- Department of Neurosurgery, Faculty of Medicine, Helwan University, Cairo, Egypt.
- Department of Neurosurgery, Faculty of Medicine, Benha University, Benha, Al Qalubia, Egypt.
Correspondence Address:
Mohamed Atef Elnokaly
Department of Neurosurgery, Faculty of Medicine, Benha University, Benha, Al Qalubia, Egypt.
DOI:10.25259/SNI_676_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamed Atef Elnokaly1, Mohammed M. Adawi2, Ahmed M. Nabeel2. Pedicular lumbosacral spine fusion for adult/adolescent lumbar developmental high-grade spondylolisthesis. 04-Dec-2020;11:416
How to cite this URL: Mohamed Atef Elnokaly1, Mohammed M. Adawi2, Ahmed M. Nabeel2. Pedicular lumbosacral spine fusion for adult/adolescent lumbar developmental high-grade spondylolisthesis. 04-Dec-2020;11:416. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10429
Abstract
Background: Few series report on the management of high-grade spondylolisthesis (HGS) in adolescents and young adults. This review highlights a series of six consecutive cases with developmental (dysplastic) HGS successfully managed with L3 or L4 to S1 transpedicular screw placement, rather than in situ/noninstrumented lumbosacral fusion.
Methods: The six patients with HGS, according to the Meyerding Grading, presented with low back pain and bilateral sciatica (2016–2020). Patients averaged 19.8 years of age and underwent posterior transpedicular L3 or L4-S1 screw fusions. They were all monitored for at least 6 postoperative months.
Results: None of the six patients developed any major perioperative/postoperative complications; only one patient had severe postoperative back pain that slowly improved over 3 months. All the patients were clinically improved postoperatively, uniformly demonstrated fusion on postoperative CT studies, and considered the operation worthwhile.
Conclusion: Posterior transpedicular screw fixation of the lumbosacral spine is an efficient and safe technique for the treatment of L3 or L4 to L5-S1 HGS. It is a suitable instrumented technique for managing adult/adolescent HGS and offers an alternative to the more typically performed in situ/noninstrumented L4-S1 procedures.
Keywords: Adolescent spine, Developmental spondylolisthesis, High-grade spondylolisthesis, In place fusion, Transvertebral fusion
INTRODUCTION
Lumbar spondylolisthesis is a common spinal problem and is presented in about 5% of the population. However, high-grade spondylolisthesis (HGS) according to the Meyerding[
The following pathology characterizes congenital spondylolisthesis; L5 subluxation over the sacrum due to pars defects, hypoplastic L5 and S1 facets, and a “dooming” sacrum.[
MATERIALS AND METHODS
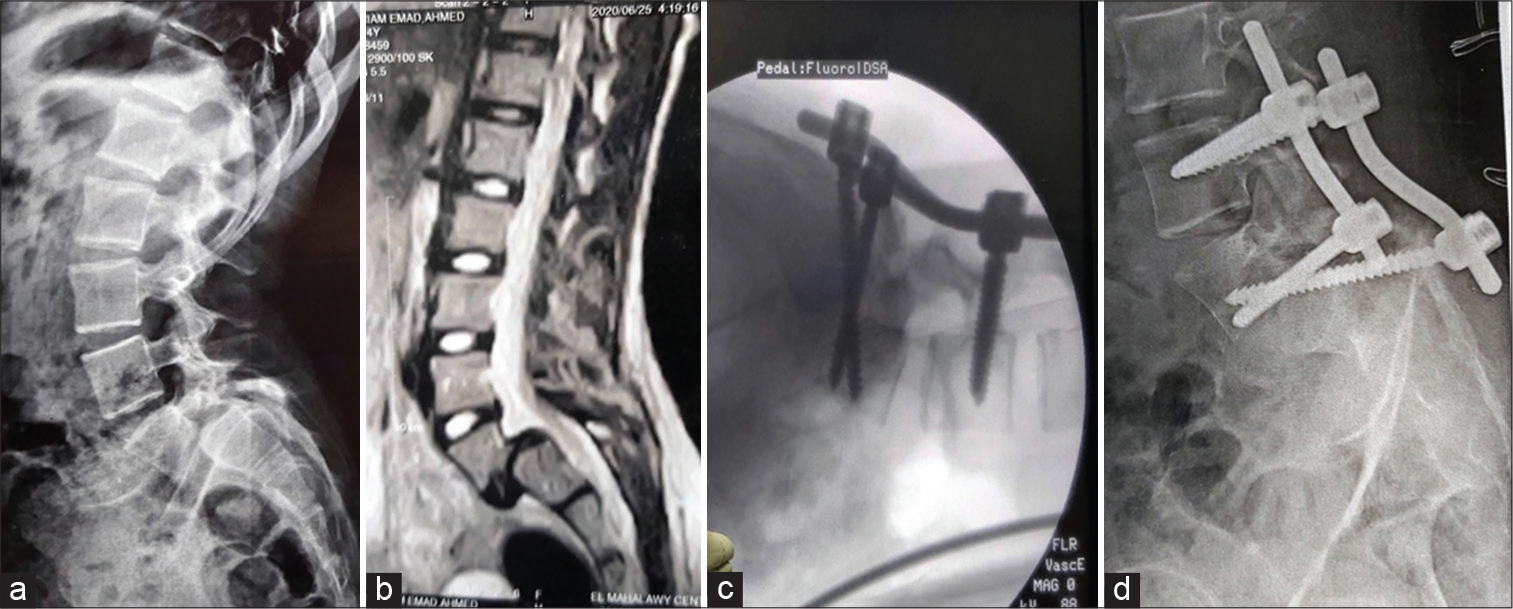
We retrospectively reviewed six consecutive patients with HGS (2016–2020), averaging 19.5 years of age [
All six patients underwent transpedicular L3 or L4 to L5-S1 fusions without reduction of the slip. Relief of symptoms (subjectively) was recorded over the minimum follow-up period of 6 postoperative months. Outcomes were evaluated utilizing the visual analog score (VAS) for low back pain and Oswestry disability index (ODI). Further, postoperative radiological bone fusion was documented over a minimum of 6 months on CT scans/plain radiographs. [
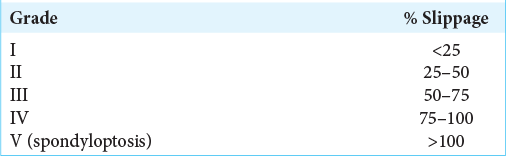
Figure 1:
Female patient, house wife, 27 years old, presented by low back pain, bilateral sciatica and flexion attitude. Pre-operative image; (a) Plain x-ray lumbar spine, lateral view, (b) MRI lumbosacral spine, sagittal view showing HGS. Post-operative images CT lumbosacral spine, (c) sagittal view, showing the screws and limit of its reach, (d) axial view showing triangular arrangement of the transvertebral screws, 16 months following surgery.
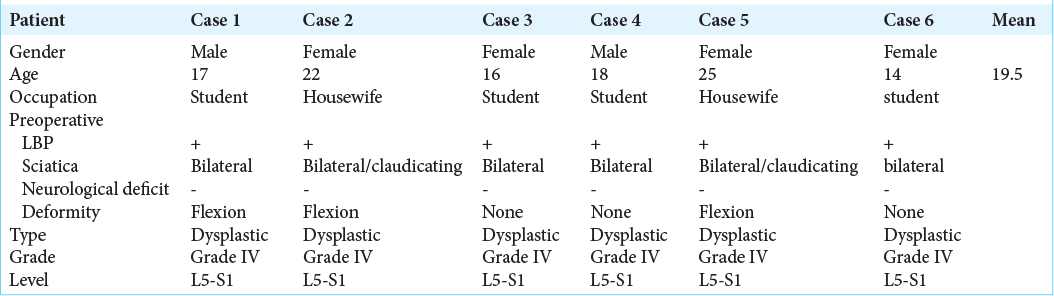
Figure 2:
Male student, armature soccer player 17 years old, presented with low back pain, bilateral sciatica and flexion attitude (Resembling tight hamstring). 56 months fu, returned back to his sport. Pre-operative images, (a) Plain x-ray lumbar spine, lateral view, (b) MRI lumbosacral spine, sagittal view showing HGS. Post-operative plain X-ray lumbar images, (c) lateral view, (d) anteroposterior view after screw placement, 21 months following surgery.
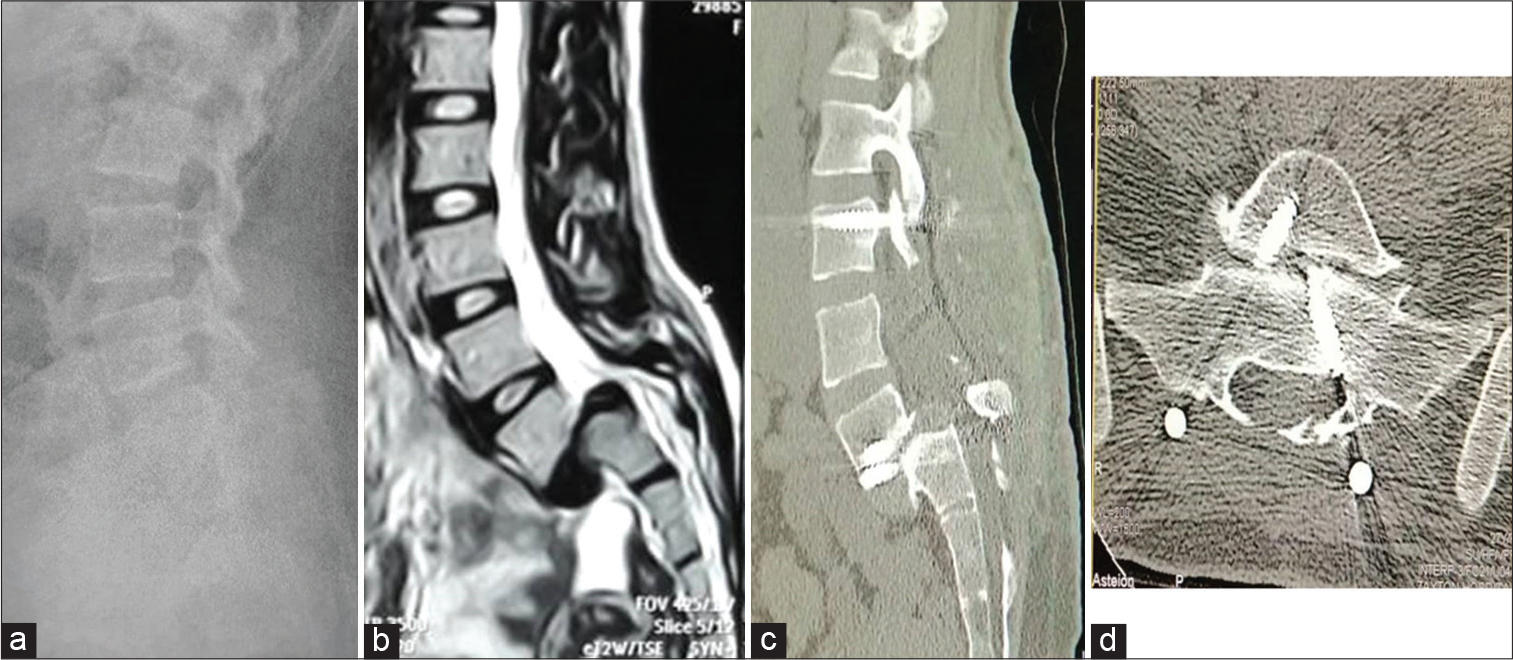
Figure 3:
Female patient, 14 years student, the youngest in our series, present to us with low back pain and unilateral sciatica. Preoperative images; (a) Plain X-ray lumbar spine, lateral and (b) MRI lumbosacral spine, sagittal view showing Grade IV spondylolisthesis. Plain X-rays lumbar spine, (c) intraoperative c-arm image, showing the screws after fully inserted, while patient is in prone position, (d) early postoperative image, lateral view showing the screws in place with patient in standing position.
Surgical technique
Standard L3 or L4 through S1 laminectomies were performed [
RESULTS
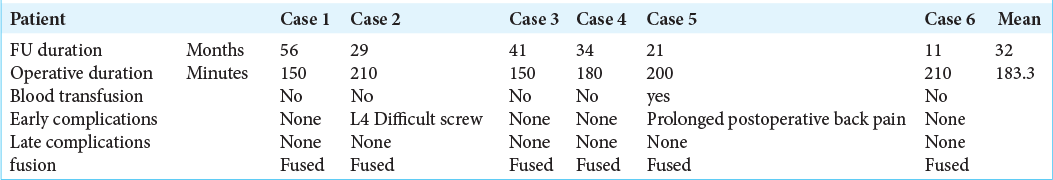
There were no major intraoperative complications (e.g., infections, hemorrhages or nerve injuries, and motor deficits), or long-term postoperative complications (e.g., instrumentation failure, slippage progression, or pseudoarthrosis) in these six patients [
Outcomes
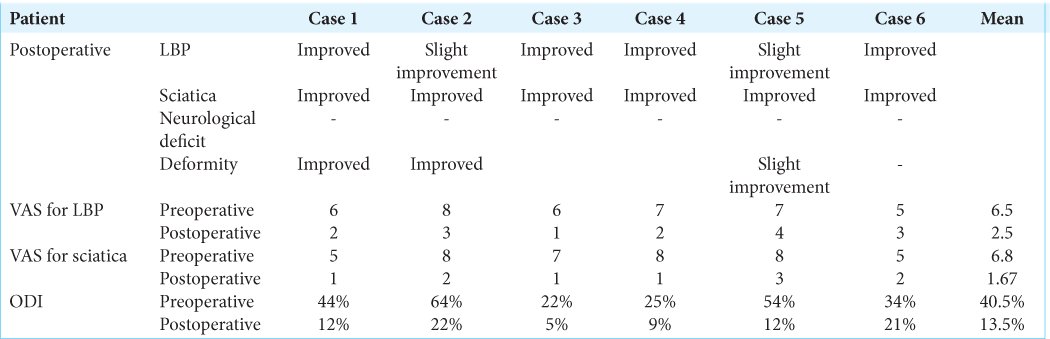
In 5 of 6 patients, radiculopathy improved on VAS and ODI scores (e.g., the latter went from 22 to 64%, mean 40.5% preoperatively, to 5-22% (mean 13.5%) postoperatively) [
DISCUSSION
Most patients with high-grade developmental spondylolistheses (HGS) develop significant slippage and symptoms during the adolescent growth period. Symptoms typically include; the onset of low back and sciatic pain that can evolve into a full-blown sciatic crisis.[
Surgical techniques for HGS management have included posterior instrumented fusion, posterolateral interbody fusion, stand-alone oblique interbody fusion, anterior fusion, L5 vertebrectomy with reduction and fusion, and circumferential in situ fusion (either two-staged or single staged posterior approach).[
We, therefore, concluded that the transpedicular instrumentation technique was more effective than the typical in situ/noninstrumented L5-S1 HGS fusion for HGS.[
CONCLUSION
Transpedicular lumbosacral L3 or L4 to L5-S1 instrumented fusions for grade IV spondylolisthesis/HGS without reduction was successfully performed in six adolescent/ young adults. This resulted in favorable outcomes and was a useful alternative to in situ/noninstrumented HGS lumbosacral fusions.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Boachie-Adjei O, Do T, Rawlins BA. Partial lumbosacral kyphosis reduction, decompression, and posterior lumbosacral transfixation in high-grade isthmic spondylolisthesis: Clinical and radiographic results in six patients. Spine (Phila Pa 1976). 2002. 27: E161-8
2. Greenberg MS.editors. Spine and spinal cord. Handbook of Neurosurgery. New York: Thieme Publishers; 2016. p. 1024-151
3. Hart RA, Domes CM, Goodwin B, D’Amato CR, Yoo JU, Turker RJ. High-grade spondylolisthesis treated using a modified Bohlman technique: Results among multiple surgeons. J Neurosurg Spine. 2014. 20: 523-30
4. Kotil K, Tunckaya T, Bilge T. Reduction of high-grade spondylolisthesis using a transvertebral surgical approach in a child. A case report and review of the literature. Turk Neurosurg. 2006. 6: 4197-201
5. Lehmer SM, Steffee AD, Gained RW. Treatment of L5-S1 spondyloptosis by staged L5 resection with reduction and fusion of L4 onto S1 (Gaines procedure). Spine (Phila Pa 1976). 1994. 19: 1916-25
6. Meyerding HW. Spondyloptosis. Surg Gynecol Obstet. 1932. 54: 371-7
7. Pizzutillo PD, Hummer CD. Nonoperative treatment for painful adolescent spondylolysis or spondylolisthesis. J Pediatr Orthop. 1989. 9: 538-40