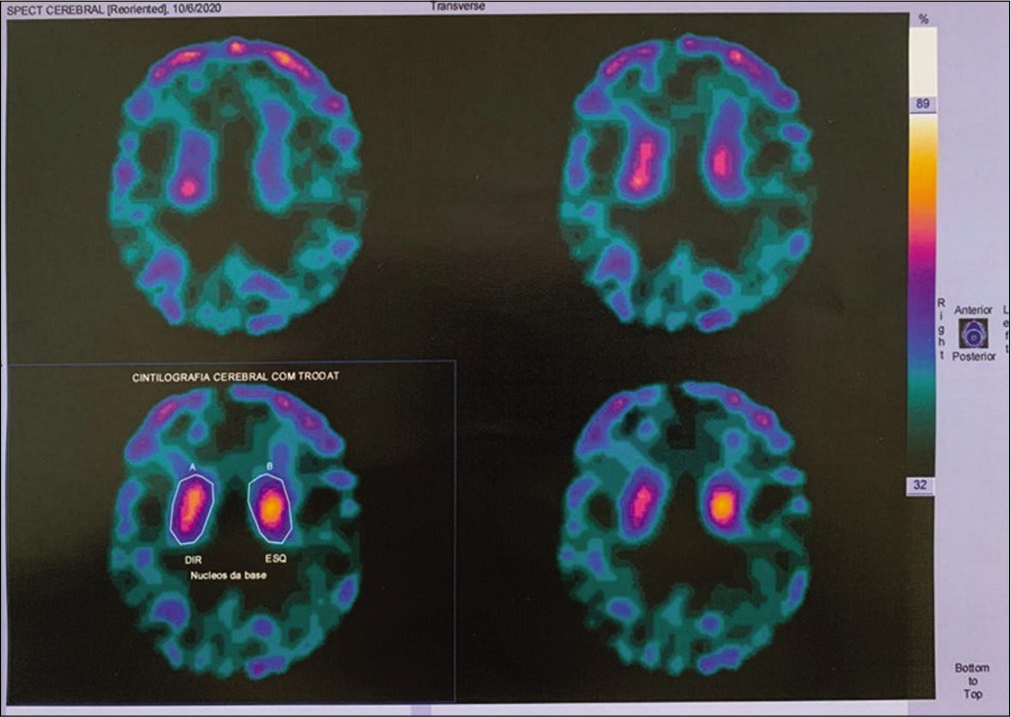
A 38-year-old male with a history of moderate-intensity daily headache, complained of a deteriorating headache at 2 months before admission, with no changes in the neurological examination. Magnetic resonance imaging (MRI) showing hypertensive hydrocephalus associated with cerebral aqueduct stenosis. At first, it was decided to perform a VP shunt due to the unfavorable anatomy of the third ventricle floor, which showed a distance of approximately 2 mm from the top of the basilar artery. A VP shunt was performed, with good initial response, and the patient was discharged 72 h later, asymptomatic. An adjustable pressure valve was inserted, with the initial opening pressure set at 14 cm H2O. After a week, he returns complaining of an important orthostatic headache, which restricted him to bed. The valve pressure was then regulated to 20 cm H2O, again with resolution of the condition. He remains well for about 75 days postoperatively, but then gradually developed headache and visual turbidity, which led him into a new MRI that revealed a ventriculomegaly, without imaging signs of intracranial hypertension. Due to this situation, the valve pressure was set at 17 cm H2O. He returned after 3 days with Parinaud’s syndrome and lowered level of consciousness, which slightly improved when valve pressure was decreased to 14 cm H2O, although the paired gaze and sleepiness persisted. As his condition worsened, despite changes in valve pressure, he was urgently submitted to a system overhaul and a new programmable valve was set at 14 cm H2O and an antigravity mechanism at 25 cm H2O. Immediate postoperative exhibited period with ideomotor slowing, loss of cervical tone, and preserved consciousness, imaging examinations showed adequate control of hydrocephalus, without signs of intracranial hypertension. After 2 weeks, he was readmitted with mental confusion, bilateral mydriasis, and left abducens nerve palsy, neuroimaging revealed hydrocephalus with signs of intracranial hypertension. The patient was referred for urgent endoscopic ventriculostomy, closure of the VP shunt system with ligation of the distal catheter at the level of the clavicle and intracranial pressure (ICP) catheter implantation for monitoring the intracranial pressure for 72 h, which proved to be normal throughout the period. In the intensive care unit, the patient’s level of consciousness improved, but he shortly developed severe Parkinsonian syndrome, characterized by asymmetric stiffness, resting tremor, anarthria, hypomimia, and cogwheel rigidity. 99mTc-ethyl cysteinate dimer (ECD) bicisate single-photon emission computed tomography (SPECT) showed low fixation of the dopamine transporter in the striated nuclei bilaterally [
DISCUSSION
Parkinsonism secondary to VP shunt is an uncommon situation that usually occurs mainly in patients who present hydrocephalus, associated with aqueductal stenosis and failures in ventricular shunt with periods of hyperdrainage.[
The main hypothesis is the occurrence of a lesion of the rostral portion of the midbrain, including the nigrostriatal pathway and/or basal ganglia.[
However, the most striking aspect of this case was the patient’s paradoxical responses to variations in valve pressure even when there was a small change in pressure and changes in cerebrospinal fluid (CSF) dynamics even after long periods of stability. The cases found in the literature to date [
SPECT revealed low bilateral fixation of TRODAT-Tc by striated nuclei, common in ongoing Parkinsonism. Patients with defect in the dopaminergic pathways, evidenced by 99mTc-ECD SPECT, tend to respond more effectively to oral therapy with levodopa to treat Parkinsonism symptoms,[
After performing an ETV, there was stabilization of the ICP and resolution of the patient’s hydrocephalus, but with worsening of the motor symptoms of Parkinsonism, which had already started. Some studies[
The patient in question presented initial resistance to treatment with levodopa in the 1st weeks but showed positive results from the increase in dose and maintenance of therapy, progressively acquiring independence in his daily activities, with significant improvement of tremors and resolution of stiffness. All these information make us believe that Parkinsonism secondary to VP shunt may be a reversible condition, yet with some patients with varying degrees of neurological sequelae.[
CONCLUSION
Despite a pathophysiology well described and suggested by the literature for the development of secondary Parkinsonism, there is still no explanation for the fact that our patient exhibited a change in the dynamics of the CSF flow after long periods of stability as well as severe neurological changes with small changes in opening pressure of the valve.
The low uptake of TRODAT by striated nuclei in brain scintigraphy using the 99mTc-ECD SPECT technique, as seen in our patient, supports the hypothesis that this group of patients responds more effectively to treatment with levodopa.[
ETV and the early introduction of levodopa therapy in patients who developed post-VP shunt Parkinsonian syndrome seem to be the most effective therapeutic combination in the management of these patients, mostly evolving with a satisfactory clinical response in the medium/ long term.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aggarwal S, Childers MK, Jimenez D. Use of carbidopalevodopa in a patient with hydrocephalus and frozen movement. Brain Inj. 1997. 11: 831-6
2. Bergsneider M, Peacock WJ, Mazziotta JC, Becker DP. Beneficial effect of siphoning in treatment of adult hydrocephalus. Arch Neurol. 1999. 56: 1224-9
3. Broggi M, Redaelli V, Tringali G, Restelli F, Romito L, Schiavolin S. Normal pressure hydrocephalus and parkinsonism: Preliminary data on neurosurgical and neurological treatment. World Neurosurg. 2016. 90: 348-56
4. Chun MH, Kang CG, Kong EJ, Chang MC. Parkinsonism after external ventricular drainage in a patient with intraventricular hemorrhage. J Stroke Cerebrovasc Dis. 2015. 24: e75-8
5. Greenberg DA, Aminoff MJ, Simon RP.editors. Neurologia Clínica. Porto Alegre: AMGH; 2014. p.
6. Hashizume A, Watanabe H, Matsuo K, Katsuno M, Tanaka F, Nagatani T. Endoscopic third ventriculotomy improves parkinsonism following a ventriculo-peritoneal shunt in a patient with non-communicating hydrocephalus secondary to idiopathic aqueduct stenosis. J Neurol Sci. 2011. 309: 148-50
7. Ochiai H, Yamakawa Y, Miyata S, Kawasoe T. L-dopa effective parkinsonism appeared after shunt revision of the aqueductal stenosis: Report of two cases. No To Shinkei. 2000. 52: 425-9
8. Okawa S, Sanpei Y, Sugawara M, Nakazawa M, Endo T, Ohnishi H. Parkinsonism improved with levodopa after endoscopic third ventriculostomy in shunted hydrocephalus due to aqueductal stenosis. Neurologist. 2015. 20: 4-7
9. Prashantha DK, Netravathi M, Ravishankar S, Panda S, Pal PK. Reversible parkinsonism following ventriculoperitoneal shunt in a patient with obstructive hydrocephalus secondary to intraventricular neurocysticercosis. Clin Neurol Neurosurg. 2008. 110: 718-21
10. Racette BA, Esper GJ, Antenor J, Black KJ, Burkey A, Moerlein SM. Pathophysiology of parkinsonism due to hydrocephalus. J Neurol Neurosurg Psychiatry. 2004. 75: 1617-9
11. Yomo S, Hongo K, Kuroyanagi T, Kobayashi S. Parkinsonism and midbrain dysfunction after shunt placement for obstructive hydrocephalus. J Clin Neurosci. 2006. 13: 373-8
12. Zeidler M, Dorman PJ, Ferguson IT, Bateman DE. Parkinsonism associated with obstructive hydrocephalus due to idiopathic aqueductal stenosis. J Neurol Neurosurg Psychiatry. 1998. 64: 657-9
13. Zhou J, Chen Y, Huang C, Ming Y, Xiang W, Li S. Parkinsonism after chronic subdural haematoma followed by ventriculoperitoneal shunt for obstructive hydrocephalus: A case report. Br J Neurosurg. 2019. 33: 302-4