- Department of Orthopedic Surgery, Joint Reconstruction Research Center, Tehran University of Medical Sciences,
- Spine Center of Excellence, Yas Hospital, Tehran University of Medical Sciences,
- Sports Medicine Research Center, Neuroscience Institute, Tehran University of Medical Sciences,
- Department of Neurosurgery, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran.
Correspondence Address:
Mohsen Rostami, Department of Neurosurgery, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran.
DOI:10.25259/SNI_616_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammad Zarei1, Mersad Moosavi2, Sajjad Saghebdoust3, Milad Shafizadeh2, Mohsen Rostami2,4. Percutaneous iliosacral screw insertion with only outlet and inlet fluoroscopic view for unstable pelvic ring injuries: Clinical and radiological outcomes. 30-Sep-2022;13:455
How to cite this URL: Mohammad Zarei1, Mersad Moosavi2, Sajjad Saghebdoust3, Milad Shafizadeh2, Mohsen Rostami2,4. Percutaneous iliosacral screw insertion with only outlet and inlet fluoroscopic view for unstable pelvic ring injuries: Clinical and radiological outcomes. 30-Sep-2022;13:455. Available from: https://surgicalneurologyint.com/surgicalint-articles/11894/
Abstract
Background: Percutaneous iliosacral screw fixation in posterior pelvic ring fractures is challenging and commonly performed under fluoroscopy or navigation techniques. This study aimed to assess the safety and efficacy of percutaneous iliosacral screw implantation under fluoroscopy guidance with only inlet and outlet views.
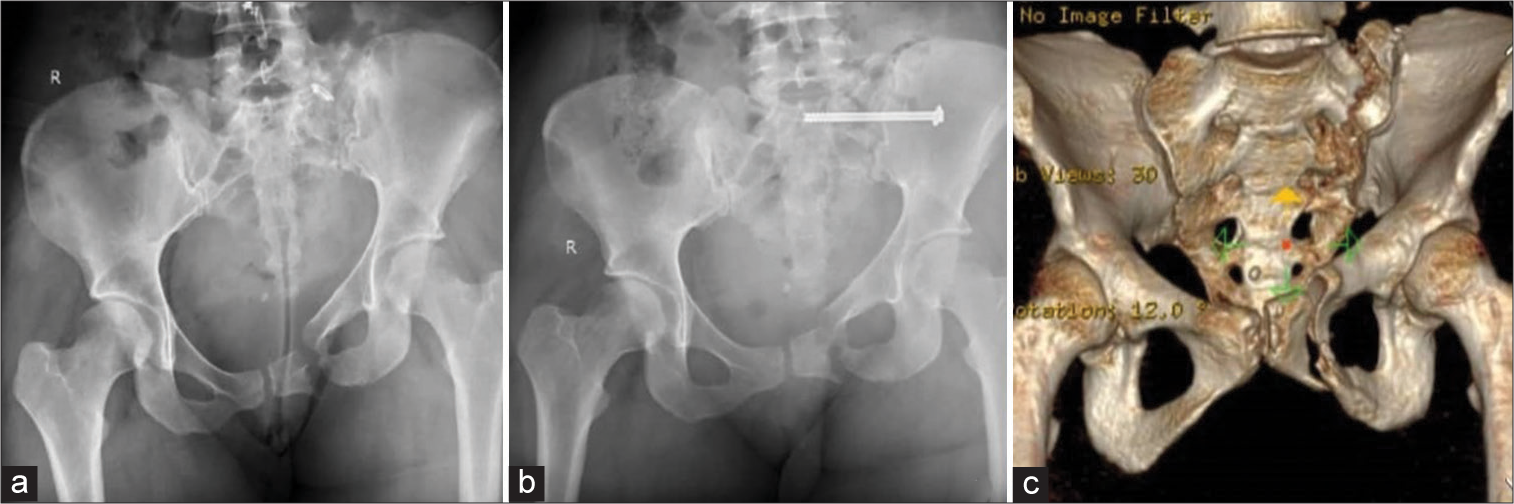
Methods: This retrospective study included 58 consecutive unstable posterior pelvic injury patients (36 sacral fractures and 22 sacroiliac joint disruptions) treated with percutaneous iliosacral screws between January 2015 and November 2019. Acceptable inlet radiographs show the anterior cortex of the S1 body superimposed on the S2 body. Acceptable outlet radiographs show the superior pubic symphysis at the level of the S2 foramen and visualize the S1 and S2 sacral foramina. In our technique, the screw was inserted at the inferior half of the outlet view and the posterior half of the inlet view. The time needed for screw insertion and the radiation exposure time was recorded. Intra and postoperative complications were documented. Postoperative computed tomography (CT) scans assessed screw position.
Results: In total, 69 iliosacral screws were inserted in 58 patients. In postoperative CT scans, the screw position was assessed, 89.8% were in a secure position, and 10.2% had malposition. The mean operation time per screw was 21.18 min and the mean fluoroscopy time per screw was 112 s. There was no evidence of wound infection or iatrogenic neurovascular injury. No reoperation was performed.
Conclusion: Percutaneous iliosacral screws can be placed using the only outlet and inlet fluoroscopic views with comparable radiological and clinical outcomes to the conventional method.
Keywords: Inlet view, Outlet view, Pelvic ring fracture, Percutaneous iliosacral screw, Sacral fracture
INTRODUCTION
Unstable pelvic fractures account for 40% of all pelvic fractures[
Appropriate fluoroscopic visualization of the posterior pelvic ring is essential for the safe percutaneous iliosacral screw placement.[
The fluoroscopy technique’s significant disadvantages are radiation exposure to the surgical team and patient[
MATERIALS AND METHODS
Reviewing our database, patients were included in the study if they were older than 18 years and had undergone percutaneous iliosacral screws fixation due to unstable pelvic ring traumatic fracture between January 2015 and November 2019. Pelvic ring instability was defined as at least one of the following conditions: (1) A break in the anterior and posterior pelvic ring; (2) an extremely misshapen pelvis; (3) a displaced posterior ring injury; and (4) a displaced triradiate fracture. Data of the subjects with any of the following conditions were excluded from the study: (1) Lumbosacral dysplasia and sacral dysmorphism, (2) history of the pelvic girdle neoplasm, (3) history of seronegative arthropathies, and (4) the previous sacral fracture or lumbosacral dislocation.
The patients’ demographic information, such as gender and age, was gathered from the medical records, and postoperative images were reviewed. After explaining the study goals and receiving written informed consent, a postoperative computed tomography (CT) scan was performed for each subject to evaluate the intraosseous screw implantation and reduction of the SI joint and sacral fracture. Pre and postoperative neurological examinations of muscles and dermatomes served by the L4, L5, and S1 roots were obtained retrospectively. The amount of time spent exposed to radiation (fluoroscopy time) per screw and operative time per screw was recorded. All screw misplacements that were outside of the favorable anatomical safe zone were accurately measured and recorded. Early outcome factors were operative and fluoroscopy times, intraoperative loss of blood, and length of hospital stay. Late outcome factors were determined as SI joint pain and radiological outcome. A visual analog scale (VAS) was utilized to measure the pain intensity.
Surgical technique
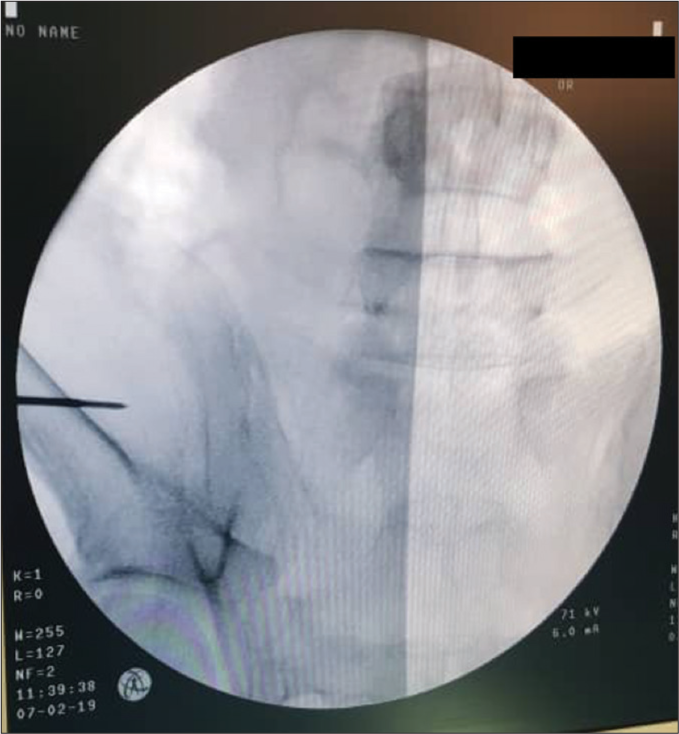
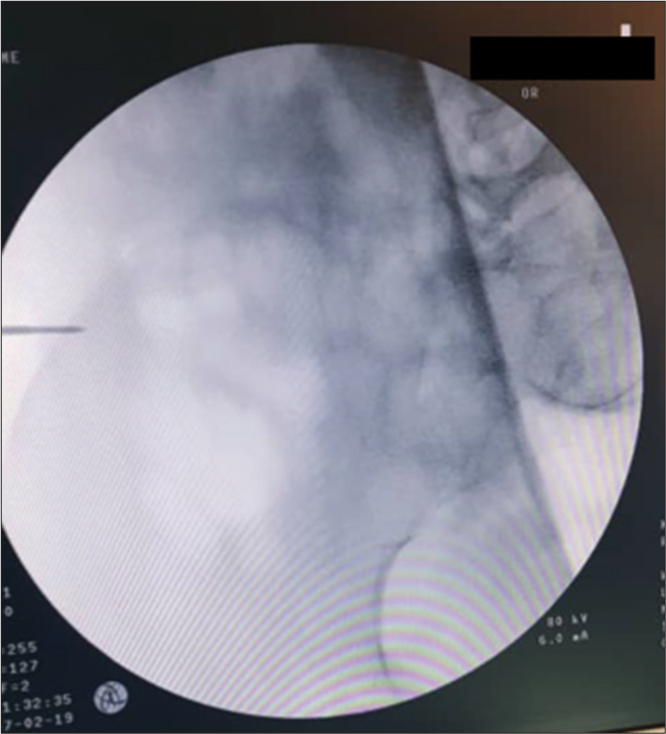
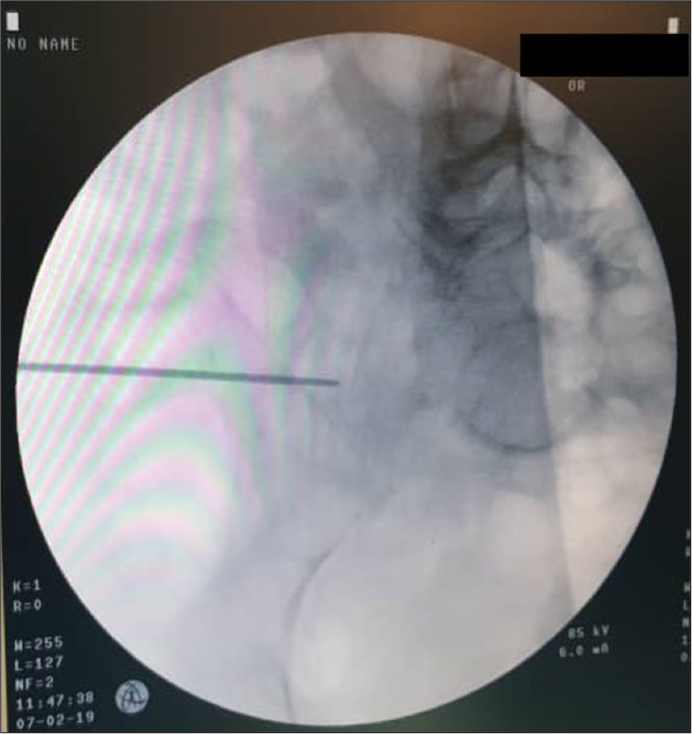
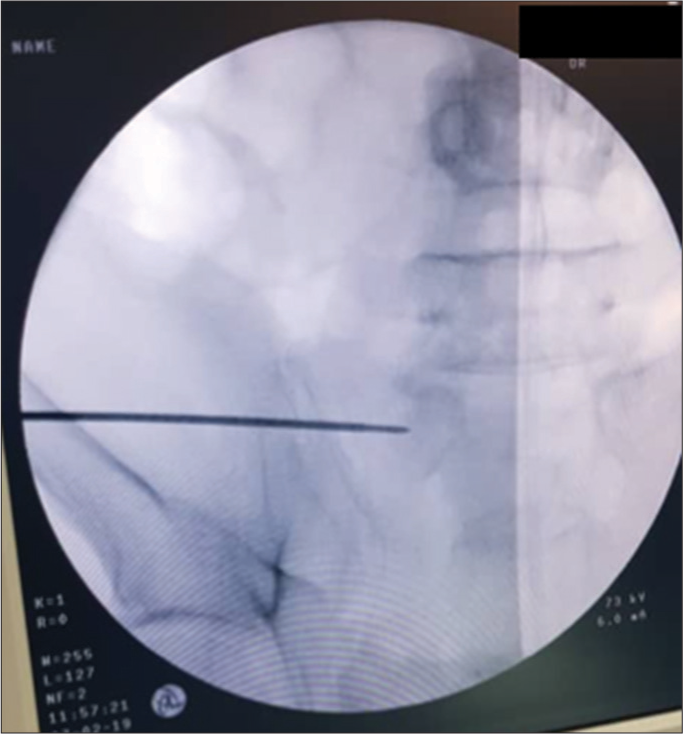
Patients were positioned on a transparent table in a supine position,[
The entire process of insertion of the screw was performed under fluoroscopic control using one C-Arm.[
In contrast to SI joint dislocation, screw fixation of a comminuted Zone II sacral fracture does not require compression of the fragments, leading to the nerve roots injury.[
Assessments
The primary outcome of interest in this retrospective study was the accurate positioning of iliosacral screws, which were defined as screws being within the sacrum’s cortical margins with no bony perforation or neural foramen hit. The final screw position was measured on a postoperative CT.[
Statistical analysis
All analyses were carried out using SPSS, version 25. P < 0.05 was considered significant.
RESULTS
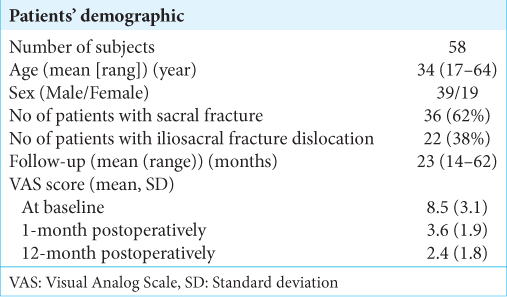
Fifty-eight patients underwent fixation with percutaneous iliosacral screw for unstable pelvic injuries between January 2015 and November 2019. This study was conducted on 39 male and 19 female patients with ages ranging from 17 to 64 years (mean = 34). Of the subjects, 22 had iliosacral fracture-dislocations and 36 patients had sacral fractures [
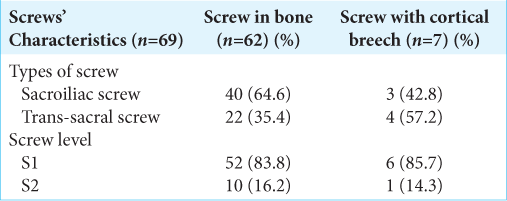
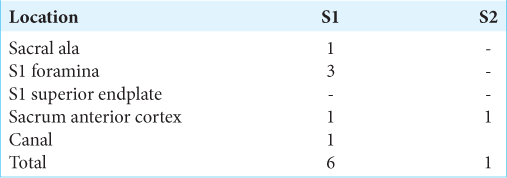
Of 69 screws, 62 (89.8%) were in the secure position [
In total, 43 (62.3%) SI screws and 26 (37.7%) trans-sacral screws were placed [
Neurological loss, pain intensity, and revision rate were considered secondary outcome measures, including implant failure or breakage and non-union. Neurologic pain occurred in two patients. Severe pain in one of the patients was due to an S1 neural foramen hit, and another patient had neurologic pain while the iliosacral screw was in the proper place. Both of the patients were treated conservatively and no reoperation was performed. We failed to find any intraoperative difficulties or postoperative neurological deficits among the individuals.
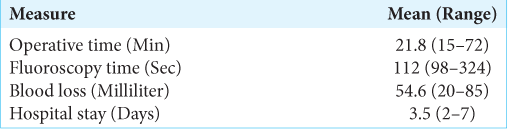
The average operational time per screw was 21.18 min (15–72 min) and the mean fluoroscopic time included management of the patient’s position on the operating table before the surgery, reduction maneuvers, capturing images for screw placement, and documenting final screw position during the operation was 112 s per screw (range 98–324). The average blood loss during the operation was 54.6 ml and the patients’ mean length of stay in the hospital was 3.5 days [
DISCUSSION
Percutaneous iliosacral screw placement is a challenging and technically demanding surgery, mostly due to highly varied pelvic anatomy and screw trajectories.[
The previous studies compared the screw malposition rate concerning the application of fluoroscopy or computer navigation. Zwingmann et al.[
Correct inlet and outlet views using the intraoperative C-arm necessitate various angles because of variations in the sacral bone anatomy.[
The amount of radiation exposure and operative time in iliosacral screw placement under fluoroscopy guidance is associated with the surgical and fluoroscopic techniques. Appropriate protection use, sparse use of fluoroscopy, systemic approach to screw insertion, preoperative planning, and good communication with the X-ray technician will decrease fluoroscopy shots and operating time.[
The average preoperative VAS score was 8.5, which decreased to 3.6 and 2.4 at 1- and 12-month postoperative, respectively. Furthermore, no case of wound infection was found in our series. These results are consistent with the previous studies.[
Retrospective design and short follow-up might be considered the major limitations of our study. Furthermore, the small sample size of the study and performing the procedures in two different operating rooms and with two different C-Arms might decrease the accuracy of the results. We suggest feasibility studies and measurement of outcomes for future studies while the procedures are done by residents and junior surgeons. Comparison of the outcomes while doing the operation using only one C-Arm or 2 C-Arms should also be addressed in the future studies.
CONCLUSION
In summary, percutaneous iliosacral screw placement with only outlet and inlet fluoroscopic view is a safe, easily obtained, reproducible, and anatomically based technique with comparable clinical and radiological results to other techniques with shorter operating time and lower radiation exposure than the conventional method. Clear C-arm images and precise evaluation of the images are crucial to avoid possible complications such as malposition screw and neurovascular injuries.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent .
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Briem D, Windolf J, Rueger JM. Percutaneous, 2D-fluoroscopic navigated iliosacral screw placement in the supine position: Technique, possibilities, and limits. Unfallchirurg. 2007. 110: 393-401
2. Collinge C, Coons D, Tornetta P, Aschenbrenner J. Standard multiplanar fluoroscopy versus a fluoroscopically based navigation system for the percutaneous insertion of iliosacral screws: A cadaver model. J Orthop Trauma. 2005. 19: 254-8
3. Ebraheim NA, Haman SP, Xu R, Stanescu S, Yeasting RA. The lumbosacral nerves in relation to dorsal S1 screw placement and their locations on plain radiographs. Orthopedics. 2000. 23: 245-7
4. Ebraheim NA, Xu R, Biyani A, Nadaud MC. Morphologic considerations of the first sacral pedicle for iliosacral screw placement. Spine (Phila Pa 1976). 1997. 22: 841-6
5. Gänsslen A, Hüfner T, Krettek C. Percutaneous iliosacral screw fixation of unstable pelvic injuries by conventional fluoroscopy. Oper Orthop Traumatol. 2006. 18: 225-44
6. Giannoudis PV, Papadokostakis G, Alpantaki K, Kontakis G, Chalidis B. Is the lateral sacral fluoroscopic view essential for accurate percutaneous sacroiliac screw insertion? An experimental study. Injury. 2008. 39: 875-80
7. Gras F, Marintschev I, Wilharm A, Klos K, Mückley T, Hofmann GO. 2D-fluoroscopic navigated percutaneous screw fixation of pelvic ring injuries a case series. BMC Musculoskelet Disord. 2010. 11: 153
8. Grossterlinden L, Rueger J, Catala-Lehnen P, Rupprecht M, Lehmann W, Rücker A. Factors influencing the accuracy of iliosacral screw placement in trauma patients. Int Orthop. 2011. 35: 1391-6
9. Gusic N, Grgorinic I, Fedel I, Lemac D, Bukvic N, Gusic M. Fluoroscopic iliosacral screw placement made safe. Injury. 2017. 48: S70-2
10. Herman A, Keener E, Dubose C, Lowe JA. Simple mathematical model of sacroiliac screws safe-zone-Easy to implement by pelvic inlet and outlet views. J Orthop Res. 2017. 35: 1478-84
11. Iorio JA, Jakoi AM, Rehman S. Percutaneous Sacroiliac Screw Fixation of the Posterior Pelvic Ring. Orthop Clin North Am. 2015. 46: 511-21
12. Kim JW, Kim JJ. Radiation exposure to the orthopaedic surgeon during fracture surgery. J Korean Orthop Assoc. 2010. 45: 107-13
13. Lee JJ, Rosenbaum SL, Martusiewicz A, Holcombe SA, Wang SC, Goulet JA. Transsacral screw safe zone size by sacral segmentation variations. J Orthop Res. 2015. 33: 277-82
14. Lee MJ, Wright A, Cline M, Mazza MB, Alves T, Chong S. Pelvic fractures and associated genitourinary and vascular injuries: A multisystem review of pelvic trauma. AJR Am J Roentgenol. 2019. 213: 1297-306
15. Mason LW, Chopra I, Mohanty K. The percutaneous stabilisation of the sacroiliac joint with hollow modular anchorage screws: A prospective outcome study. Eur Spine J. 2013. 22: 2325-31
16. Miller AN, Routt ML. Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg. 2012. 20: 8-16
17. Moed BR, Geer BL. S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: A report of 49 cases. J Orthop Trauma. 2006. 20: 378-83
18. Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. Percutaneous iliosacral screw fixation in S1 and S2 for posterior pelvic ring injuries: Technique and perioperative complications. Arch Orthop Trauma Surg. 2011. 131: 809-13
19. Ozmeric A, Yucens M, Gultaç E, Açar HI, Aydogan NH, Gül D. Are two different projections of the inlet view necessary for the percutaneous placement of iliosacral screws?. Bone Joint J. 2015. 97B: 705-10
20. Pekmezci M, Rotter P, Toogood P, Morshed S, Kandemir U. Reexamination of pelvic inlet and outlet images using 3-dimensional computed tomography reconstructions. J Orthop Trauma. 2014. 28: 324-9
21. Peng KT, Huang KC, Chen MC, Li YY, Hsu RW. Percutaneous placement of iliosacral screws for unstable pelvic ring injuries: Comparison between one and two C-arm fluoroscopic techniques. J Trauma. 2006. 60: 602-8
22. Ricci WM, Mamczak C, Tynan M, Streubel P, Gardner M. Pelvic inlet and outlet radiographs redefined. J Bone Joint Surg Am. 2010. 92: 1947-53
23. Routt ML, Kregor PJ, Simonian PT, Mayo KA. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995. 9: 207-14
24. Routt ML, Simonian PT. Closed reduction and percutaneous skeletal fixation of sacral fractures. Clin Orthop Relat Res. 1996. 329: 121-8
25. Routt ML, Simonian PT, Mills WJ. Iliosacral screw fixation: Early complications of the percutaneous technique. J Orthop Trauma. 1997. 11: 584-9
26. Schweitzer D, Zylberberg A, Córdova M, Gonzalez J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury. 2008. 39: 869-74
27. Shuler TE, Boone DC, Gruen GS, Peitzman AB. Percutaneous iliosacral screw fixation: Early treatment for unstable posterior pelvic ring disruptions. J Trauma. 1995. 38: 453-8
28. Tidwell J, Cho R, Reid JS, Boateng H, Copeland C, Sirlin E. Percutaneous sacroiliac screw technique. J Orthop Trauma. 2016. 30: S19-20
29. Tonetti J, van Overschelde J, Sadok B, Vouaillat H, Eid A. Percutaneous ilio-sacral screw insertion, fluoroscopic techniques. Orthop Traumatol Surg Res. 2013. 99: 965-72
30. Verbeek J, Hermans E, van Vugt A, Frölke JP. Correct positioning of percutaneous iliosacral screws with computer-navigated versus fluoroscopically guided surgery in traumatic pelvic ring fractures. J Orthop Trauma. 2016. 30: 331-5
31. Yin Y, Hou Z, Zhang R, Jin L, Chen W, Zhang Y. Percutaneous placement of iliosacral screws under the guidance of axial view projection of the S1 pedicle: A case series. Sci Rep. 2017. 7: 7925
32. Zhang J, Hamilton R, Li M, Ebraheim NA, He X, Liu J. Evaluation of partial cut-out of sacroiliac screws from the sacral ala slope via pelvic inlet and outlet view. Spine (Phila Pa 1976). 2015. 40: E1264-8
33. Ziran BH, Wasan AD, Marks DM, Olson SA, Chapman MW. Fluoroscopic imaging guides of the posterior pelvis pertaining to iliosacral screw placement. J Trauma. 2007. 62: 347-56
34. Zwingmann J, Hauschild O, Bode G, Südkamp NP, Schmal H. Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2013. 133: 1257-65
35. Zwingmann J, Konrad G, Kotter E, Südkamp NP, Oberst M. Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res. 2009. 467: 1833-8
36. Zwingmann J, Konrad G, Mehlhorn AT, Südkamp NP, Oberst M. Percutaneous iliosacral screw insertion: Malpositioning and revision rate of screws with regards to application technique (navigated vs. Conventional). J Trauma. 2010. 69: 1501-6
37. Zwingmann J, Südkamp NP, König B, Culemann U, Pohlemann T, Aghayev E. Intra and postoperative complications of navigated and conventional techniques in percutaneous iliosacral screw fixation after pelvic fractures: Results from the German Pelvic Trauma Registry. Injury. 2013. 44: 1765-72