- Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Universitas Brawijaya/Dr. Saiful Anwar General Hospital, Malang, East Java, Indonesia
Correspondence Address:
Donny Wisnu Wardhana, Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Universitas Brawijaya/Dr. Saiful Anwar General Hospital, Malang, East Java, Indonesia.
DOI:10.25259/SNI_668_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Donny Wisnu Wardhana, Farhad Bal’afif, Tommy Alfandy Nazwar, Amrina Rosyada, Wahju Sigit Tjahjono Putro, Anisa Nur Kholipah. Penetrating intraorbital wooden foreign bodies involving the right frontal lobe of the brain: A rare case report. 15-Nov-2024;15:418
How to cite this URL: Donny Wisnu Wardhana, Farhad Bal’afif, Tommy Alfandy Nazwar, Amrina Rosyada, Wahju Sigit Tjahjono Putro, Anisa Nur Kholipah. Penetrating intraorbital wooden foreign bodies involving the right frontal lobe of the brain: A rare case report. 15-Nov-2024;15:418. Available from: https://surgicalneurologyint.com/surgicalint-articles/13227/
Abstract
Background: Penetrating orbital trauma from a wooden foreign object is rare and challenging to identify, as it cannot be detected with a computed tomography (CT) scan. This report highlights the clinical presentation, diagnosis, and management of such a case.
Case Description: A 19-year-old female experienced penetrating orbital trauma from a wooden object following a traffic accident. She intermittently visited the hospital with eye swelling and headache, without visible penetrating wounds on the palpebra. The swelling persisted for weeks, accompanied by increasing signs of ocular and cerebral infection. The suspicion of a non-metallic foreign body penetrating the brain was confirmed 3 months after the initial visit, delayed by the hidden entry wound between the eyelid and eyeball and orbital edema mimicking non-penetrating trauma. A multidisciplinary team managed the case. Procedures included debridement, retro-orbital exploration, retro-orbital abscess evacuation, and frontal basal trephination exploration, successfully removing the wooden object that had penetrated the medial orbit, frontal bone, and brain, along with cerebral abscess evacuation. Postoperative CT scans showed complete removal of the foreign object and successful abscess evacuation. The patient showed improvement in ocular symptoms, resolution of headaches, and no wound leakage. She was discharged on the 14th day after completing antibiotic treatment and having the dressing removed.
Conclusion: This case is notable for its rarity, high risk of misdiagnosis, and potentially fatal consequences if not promptly managed. We emphasize the importance of patient involvement in routine consultations, careful anamnesis, clinical examination, and a multidisciplinary approach for optimal outcomes.
Keywords: Brain, Computed tomography, Orbita, Penetrating, Wooden foreign body
INTRODUCTION
Penetrating orbital trauma with breakable objects like wood often results in hidden foreign bodies.[
CASE DESCRIPTION
A 19-year-old female presented to the emergency department with complaints of a headache and swelling of the right eyelid. Initially, the patient had been involved in a single motorcycle accident, falling into a bush with many tree branches. The patient did not remember any branches striking her eye, but her right eye was swollen. A primary survey indicated that the patient was stable, with good respiratory, circulatory, and neurological functions and a Glasgow Coma Scale (GCS) score of 15. There were abrasion marks around the right orbital area and limited movement of the right eyeball [
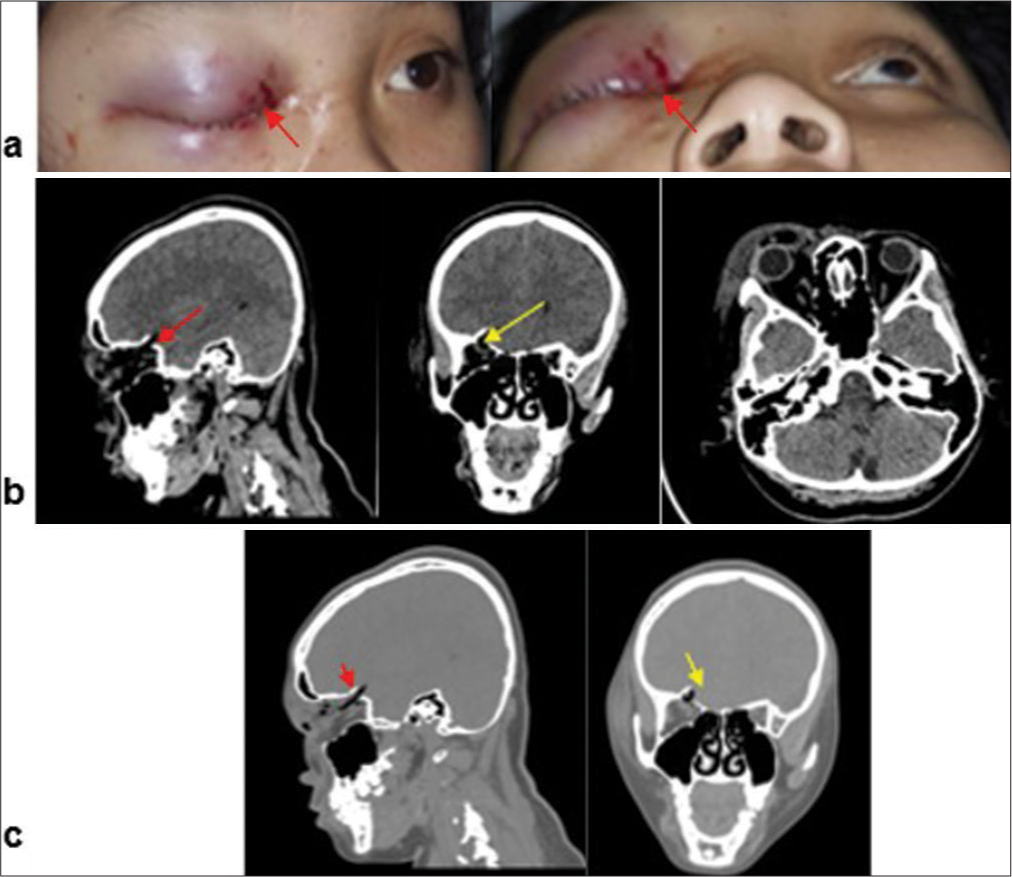
Figure 1:
Clinical appearance and imaging of the patient at the time of injury. (a) The red arrows indicate the clinical appearance of the patient’s eye at the initial visit; (b) Non-contrast CT scan of the brain window at the time of injury. The image shows a fracture of the superior orbital wall and pneumocephalus. There is no evidence of a foreign body at this time. Red and yellow arrows indicate the fracture of the superior orbital wall and pneumocephalus; (c) CT scan with a bone window. Red and yellow arrows indicate the fracture of the superior orbital wall and pneumocephalus.
Overview of brain window and bone window on a head CT scan revealed no intracranial hemorrhage but showed fracture fragments in the superior right orbit extending into the right frontal lobe, along with pneumocephalus [
Three months later, the patient visited the hospital with persistent ocular symptoms, early signs of increased intracranial pressure (ICP), and local infection [
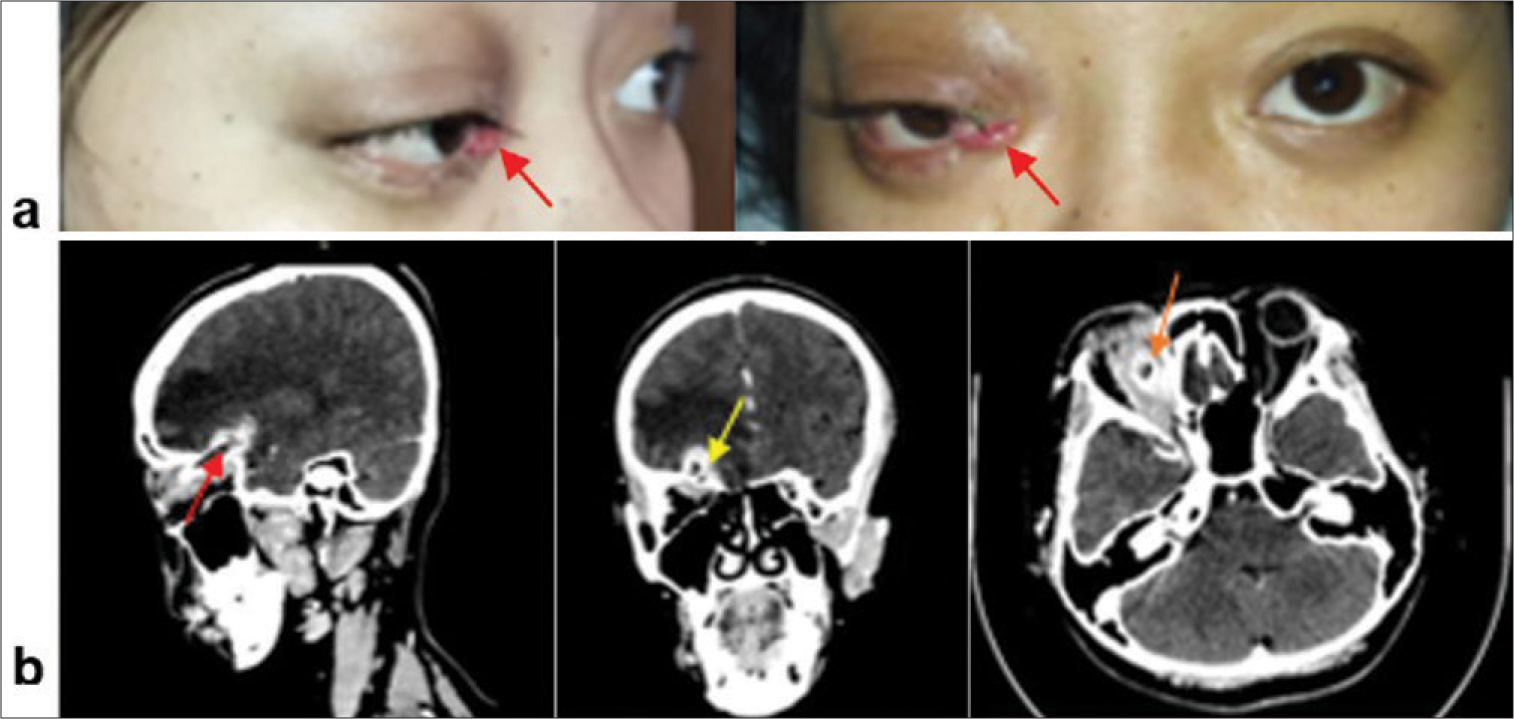
Figure 2:
Clinical appearance and imaging of the patient three months after injury. (a) The red arrows indicate the clinical appearance of the patient’s eye prior to the removal of the wooden foreign body (three months after injury); (b) Contrast-enhanced CT scan three months post-injury. The image shows an abscess extending from the retroorbital region to the right basal frontal area through a defect in the superior orbital wall. A suspicion of a foreign body is noted. Red arrow: suspected foreign body; yellow arrow: basal frontal abscess; orange arrow: retroorbital abscess.
At the initial evaluation, the low-density linear region in the CT scan from the orbit to the right frontal base was initially suspected to be pneumocephalus due to the patient’s orbital fracture and trauma history. However, the shape and the clinical progression raised suspicion of a potential foreign object, even though wooden IOFBs are difficult to detect on imaging. The possibility of a wooden foreign body was not considered in the initial diagnosis due to the lack of visible skin wounds or traumatic entry points in the orbit.
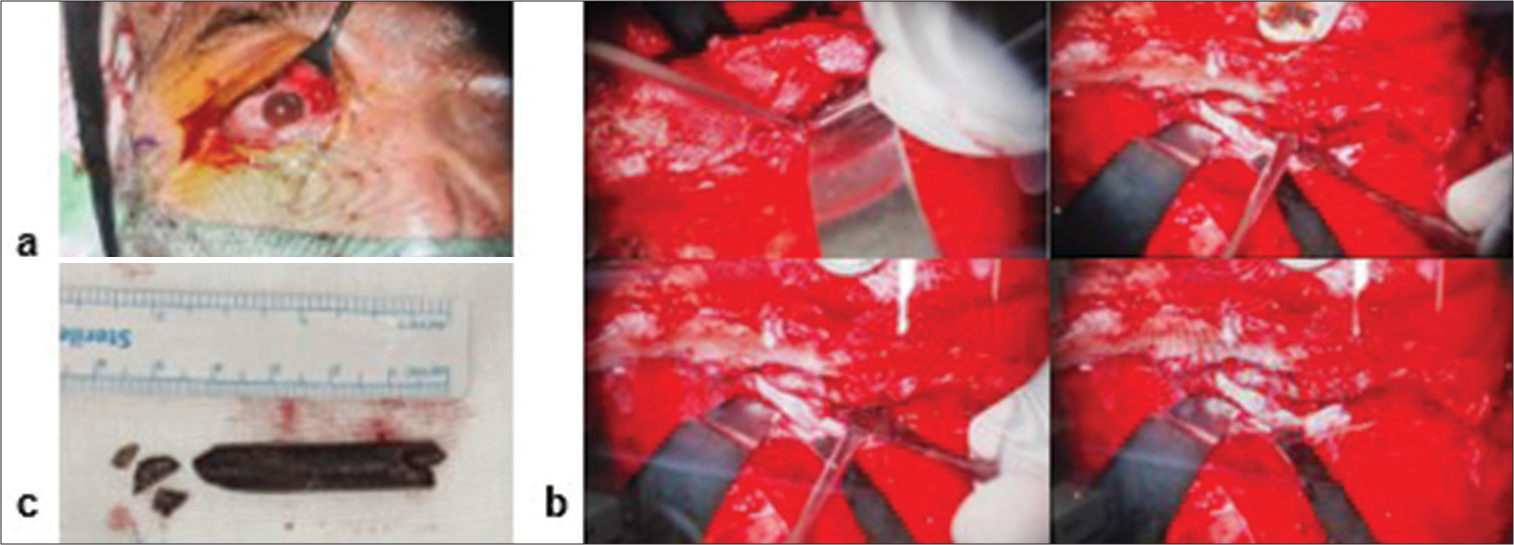
The patient underwent surgery performed by a multidisciplinary team consisting of neurosurgeons, plastic surgeons, and ophthalmologists. The procedure included debridement, retro-orbital exploration, exploratory trepanation with a subfrontal approach, and abscess evacuation [
Figure 3:
Intraoperative images. (a) Exploration of the entry wound of the foreign body inside the palpebral and right eyeball; (b) exploration of the foreign body and abscess evacuation through surgery using a bicoronal subfrontal approach; and (c) view of the wooden foreign body and its fragments, measuring 4–5 cm in length and ±1 cm in width.
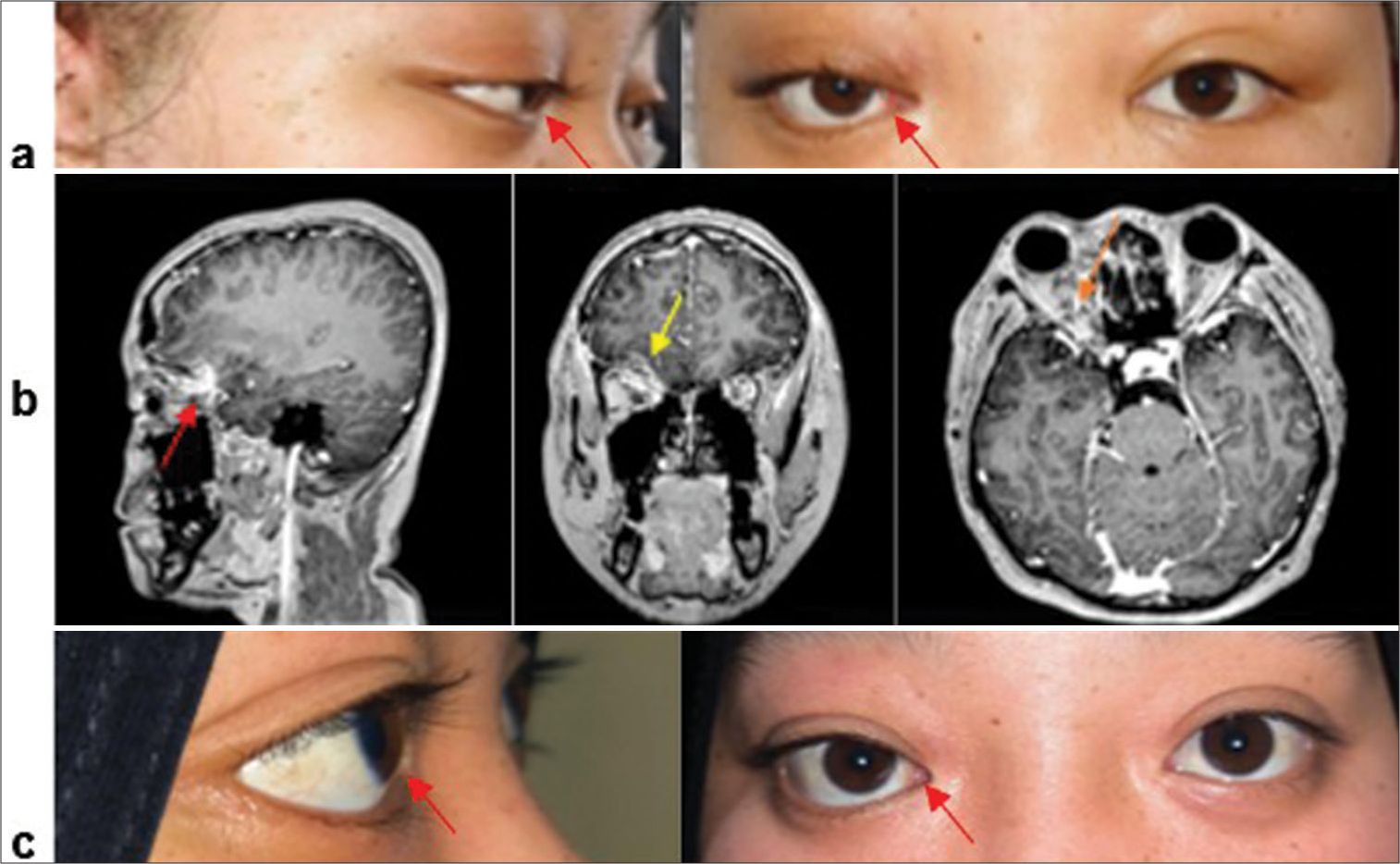
After debridement, foreign body removal, and a 2-week treatment with antibiotics, including ceftriaxone and metronidazole, we evaluated the patient’s ocular [
Figure 4:
Clinical appearance and imaging of the patient after surgery. (a) The red arrows indicate the clinical appearance of the patient’s eye following the removal of the wooden foreign body; (b) MRI two weeks post-surgery and antibiotic treatment. Red arrow: no mass observed; yellow arrow: no basal frontal abscess observed; orange arrow: no retroorbital abscess observed; (c) The red arrows indicate the clinical appearance of the patient’s eye three months after the removal of the wooden.
DISCUSSION
The presence of a wooden foreign body in the orbit, extending into the intraparenchymal region of the right frontal lobe, is a rare occurrence that can lead to severe injuries to both the orbit and the brain. Thorough anamnesis and clinical examination of the injury are crucial for establishing an accurate diagnosis and determining appropriate surgical intervention, thereby reducing the rate of reoperation and optimizing patient outcomes.[
When injury occurs, foreign bodies can either pass through or be embedded in the space between the eyeball and the orbital bone wall.[
Common clinical manifestations resulting from foreign body penetration include orbital cellulitis, orbital hematoma, proptosis, ptosis, ocular motility disorders, superior orbital fissure syndrome, and orbital apex syndrome.[
In addition to causing orbital damage, a wooden object penetrating the brain without prompt removal can lead to acute inflammatory reactions. The risk of infection with retained wooden foreign bodies can be as high as 64% due to the porous consistency and organic nature of wood, which provides a favorable medium for bacterial growth.[
In our case, the CT scan played a crucial role in establishing the diagnosis and planning the surgery. CT imaging helps assess the extent of the lesion, localize foreign bodies and bone fragments, detect hematomas, and determine the penetration path.[
In this case, the initial suspicion of pneumocephalus led to a delayed diagnosis of the wooden foreign body. Wooden foreign bodies are difficult to detect due to their similar density to air in the acute phase, and their appearance can easily be missed on CT scans. Moreover, the lack of visible entry points further complicated the diagnosis. Identifying wooden foreign bodies requires careful evaluation of clinical symptoms, persistence of symptoms, and consideration of the possibility, even in cases with subtle imaging findings.
In this case, the patient experienced a delayed diagnosis of a penetrating wooden foreign body in the brain for up to 3 months. Suspicion of a foreign body arose following persistent ocular symptoms of proptosis, early signs of ICP, and local infection. CT- and contrast-enhanced MRI focused on the skull base revealed an abscess in the retro-orbital space and a frontal basal brain abscess. These abscesses were suspected to be caused by a non-metallic foreign body that was difficult to detect with CT or MRI. The difficulty in establishing a diagnosis at the initial visit was due to the hidden entry point of the wooden foreign body between the bulbus oculi and conjunctiva (without skin wounds). This condition was accompanied by orbital edema resembling non-penetrating ocular trauma. Active patient engagement through regular consultations was crucial in detecting this case early.
Diagnosis of a wooden foreign body must be promptly followed by appropriate management.[
Three months postoperation, the patient had normal visual function with minimal rightward eye movement deficit. There were no signs of infection, enabling the patient to return to normal activities and work [
CONCLUSION
In this report, we present a case and management of penetrating orbital trauma caused by a wooden foreign body that resulted in damage to both the eye and the brain. We encountered significant challenges in establishing the diagnosis, leading to a 3-month delay in diagnosing the penetrating foreign body injury to the brain. In our case, the wooden foreign body was difficult to identify due to the hidden location of the entry wound and orbital edema that resembled non-penetrating ocular trauma. This situation required a careful and thorough anamnesis and clinical examination of the injury. We successfully managed this case through surgical intervention by a multidisciplinary team comprising neurosurgery, plastic surgery, and ophthalmology specialists. Our findings emphasize the crucial role of patient involvement in regular consultations, careful anamnesis and clinical examination, and the involvement of a multidisciplinary team in establishing the diagnosis and determining appropriate surgical interventions.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chai GR, Chen M, Song ZX, Liu L. Clinical features, radiological imaging, and treatment strategies of nonmetallic intraorbital foreign bodies: A retrospective analysis. Int J Ophthalmol. 2023. 16: 1130-7
2. Chowdhary S, Garg P, Sawhney V, Pandya A, Sambhav K, Gupta S. Unusual missed diagnosis of foreign body: A case report. Int Med Case Rep J. 2020. 13: 187-90
3. Li J, Zhou LP, Jin J, Yuan HF. Clinical diagnosis and treatment of intraorbital wooden foreign bodies. Chin J Traumatol. 2016. 19: 322-5
4. Nazwar TA, Bal’afif F, Wardhana DW, Panjaitan C. Penetrating neck injury involving wooden foreign bodies: Case report. Korean J Neurotrauma. 2023. 19: 502-8
5. Sasindran V, John MS, Augustian SM. Removal of intraorbital foreign body by transnasal endoscopic approach removal of intraorbital foreign body by transnasal endoscopic approach. Indian J Otolaryngol Head Neck Surg. 2023. 75: 1090-2
6. Siddiqui AR, Kariem K, Fayaz M, Scalia G, Chaurasia B. Transorbital penetrating intracranial injury involving bilateral frontal lobes with evisceration of right eye: A case report. Clin Case Rep. 2024. 12: e9018
7. Singh A, Sadique SI, Ghosh SN. Intraorbital foreign body with intracranial extension: A case series. Int Clin Neurosci J. 2018. 5: 43-5
8. You YY, Shi BJ, Wang XY, Chen J, Wang ZR, Wang XH. Intraorbital wooden foreign bodies: Case series and literature review. Int J Ophthalmol. 2021. 14: 1619-27