- Department of Surgery, Santa Casa de Sao Paulo School of Medical Sciences, São Paulo, Brazil.
Correspondence Address:
Guilherme Brasileiro de Aguiar, Department of Surgery, Santa Casa de Sao Paulo School of Medical Sciences, São Paulo, Brazil.
DOI:10.25259/SNI_588_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Andrew Vinícius de Souza Batista, Guilherme Brasileiro de Aguiar, Priscilla Bennett, José Carlos Esteves Veiga. Periodontoid pseudotumoral lesions. 09-Aug-2021;12:403
How to cite this URL: Andrew Vinícius de Souza Batista, Guilherme Brasileiro de Aguiar, Priscilla Bennett, José Carlos Esteves Veiga. Periodontoid pseudotumoral lesions. 09-Aug-2021;12:403. Available from: https://surgicalneurologyint.com/surgicalint-articles/11025/
Abstract
Background: Periodontoid pseudotumoral lesions (PPL) are an uncommon cause of cervical pain and myelopathy. In addition, they may be associated with atlantoaxial instability (AAI).
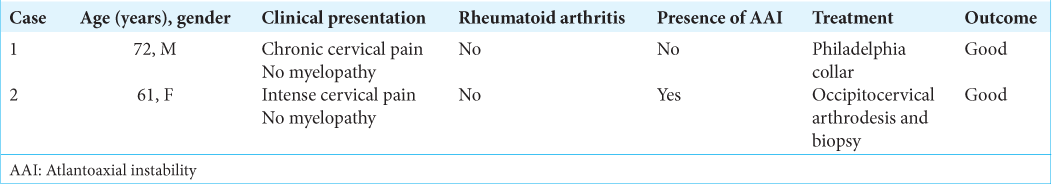
Case Description: Two patients over 60 years of age presented with neck pain alone. Their MR scans showed expansive lesions involving the odontoid process. One patient with AAI required an occipitocervical arthrodesis, while the other patient without instability was managed with an external orthosis (Philadelphia collar). Both of them experienced full resolution of pain and remained neurologically intact an average 36 months later (range 24–48).
Conclusion: Here, we discussed the clinical, MR, and non-surgical (without AAI) versus surgical management (with AAI) for different types of PPL.
Keywords: Atlanto-axial joint, Magnetic resonance imaging, Odontoid process, Skull base, Spinal cord diseases
INTRODUCTION
In this study, we present the clinical, MR appearance, non-surgical, and surgical management for two cases of periodontoid pseudotumoral lesions (PPL), and selectively reviewed the appropriate literature.
CASE DESCRIPTION
Case 1: Non-surgical management of PPL
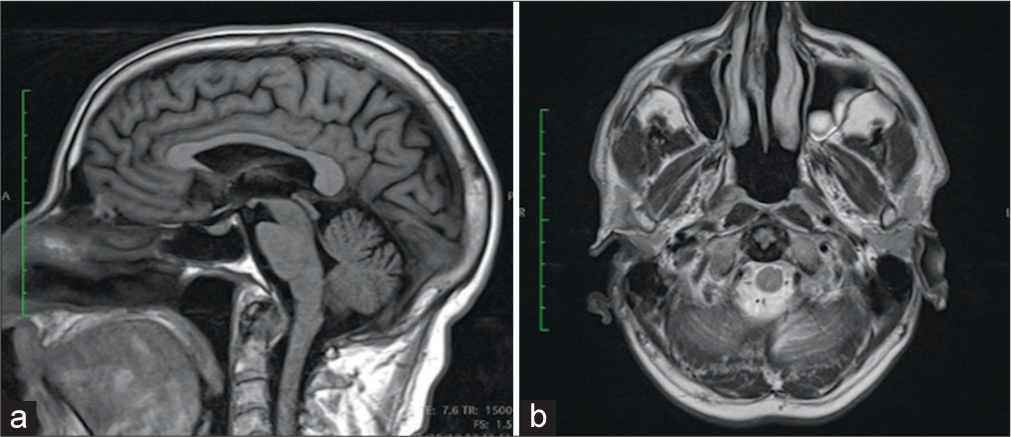
A 72-year-old male presented with neck pain alone, no neurological deficit, and a cervical MR that showed an expansive lesion posterior to the odontoid process [
Case 2: Surgical management of PPL
A 61-year-old female developed the rapid onset cervical pain exacerbated with cervical rotation but no neurological deficit.
Here, the cervical MRI revealed an intense inflammatory reaction involving the atlantoaxial joint (i.e. hyperintense T2 signal in anomalous tissue around the axis dens, with widening of the atlantodental interval) [
Figure 2:
Sagittal sections from preoperative magnetic resonance imaging (a-c) indicating tissue formations that suggest an expansive process at the atlantodental joint, with low signal at T1 (a), intense enhancement after contrast injection (b) and heterogeneous signal at T2 (c). In (d), it is presented an axial section of a computed tomography image of the cervical spine obtained at the immediate postoperative period of occipitocervical arthrodesis; the arrow points to the calcification halo around the axon odontoid process. In (e) and (f), it is presented the final result of the occipitocervical arthrodesis.
DISCUSSION
Retro-odontoid pseudotumor (ROP)
ROP tumor is most often attributed to rheumatoid arthritis,[
The first patient we presented had a Tanaka’s type 2 ROP lesion without AAI.
Crowned dens syndrome (CDS)
In CDS, calcium pyrophosphate crystal deposition leads to expansion of the soft tissues and local inflammatory reaction (i.e. similar to pseudogout). CT is the most useful method for diagnosis.[
MR imaging of PPL and documentation of three types of lesions
Yonezawa et al. classified retro-odontoid lesions in three types based on MR signals: type I (inflammatory, typical of pannus) – hyposignal in T1 and hypersignal in T2; type II (fibrous) - hyposignal in T1 and T2; and type III (mixed) – heterogeneous signal in T2.[
Non-surgical and surgical management of PPL
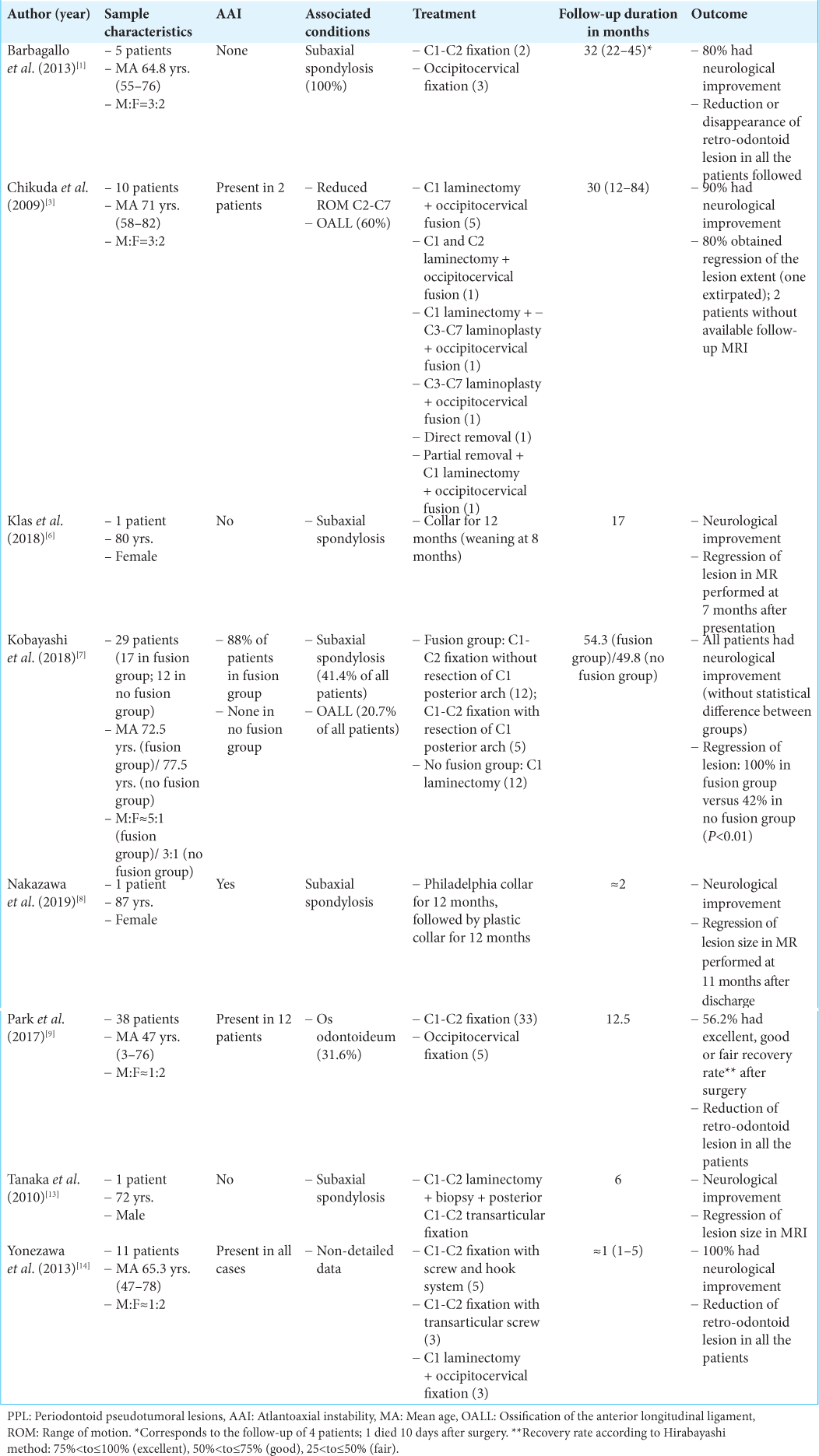
The ideal approach to cases of PPL may be non-surgical or surgical [
Since those without instability do not typically warrant fusions,[
For those with AAI, fusions are usually warranted. Atlantoaxial and occipitocervical fixations are associated with good rates of recovery and reduction or disappearance of PPL.[
Here, case 1 of ROP was successfully managed with cervical collar immobilization for an average of 18 months.[
CONCLUSION
The best treatment for PPL requires MR evaluation and X-ray assessment of AAI; the latter may warrant fusion.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barbagallo GM, Certo F, Visocchi M, Palmucci S, Sciacca G, Albanese V. Disappearance of degenerative, non-inflammatory, retro-odontoid pseudotumor following posterior C1-C2 fixation: Case series and review of the literature. Eur Spine J. 2013. 22: S879-88
2. Batista AV, Aguiar GB, Daniel JW, Veiga JC. Retro-odontoid pseudotumor: A poorly recognized alteration of the craniocervical junction. Rev Assoc Med Bras. 2020. 66: 507-11
3. Chikuda H, Seichi A, Takeshita K, Shoda N, Ono T, Matsudaira K. Radiographic analysis of the cervical spine in patients with retro-odontoid pseudotumors. Spine (Phila Pa 1976). 2009. 34: E110-4
4. Goto S, Umehara J, Aizawa T, Kokubun S. Crowned dens syndrome. J Bone Joint Surg Am. 2007. 89: 2732-6
5. Jun BY, Yoon KJ, Crockard A. Retro-odontoid pseudotumor in diffuse idiopathic skeletal hyperostosis. Spine (Phila Pa 1976). 2002. 27: E266-70
6. Klas PG, Wilson J, Cusimano MD. Regression of degenerative retro-odontoid pseudotumor treated in a collar. Can J Neurol Sci. 2018. 45: 599-600
7. Kobayashi K, Imagama S, Ando K, Nishida Y, Ishiguro N. Postoperative regression of retro-odontoid pseudotumors treated with and without fusion. Eur Spine J. 2018. 27: 3105-12
8. Nakazawa T, Inoue G, Imura T. Regression of retro-odontoid pseudotumor using external orthosis without atlantoaxial fusion: A case report. JBJS Case Connect. 2019. 9: e0329
9. Park JH, Lee E, Lee JW, Kang Y, Ahn JM, Yeom JS. Postoperative regression of retro-odontoid pseudotumor after atlantoaxial posterior fixation: 11 years of experience in patients with atlantoaxial instability. Spine (Phila Pa 1976). 2017. 42: 1763-71
10. Robles LA, Mundis GM. Retro-odontoid pseudotumor without radiologic atlantoaxial instability: A systematic review. World Neurosurg. 2019. 121: 100-10
11. Ryu JI, Han MH, Cheong JH, Kim JM, Kim CH, Chun H. The effects of clinical factors and retro-odontoid soft tissue thickness on atlantoaxial instability in patients with rheumatoid arthritis. World Neurosurg. 2017. 103: 364-70
12. Tajima K, Ueda T, Ueno K, Shimizu C, Yoshizawa J, Hori S. Crowned dens syndrome: Reports of six cases and review of the literature. Acute Med Surg. 2016. 3: 155-8
13. Tanaka S, Nakada M, Hayashi Y, Mohri M, Uchiyama N, Hamada J. Retro-odontoid pseudotumor without atlantoaxial subluxation. J Clin Neurosci. 2010. 17: 649-52
14. Yonezawa I, Okuda T, Won J, Sakoda J, Nakahara D, Nojiri H. Retrodental mass in rheumatoid arthritis. J Spinal Disord Tech. 2013. 26: E65-9