- Department of Neurosurgery, University of Caxias do Sul, Caxias do Sul, Rio Grande do Sul, Brazil,
- Laboratory of Clinical Studies and Basic Models on Spinal Cord Pathologies, University of Caxias do Sul, Caxias do Sul, Rio Grande do Sul, Brazil,
- Department of Orthopedics, Hospital Español, Mendoza, Argentina,
- Department of Oncological and Degenerative Spine Surgery, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy.
Correspondence Address:
Asdrubal Falavigna
Coordinator of Post-Graduation Program in Medicine. Departament of Neurosurgery of the University of Caxias do Sul. Rua General Arcy da Rocha Nóbrega, 401/602 CEP: 95040-290, Caxias do Sul – RS, Brazil.
DOI:10.25259/SNI_34_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Asdrubal Falavigna, Jefferson Dedea, Alfredo Guiroy, Giovanni Barbanti Brodano. Perception of complications by spine surgeons. 02-May-2020;11:88
How to cite this URL: Asdrubal Falavigna, Jefferson Dedea, Alfredo Guiroy, Giovanni Barbanti Brodano. Perception of complications by spine surgeons. 02-May-2020;11:88. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10021
Abstract
Background: The perception of major versus minor complications may vary according to surgeons, institutions, and different specialties. Here, we analyzed the geographic distribution of the different types/severities of the most frequent complications in spinal surgery, and assessed how the perception of spine surgeons about postoperative complications differed.
Methods: We performed a cross-sectional study using a questionnaire, we developed to encompass different clinical scenarios of surgeons’ perceptions of spine surgery complications. The survey involved the members of AOSpine Latin America (LA) (January 28, 2017–March 15, 2017). The main variables studied included: specialty, age, years of experience, country, individual surgeon’s perception of different clinical scenarios, and the surgeon’s classification of complications for each scenario (e.g., major, minor, or none). Our results from LA were then analyzed and compared to North American (NA) responses.
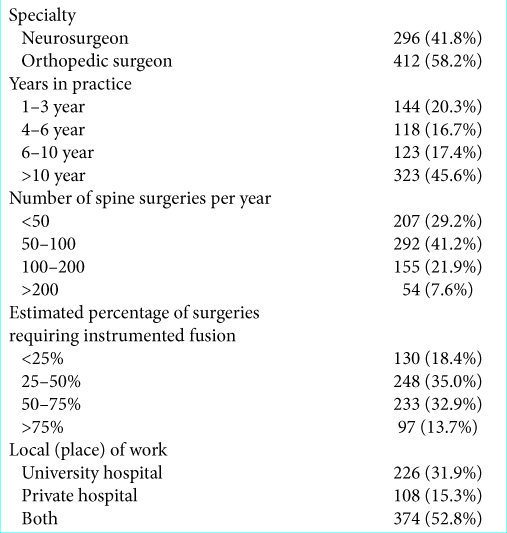
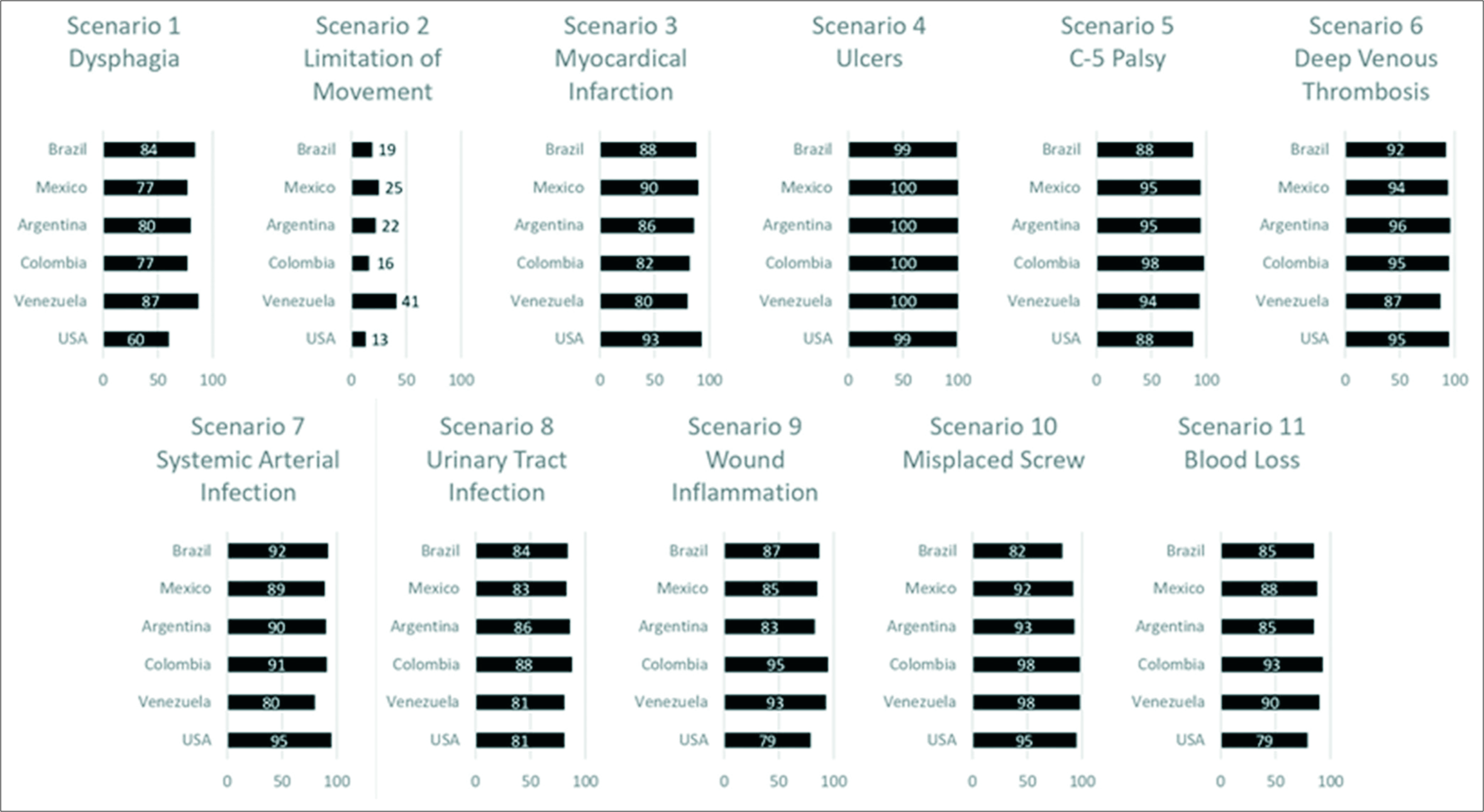
Results: Orthopedic surgeons represented about 58.2% (n = 412) of the 708 questionnaires answered. Of interest, 45.6% (n = 323) of those responding had >10 years of experience. The countries analyzed included Brazil (31.5%), Mexico (17.5%), Argentina (14.4%), Colombia (8.0%), and Venezuela (7.6%). Four of the 11 scenarios showed consensus in the results (e.g., average being over 82.5%). A tendency toward consensus was present in 45.4% of the clinical cases, while two out of 11 clinical cases did not present a consensus among surgeons. Of interest, the perception of complications was similar between cohorts (LA 85% vs. NA 80%).
Conclusion: Significant consensus in the perception of complications was observed in most of the analyzed scenarios for both LA and NA. However, within the LA data, responses to different clinical scenarios varied.
Keywords: Complications, Neurosurgeon, Orthopedist, Spine, Spine surgery
INTRODUCTION
The incidence of complications after spine surgery is an important parameter to be consider for cost benefits analyses and the decision-making process.[
Information is critical to establish criteria for reporting complications of spine surgery. However, in most of the spine centers worldwide, the perception of major versus minor complications can vary according to the surgeons, institutions, and different orthopedics and neurosurgery spinal specialties.[
MATERIALS AND METHODS
Study design
A cross-sectional study was performed using a spine surgery complications survey. The questionnaire was sent to spine surgeons who were members of AOSpine LA.
Spine surgery complications questionnaire
The questionnaire was sent to members of AOSpine LA (January 28, 2017–March 15, 2017). The e-mail contained a questionnaire translated from English to the Portuguese and Spanish (e.g., Lebude et al.).[
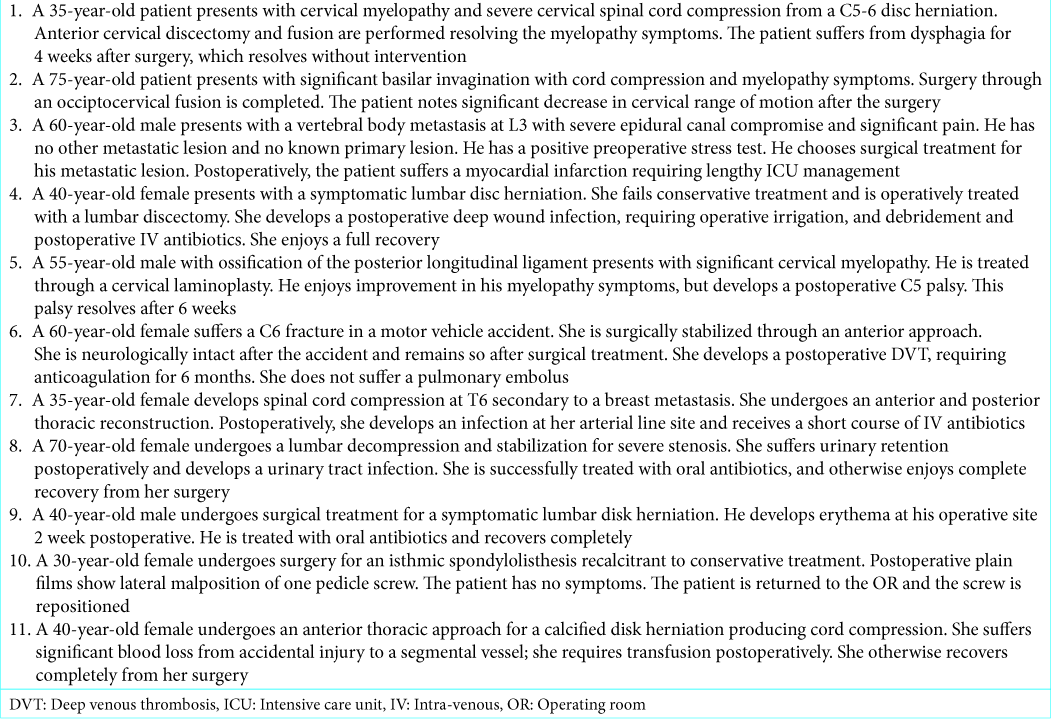
It included 17 questions; six related to surgeon demographics and 11 to clinical scenarios of complications adverse events after spine surgery [
Scenario of spine surgery complications
To evaluate a spine surgeon’s perception of postoperative complications, we developed a survey utilizing 11 different scenarios, grading each as major, minor, or none [
General information
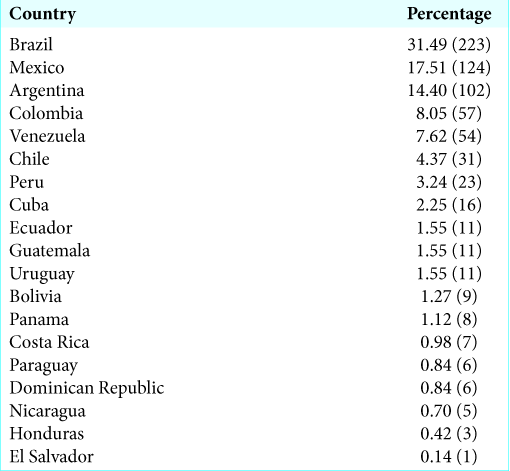
The number of participants in each country is presented in [
Statistical analysis
The probability of considering an event as a complication or not and the severity of the complication were analyzed; the odds ratio was defined in each clinical scenario. Statistical analysis was performed using the SPSS program (IBM v22.0, Chicago, IL). Categorical data were presented as counts and percentages and compared using the Chi-squared test. Proportion pairwise comparisons were conducted among groups using Bonferroni post hoc corrections. The significance level was set at P < 0.05. All data have been kept confidential.
RESULTS
Scenario of spine surgery complications
Those responding the LA questionnaire in descending order included Brazil (n = 223), Mexico (n = 124), and Argentina (n = 102). Fewer responded from Colombia (n = 57) and Venezuela (n = 54) (e.g. the countries showing more than 50 respondents vs. the NA study; n = 229) [
Scenarios with established consensus (>80%), tendency toward consensus (60–80%) and without established consensus (<60%)
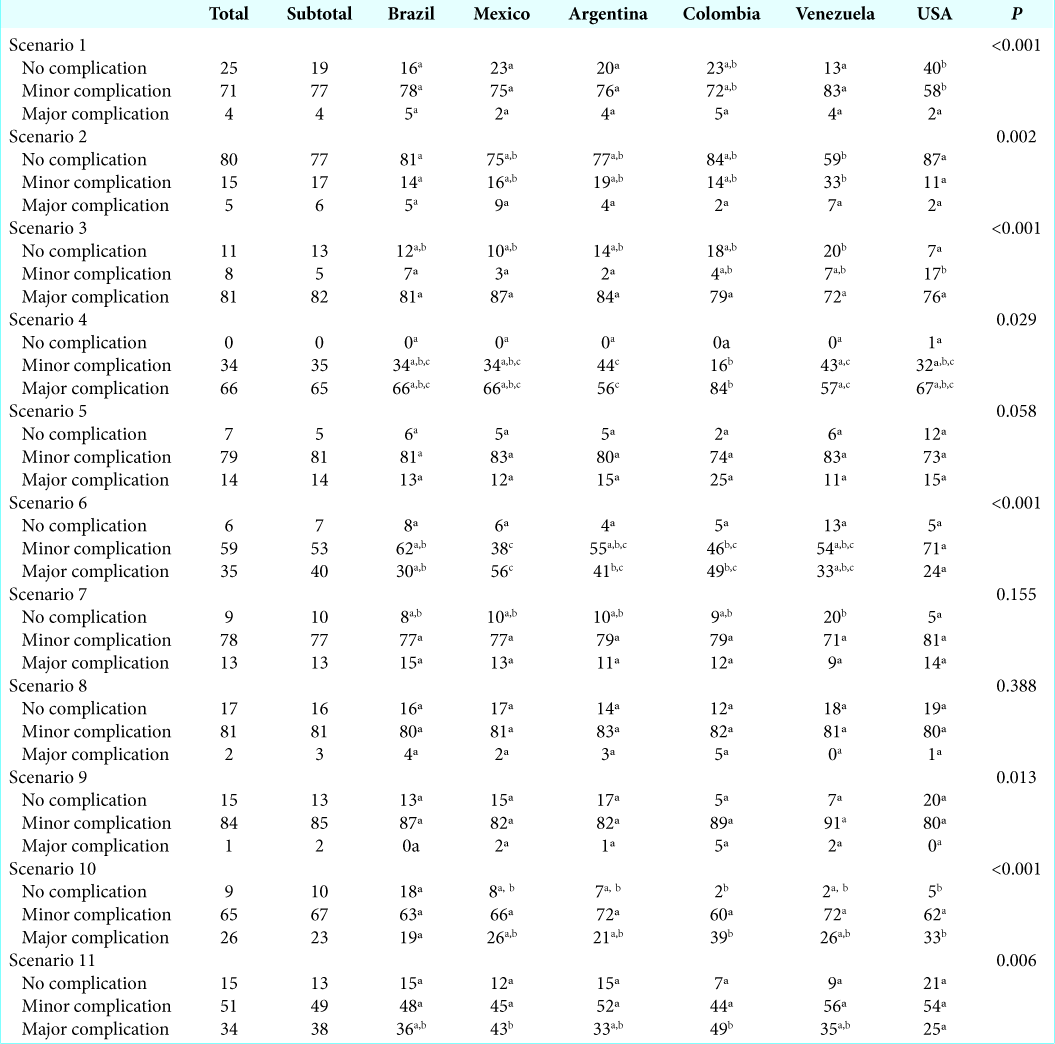
Clinical scenarios 3, 5, 8, and 9 showed a general consensus in the responses (e.g., superior to 82%) [
Comparisons of responses between LA and NA
Among the analyzed LA and NA groups, the perception of complications was similar (e.g. LA 85% and NA 80%). However, the forms of classification into major, minor, or noncomplication categories were not well defined.
In scenario 1, 77% of LA versus 58% of NA surgeons defined dysphagia as a minor complication (consensus). In scenario 3, myocardial infarction was considered a major complication for 76% for NA versus 82% of LA surgeons (consensus). However, there was no consensus for scenario 6 deep venous thrombosis (DVT); 71% from NA versus 53% of surgeons from LA classified it as a minor complication.
DISCUSSION
In the present study, we sought to understand how the spine surgeons identify and classify postoperative complications. In general, spine surgeons from LA and NA had the perception that complications were present in 82.3%, LA 85.3%, and NA 79.7%, of the clinical scenarios with 81.8% of consensus between the regions.
Complications in spinal surgery have a great impact on patient outcome and health-care costs, which increase exponentially according to severity.[
The classification of major, minor, or no complications usually is performed by the knowledge and perception of the spine surgeon.
Based on the current literature data, Lebude et al.[
Major complication
It is defined as a severe postoperative adverse event that produces permanent damaging effect or requires surgical reintervention. These adverse events occur within 30 days of surgery, having a specific connection with the surgical procedure.
Minor complication
A postoperative adverse event that produces only a transient detrimental effect, including adverse medical events in the perioperative period.
Consensus or not between NA and LA
The presence of a consensus of complications among the LA and NA cohorts was presented in 8 (72.7%) of the 11 clinical scenarios [
NA and LA did not perceive the presence of complications in clinical scenario 2 that discusses the limitation of movement after occipitocervical fusion. It was considered that the limitation of movement is expected after this type of procedure.
Among the scenarios that presented divergence among the cohorts, are scenario 1, which evaluated the dysphagia in the postoperative period. Dysphagia after anterior cervical approach can be expected in the 1st week due to the retraction of the larynx and adjacent organs during surgery.[
DVT is described as a severe postoperative complication, and the use of platelet antiaggregants and anticoagulants is aimed at decreasing the number of DVT events. Lack of movement for long periods is one of the main factors for the development of DVT in patients who need to undergo spinal surgery. Thus, it is necessary to use medications and monitoring to avoid the present adverse event.[
Although there was divergence between LA and NA cohorts in the clinical scenarios presented, responses were similar in 8 of 11 cases. However, the way both regions perceive and classify complications varies according to the individual analysis and judgment of each spine surgeon.
Chen et al.[
The study by Chen et al.[
One limitation of the study is that there was a small percentage of respondents (708 out of 1445 or 48.9%). Those who did not respond could have been either more or less knowledgeable. Nevertheless, 708 is still a large number of respondents and enough to show that surgeons’ perception regarding definition of complication after spine surgery is woefully lacking.
The better capture and perception of complications in spine surgery may lead to improvements in medical services and management strategies in the postoperative period. Studies are necessary to establish an understanding of perception to improve the management strategies and guide future research. To do that, we are currently gathering similar data regarding surgeons in other regions of the world. Our findings strongly highlight the importance of defining complications and have a similar classification.
CONCLUSION
A significant consensus was observed in the perception of the presence of complications in most of the scenarios analyzed but not for classification in major and minor complications.
Declaration of patient consent
Patients consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank AO Spine LA for survey distribution.
References
1. Akins PT, Harris J, Alvarez JL, Chen Y, Paxton EW, Bernbeck J. Risk factors associated with 30-day readmissions after instrumented spine surgery in 14,939 patients: 30-day readmissions after instrumented spine surgery. Spine (Phila Pa 1976). 2015. 40: 1022-32
2. Bekelis K, Desai A, Bakhoum SF, Missios S. A predictive model of complications after spine surgery: The national surgical quality improvement program (NSQIP) 2005-2010. Spine J. 2014. 14: 1247-55
3. Berven SH, Hohenstein NA, Savage JW, Tribus CB. Does the outcome of adult deformity surgery justify the complications in elderly (above 70 y of age) patients?. J Spinal Disord Tech. 2015. 28: 271-4
4. Chen BP, Garland K, Roffey DM, Poitras S, Dervin G, Lapner P. Can surgeons adequately capture adverse events using the spinal adverse events severity system (SAVES) and OrthoSAVES?. Clin Orthop Relat Res. 2017. 475: 253-60
5. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. 240: 205-13
6. Goz V, Weinreb JH, McCarthy I, Schwab F, Lafage V, Errico TJ. Perioperative complications and mortality after spinal fusions: Analysis of trends and risk factors. Spine (Phila Pa 1976). 2013. 38: 1970-6
7. Joaquim AF, Murar J, Savage JW, Patel AA. Dysphagia after anterior cervical spine surgery: A systematic review of potential preventative measures. Spine J. 2014. 14: 2246-60
8. Lebude B, Yadla S, Albert T, Anderson DG, Harrop JS, Hilibrand A. Defining “complications” in spine surgery: Neurosurgery and orthopedic spine surgeons’ survey. J Spinal Disord Tech. 2010. 23: 493-500
9. Lee MJ, Konodi MA, Cizik AM, Weinreich MA, Bransford RJ, Bellabarba C. Risk factors for medical complication after cervical spine surgery: A multivariate analysis of 582 patients. Spine (Phila Pa 1976). 2013. 38: 223-8
10. Yeramaneni S, Robinson C, Hostin R. Impact of spine surgery complications on costs associated with management of adult spinal deformity. Curr Rev Musculoskelet Med. 2016. 9: 327-32