- Department of Neurosurgery, Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia.
- Department of Neurosurgery, Universitas Airlangga - Faculty of Medicine, Dr. Soetomo Academic General Hospital, Surabaya, East Java, Indonesia.
Correspondence Address:
Muhammad Arifin Parenrengi, Department of Neurosurgery, Dr. Soetomo Academic General Hospital, Surabaya, East Java, Indonesia.
DOI:10.25259/SNI_283_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Muhammad Azzam1, Roidah Taqiyya Zahra Wathoni1, Wihasto Suryaningtyas2, Muhammad Arifin Parenrengi1. Pediatric shunt revision analysis within the first year of shunt placement: A single center experience. 24-Aug-2021;12:419
How to cite this URL: Muhammad Azzam1, Roidah Taqiyya Zahra Wathoni1, Wihasto Suryaningtyas2, Muhammad Arifin Parenrengi1. Pediatric shunt revision analysis within the first year of shunt placement: A single center experience. 24-Aug-2021;12:419. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11066
Abstract
Background: Hydrocephalus is a common problem in neurosurgery with shunt placement remains the mainstay of the management. However, shunt placement generally requires following surgical procedures, including shunt revision. Despite the recent developments, the incidence of shunt failure remains high, approximately 30–51% in the 1st year following the shunt placement.
Methods: An observational retrospective study of pediatric neurosurgery patients whom underwent CSF shunting procedure, both primary and repeated VPS, VAS, CPS, and subdural-peritoneal shunt procedures between January 2018 and May 2019. The patients were observed for 12 months for potential complication requiring shunt revision following the shunt placement.
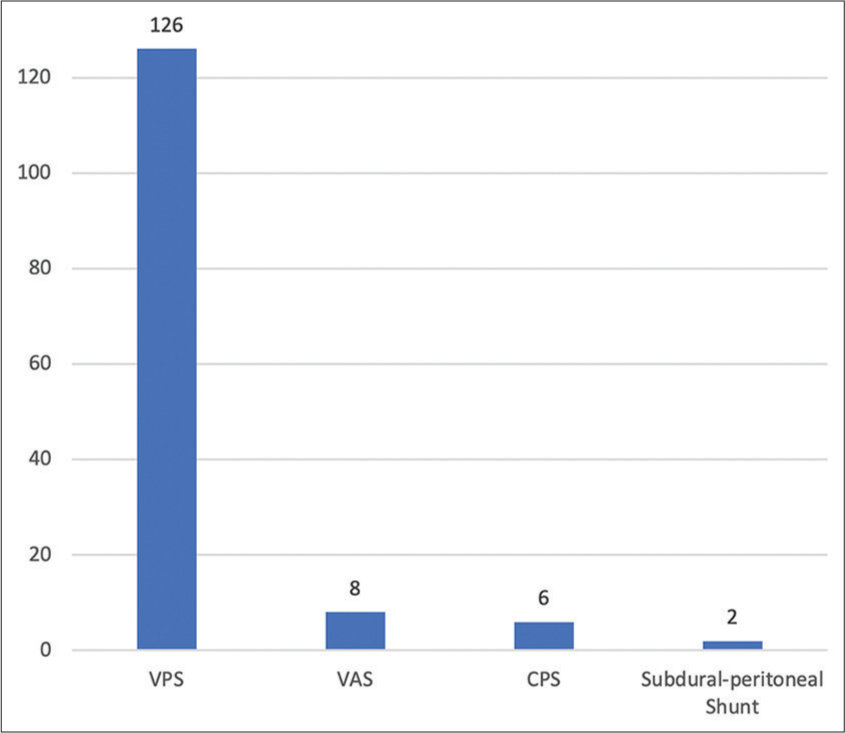
Results: A total of 142 patients underwent shunt placement. The shunt revision within 12 months was found in 26 patients (18.3%), 25 cases were VPS (96.2%) and one case was CPS (3.8%). The mean period of time between shunt placement to shunt revision was 3.96 months. Age of under 6 months old during the shunt placement showed significantly higher risk for shunt revision (RR 2.32 CI 1.13–4.74, P = 0.018). The most common diagnosis requiring shunt revision was congenital anomaly (16 cases, 61.5%). The most common cause of revision was shunt malfunction, with 21 cases (80.8%) followed by infected shunt with 5 cases (19.2%).
Conclusion: The 1st year observation showed relatively high rate for shunt revision. The patient underwent shunt procedure should be regularly followed up in long period for better evaluation of the outcome. The application of shunt registry in some countries appears to be efficient and beneficial for sustainable follow-up in patients underwent shunt placement.
Keywords: Cerebrospinal fluid shunt, Hydrocephalus, Pediatric, Shunt revision
INTRODUCTION
Hydrocephalus is defined as an enlargement of the ventricular system of the brain caused by obstruction in cerebrospinal fluid (CSF) flow, increased CSF production, and disturbance of its absorption into the systemic circulation.[
Placement of CSF shunt for diversion remains a mainstay for treating patients with hydrocephalus, even though surgical complications remain high, becoming a medical and social problem. However, shunt complications generally require several surgical procedures, including shunt revision, during a patient’s lifetime. Studies showed that the incidence of shunt failure is approximately 30–51% in the 1st year after shunt placement.[
Some studies have conveyed the pediatric shunt revision rate in the 1st year after the placement with varying result.[
MATERIALS AND METHODS
A retrospective observational study of pediatric-neurosurgery patients requiring shunting procedure from January 2018 to May 2019. The period of implementation of Hydrocephalus Clinical Research Network (HCRN) protocol in Dr. Soetomo General Academic Hospital was started in 2018. The shunting procedures included are ventriculoperitoneal shunt (VPS), ventriculoatrial shunt (VAS), cystoperitoneal shunt (CPS), and subdural-peritoneal shunt. Shunting procedures performed outside Dr. Soetomo General Academic Hospital, follow-up period under 12 months, and shunt revisions following shunt exteriorization and foregoing revision were excluded from the study.
The patients’ age was defined in months and categorized as neonates (within a month old), infants (age 1–12 months), and children (age >12 months). The diagnosis is categorized into infection, congenital, tumor, and hemorrhage. The shunt procedure is divided into emergency, performed in an emergency operating theater, and urgent, in a neurosurgery operating theater. The shunt procedures were in line with the HCRN protocol except for antibiotic-impregnated catheter (AIC) as our health-care system did not provide it. The shunt procedure was categorized into primary for the 1st time insertion and repeated insertion.
The patients were divided into those who underwent and did not undergo revision under 12 months of follow-up. The number of revision procedure was observed within a year after the shunt insertion. The cause of revision was divided into infected shunt and shunt malfunction.
The data were analyzed using IBM SPSS Statistics version 25 for Mac to describe the characteristics of patients underwent shunting and revision procedure and to estimate risk using univariate and Chi-square analyses.
RESULTS
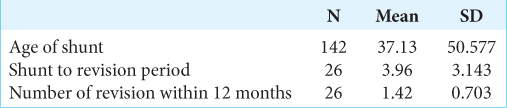
A total of 142 patients underwent shunt insertion procedure in our center. Sixty-nine patients (48.6%) were male and 73 patients (51.4%) were female. The mean age for the reported shunt insertion was 37 months old [
The shunt revision within 12 months was found in 26 patients (18.3%) with the mean period of time between the shunt procedure to the shunt revision was 3.96 months. The mean number of revisions within 12 months of follow-up was 1.42 [
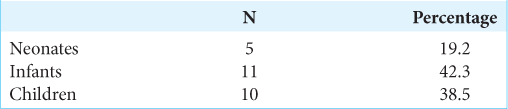
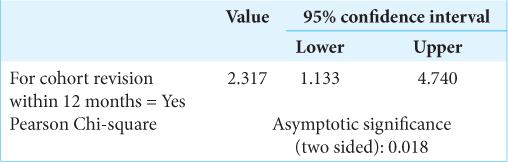
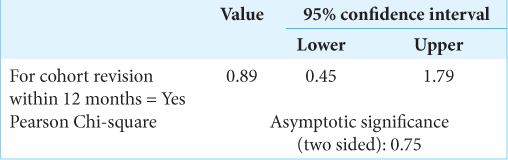
The univariate analysis showed a significantly higher risk for shunt revision within 12 months (RR: 2.32 CI: 1.13–4.74, P = 0.018) on patients under the age of 6 months on the time of the shunt procedure [
DISCUSSION
The CSF shunt procedure conducted in our center is in line with the HCRN protocol 2016 except for the use of AIC. This specific designated catheter is suggested to be able to reduce infection rate among shunt procedures after the univariate analysis[
Shunt insertion for CSF diversion becomes one of the procedures most prone to failure. Some studies showed the incidence of shunt failure of around 30–51% in the 1st year after the shunt insertion[
The causes of revision in our center were classified into two general categories; malfunction and infection. The malfunctions that lead to shunt revision include shunt obstruction, mechanical shunt failure, over-drainage of the shunt, and distal catheter site-specific failures. The most common cause of shunt revision in our center was shunt malfunction, as many as 80.8% within the 12 months after the shunt procedure.
The advancements of recent technology to assist the shunt placement, for example, endoscopic shunt placement and frameless stereotactic image guidance have not yet resulted in the decrease of shunt failures leading to shunt revisions.[
The risk of shunt revision was significantly higher in patients under 6 months old during the shunt procedure (RR: 2.32 CI: 1.13–4.74, P = 0.018). This finding is consistent with the previous studies where patients under 6 months old had significantly higher risk of shunt revision compared to rest of the study population (P < 0.001).[
VPS was the most common type of shunt requiring revision in our center (96.2%). VPS was found to be a predictive factor for preventable shunt failure compared to the other types of shunt with the risk of shunt failure which is highest during the first 6–12 months.[
CONCLUSION
Shunt procedure has long been known to have complications leading to shunt revision. The 1st year of follow-up showed relatively high rates of shunt revision with continuously increasing risk over the year. Patients undergoing shunt procedures should be regularly followed up in long period for better evaluation of the outcome. The application of shunt registry in some countries is efficient and beneficial for sustainable follow-up in patients who had a shunt procedure.
Study limitation
This study has several limitations. The design of study was a retrospective single-center study, possibly preventing us to identify patients who underwent shunt revision in another hospital. The cause of shunt revision was classified into two major groups, infection and malfunction, which might require further investigation for better results. Future studies with multicenter involvement and longer follow-up period should be performed for better depiction and explanation of shunt revision in Indonesia.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge Dr. Soetomo General Academic Hospital and all attendings and members of Neurosurgery Department for assistance in the execution of this project.
References
1. Browd SR, Ragel BT, Gottfried ON, Kestle JR. Failure of cerebrospinal fluid shunts: Part I: Obstruction and mechanical failure. Pediatr Neurol. 2006. 34: 83-92
2. Buster BE, Bonney PA, Cheema AA, Glenn CA, Conner AK, Safavi-Abbasi S. Proximal ventricular shunt malfunctions in children: Factors associated with failure. J Clin Neurosci. 2016. 24: 94-8
3. Dave P, Venable GT, Jones TL, Khan NR, Albert GW, Chern JJ. The preventable shunt revision rate: A multicenter evaluation. Clin Neurosurg. 2019. 84: 788-97
4. Garne E, Loane M, Addor MC, Boyd PA, Barisic I, Dolk H. Congenital hydrocephalus-prevalence, prenatal diagnosis and outcome of pregnancy in four European regions. Eur J Paediatr Neurol. 2010. 14: 150-5
5. Gonzalez DO, Mahida JB, Asti L, Ambeba EJ, Kenney B, Governale L. Predictors of ventriculoperitoneal shunt failure in children undergoing initial placement or revision. Pediatr Neurosurg. 2016. 52: 6-12
6. Hanak BW, Bonow RH, Harris CA, Browd SR. Cerebrospinal fluid shunting complications in children. Pediatr Neurosurg. 2017. 52: 381-400
7. Hasanain AA, Abdullah A, Alsawy MF, Soliman MA, Ghaleb AA, Elwy R. Incidence of and causes for ventriculoperitoneal shunt failure in children younger than 2 years: A systematic review. J Neurol Surg A Cent Eur Neurosurg. 2019. 80: 26-33
8. Isaacs AM, Riva-Cambrin J, Yavin D, Hockley A, Pringsheim TM, Jette N. Age-specific global epidemiology of hydrocephalus: Systematic review, metanalysis and global birth surveillance. PLoS One. 2018. 13: 1-24
9. Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F. Long-term follow-up data from the shunt design trial. Pediatr Neurosurg. 2000. 33: 230-6
10. Kestle JR, Holubkov R, Cochrane DD, Kulkarni AV, Limbrick DD, Luerssen TG. A new hydrocephalus clinical research network protocol to reduce cerebrospinal fluid shunt infection. J Neurosurg Pediatr. 2016. 17: 391-6
11. Pan P. Outcome analysis of ventriculoperitoneal shunt surgery in pediatric hydrocephalus. J Pediatr Neurosci. 2018. 13: 176-81
12. Rekate HL. A contemporary definition and classification of hydrocephalus. Semin Pediatr Neurol. 2009. 16: 9-15
13. Riva-Cambrin J, Kestle JR, Holubkov R, Butler J, Kulkarni AV, Drake J. Risk factors for shunt malfunction in pediatric hydrocephalus: A multicenter prospective cohort study. J Neurosurg Pediatr. 2016. 17: 382-90
14. Sainte-Rose C, Piatt JH, Renier D, Pierre-Kahn A, Hirsch JF, Hoffman HJ. Mechanical complications in shunts. Pediatr Neurosurg. 1991. 17: 2-9
15. Stone JJ, Walker CT, Jacobson M, Phillips V, Silberstein HJ. Revision rate of pediatric ventriculoperitoneal shunts after 15 years: Clinical article. J Neurosurg Pediatr. 2013. 11: 15-9
16. Tervonen J, Leinonen V, Jääskeläinen JE, Koponen S, Huttunen TJ. Rate and risk factors for shunt revision in pediatric patients with hydrocephalus-a population-based study. World Neurosurg. 2017. 101: 615-22
17. Tuli S, Drake J, Lawless J, Wigg M, Lamberti-Pasculli M. Risk factors for repeated cerebrospinal shunt failures in pediatric patients with hydrocephalus. J Neurosurg. 2000. 92: 31-8