- Department of Neurosurgery, School of Medicine, State University of New York at Stony Brook, N,Y., U.S.A.
DOI:10.25259/SNI_317_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Perspective: Early diagnosis and treatment of postoperative recurrent cerebrospinal fluid fistulas/ dural tears to avoid adhesive arachnoiditis. 03-May-2021;12:208
How to cite this URL: Nancy E. Epstein. Perspective: Early diagnosis and treatment of postoperative recurrent cerebrospinal fluid fistulas/ dural tears to avoid adhesive arachnoiditis. 03-May-2021;12:208. Available from: https://surgicalneurologyint.com/surgicalint-articles/10776/
Abstract
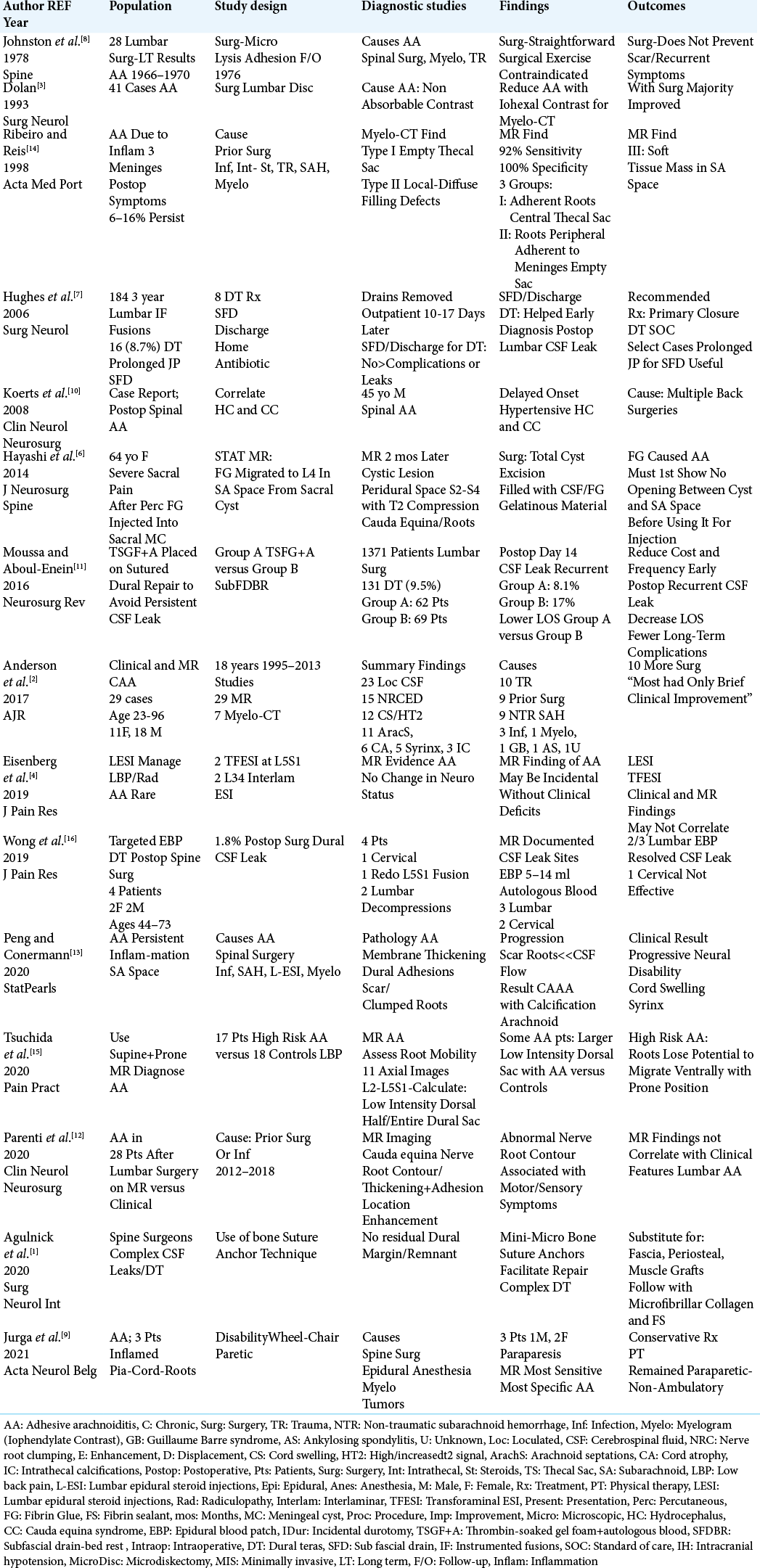
Background: Intraoperative traumatic cerebrospinal fluid (CSF) fistulas/dural tears (DT) occur in up to 8.7–9.5% of primary lumbar surgical procedures. Further, they recur secondarily in between 8.1% and 17% of cases. It is critical to diagnose and treat these recurrent lumbar DT early (i.e. within 3–4 weeks of the index surgery) to avoid the evolution of adhesive arachnoiditis (AA), and its’ permanent neurological sequelae.
Methods: Postoperative lumbar CSF fistulas/DT should be diagnosed on postoperative MR scans, and confirmed on Myelo-CT studies if needed. They should be definitively treated/occluded early on (e.g. within 3–4 postoperative weeks) to avoid the evolution of AA which can be readily diagnosed on MR studies, and corroborated, if warranted, on Myelo-CT examinations. The most prominent MR/Myelo-CT findings include; nerve roots aggregated in the central thecal sac, nerve roots peripherally scarred/adherent to the surrrounding meningeal wall (“empty thecal sac sign”), soft tissue masses in the subarachnoid space, and/or multiple loculated/scarred compartments.
Results: Percutaneous interventional procedures (i.e. epidural blood patches, injection of fibrin glue (FG)/fibrin sealants (FS)) are rarely effective for treating postoperative recurrent lumbar CSF fistulas. Rather, direct surgical occlusion is frequently warranted including the use of; an operating microscope, adequate surgical exposure, 7-0 Gore-Tex sutures, muscle/dural patch grafts or suture anchors, followed by the application of microfibrillar collagen, and fibrin sealant/glue.
Conclusion: Lumbar AA most commonly results from the early failure to diagnose and treat recurrent postoperative CSF fistulas. Since the clinical course of lumbar AA is typically one of progressive neurological deterioration, avoiding its’ initial onset is key.
Keywords: Adhesive arachnoiditis, Cerebrospinal fluid fistula, Dural tear, Lumbar surgery, MR, Myelo-CT, Neurological deficits, Postoperative recurrent, Primary, Secondary
INTRODUCTION
Lumbar spine surgery results in up to a 8.7–9.5% incidence of intraoperative cerebrospinal fluid (CSF) fisutlas/dural tears (DT) occurring during index procedures. Further, up to 8.1–17% of patients with primary lumbar DT experience recurrent postoperative CSF leaks/ DT [
MATERIALS AND METHODS
Frequency of primary and recurrent postoperative CSF fistulas/DT
The frequency of CSF fistulas/DT occurring during primary lumbar procedures ranges from 8.7% to 9.5% [
Postoperative CSF fistula/DT predominant cause of AA
AA develops secondary to an inflammatory response occurring within the 3 meningeal layers, particularly impacting the subarachnoid space [
Other etiologies of lumbar AA
Other etiologies of lumbar AA include; lumbar epidural or intrathecal particulate steroid injections, myelography (oil and water soluble contrast), trauma, infection, and subarachnoid hemorrhage amongst others [
Symptoms/signs of persistent postoperative lumbar CSF leaks/DT leading to increased neurological deficits, intracranial hypotension (IH), and AA
Major clinical disability is often associated with lumbar AA characterized on MR by; nerve root clumping, enhancement/ displacement, cord swelling/atrophy, and/or syrinx formation [
Neurodiagnostic studies for lumbar AA
MR diagnosis of lumbar AA
Ribeiro and Reis defined the 3 Types of classical MR findings for patients with lumbar AA [
Myelo-CT diagnosis of lumbar AA
Ribeiro and Reis defined the 2 Types of classical Myelo-CT findings of lumbar AA [
Both MR and Myelo-CT studies document lumbar AA in one clinical series
Anderson et al. (2017) documented chronic AA in 29 patients utilizing MR (all 29 patients), and selective Myelo-CT studies (7 patients) [
Brain MR documentation of IH in patients with untreated persistent postoperative lumbar CSF fistula/DT
Brain MR is the study of choice to document IH, particularly in patients with persistent, untreated or inadequately treated/ recurrent postoperative lumbar CSF fistulas/DT. Here, the classical Brain MR findings with/without contrast include; dural enhancement, subdural hematomas, cerebellar/ tonsillar herniation (i.e. “brain sagging”), and intracranial venous distension.
Surgical techniques for treating intraoperative and postoperative recurrent lumbar CSF fistulas/DT
Basic surgical techniques for repair of primary and/or recurrent postoperative lumbar DT
The management of initial and/or recurrent postoperative lumbar CSF fisutlas/DT includes; an operating microscope (i.e. to maximize visualization), adequate surgical exposure (i.e. to maneuver dural sutures/safely retract neural tissues), and to use of 7-0 Gore-Tex sutures (i.e. 7-0 Gore-Tex should be used due to the small size and maneuverability of the needle that is smaller than the suture thus enabling the suture itself to occlude dural holes made by the needle). For these repairs, 4-0 Nurolon should not be employed as first, the needle is too large to adequately maneuver in small spaces, and second, the suture is smaller than the needle allowing for more leakage through the dural puncture sites. More complex repairs may also warrant muscle/dural patch grafts, and/or suture anchors.[
Treating primary intraoperative lumbar DT with prolonged postoperative jackson pratt drainage
In Hughes et al. series, 16 (8.7%) of 184 patients developed intraoperative DT during index lumbar instrumented fusions; all patients underwent adequate, according to the authors, priimary dural closure [
Efficacy of managing index lumbar CSF fistulas/DT using thrombin soaked gelfoam + autologous blood (TSGF+A) versus subfascial drain + bed rest (SubFDBR)
In 131 (9.5%) of 1371 patients, Moussa et al. (2011) tested the relative efficacy of applying thrombin soaked Gelfoam plus autologous blood (TSGF+A: Group A-62 patients) versus subdural drains + bed rest (SubFDBR: Group B-69 patients) for occluding primary intraoperative lumbar CSF fistulas/ DT [
Utility of duragen/durgen plus and FS/FG for repair of lumbar CSF fisutlas/DT
Microfibrillar collagen products, including Duragen and Duragen Plus (Microfibillar Collagen, Integra LifeSciences Corporation, Plainsboro, New Jersey, USA) are excellent adjuncts to increase the strength/durability of if intraoperative CSF fistulas/DT repairs. The package insert states; “ it is a dura substitute for the repair of dura mater.” Duragen can be used as an en-lay graft. However, Duragen Plus is thicker and also suturable. With Duragen Plus you should apply circumferential 7-0 Gore-Tex sutures (i.e., or suture anchors if no dural edge is available) to secure it in place, and prevent it from migrating away from the repair site. When used appropriately, it effectively further reduces the risk of a recurrent postoperative CSF fistula/DT. When used, Duragen Plus should overlap the residual dural edges, including that of the underlying Duragen layer, by 1 cm. As noted above, it can also be placed dorsal to repairs performed with suture anchors.[
Pros and cons of FG for repair of lumbar CSF fisutlas/DT
Limited efficacy of lumbar FG percutaneous application by interventional radiology
There are various studies in which interventional radiologists utilized different FS/FG to percutaneously occlude persistent postoperative CSF fistulas/DT (e.g. reports with DuraSeal, Integra LifeSciences, and others). However, these procedures are effective in a vary small subset of patients. Further, “mass effect” from the FS/FG itself may lead to new focal neurological deficits. Rather, these recurrent CSF fisutlas/ DT typically require direct surgical repair (i.e., open surgical closure of recurrent CSF fistulas/DT).
Contraindication for interventional radiologists percutaneously treating a sacral meningeal cyst with FG
Hayashi et al. in 2014 (i.e. interventional radiologists) percutaneously injected FG into a sacral meningeal cyst (S2-S4) in a 64-year-old female complaining of persistent sacral pain.[
Failure of postoperative percutaneous techniques (epidural steroid injections (ESI), epidural blood patches (EBP)) to address recurrent lumbar CSF fistulas/DT
Contraindication for treating postoperative pain due to persistent CSF fistulas/DT with lumbar epidural steroid injections as they contribute to AA
The administration of epidural spinal injections (ESI) in patients with known or suspected recurrent/residual postoperative CSF fistulas/DT is contraindicated [
Use of targeted lumbar EBP to treat postoperative recurrent lumbar CSF fistulas/DT
Interventional radiologists perform EBPs, despite a significant lack of success, to treat postoperative residual/recurrent lumbar CSF fistulas/DT [
Lack of efficacy of secondary lumbar surgery to reverse neurological sequelae of AA
The majority of clinical studies acknowledge that postoperative lumbar AA is not a surgically-remediable lesion [
Unanticipated complication of lumbar AA – hydrocephalus
In 2008, Koerts et al. reported a single case in which a 45 year-old-male following multiple back operations developed spinal/lumbar AA, that additionally contributed to hydrocephalus [
CONCLUSION
Following lumbar surgery, CSF fisutlas/DT can recur postoperatively in up to 17% of cases. Early recognition and repair of such persistent postoperative recurrent CSF fistulas/DT are essential to avoid the evolution of AA with its permanent and progressive neurological sequelae.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agulnick M, Cohen BR, Epstein NE. Unique bone suture anchor repair of complex lumbar cerebrospinal fluid fistulas. Surg Neurol Int. 2020. 11: 153
2. Anderson TL, Morris JM, Wald JT, Kotsenas AL. Imaging appearance of advanced chronic adhesive arachnoiditis: A retrospective review. AJR Am J Roentgenol. 2017. 209: 648-55
3. Dolan RA. Spinal adhesive arachnoiditis. Surg Neurol. 1993. 39: 479-84
4. Eisenberg E, Goldman R, Schlag-Eisenberg D, Grinfeld A. Adhesive arachnoiditis following lumbar epidural steroid injections: A report of two cases and review of the literature. J Pain Res. 2019. 12: 513-8
5. Faltings L, Kulason KO, Du V, Schneider JR, Chakraborty S, Kwan K. Early epidural blood patch to treat intracranial hypotension after iatrogenic cerebrospinal fluid leakage from lumbar tubular microdiscectomy. Cureus. 2018. 10: e3633
6. Hayashi K, Nagano J, Hattori S. Adhesive arachnoiditis after percutaneous fibrin glue treatment of a sacral meningeal cyst. J Neurosurg Spine. 2014. 20: 763-6
7. Hughes SA, Ozgur BM, German M, Taylor WR. Prolonged Jackson-Pratt drainage in the management of lumbar cerebrospinal fluid leaks. Surg Neurol. 2006. 65: 410-4
8. Johnston JD, Matheny JB. Microscopic lysis of lumbar adhesive arachnoiditis. Spine (Phila Pa 1976). 1978. 3: 36-9
9. Jurga S, Szymańska-Adamcewicz O, Wierzchołowski W, Pilchowska-Ujma E, Urbaniak Ł. Spinal adhesive arachnoiditis: Three case reports and review of literature. Acta Neurol Belg. 2021. 121: 47-53
10. Koerts G, Rooijakkers H, Abu-Serieh B, Cosnard G, Raftopoulos C. Postoperative spinal adhesive arachnoiditis presenting with hydrocephalus and cauda equina syndrome. Clin Neurol Neurosurg. 2008. 110: 171-5
11. Moussa WM, Aboul-Enein HA. Combined thrombin and autologous blood for repair of lumbar durotomy. Neurosurg Rev. 2016. 39: 591-7
12. Parenti V, Huda F, Richardson PK, Brown D, Aulakh M, Taheri MR. Lumbar arachnoiditis: Does imaging associate with clinical features?. Clin Neurol Neurosurg. 2020. 192: 105717
13. Peng H, Conermann T.editors. Arachnoiditis. Treasure Island, FL: StatPearls Publishing; 2020. p.
14. Ribeiro C, Reis FC. Adhesive lumbar arachnoiditis. Acta Med Port. 1998. 11: 59-65
15. Tsuchida R, Sumitani M, Azuma K, Abe H, Hozumi J, Inoue R. A novel technique using magnetic resonance imaging in the supine and prone positions for diagnosing lumbar adhesive arachnoiditis: A preliminary study. Pain Pract. 2020. 20: 34-43
16. Wong AK, Rasouli MR, Ng A, Wang D. Targeted epidural blood patches under fluoroscopic guidance for incidental durotomies related to spine surgeries: A case series. J Pain Res. 2019. 12: 2825-33