- Department of Neurosurgery, Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and c/o Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA. 1122 Franklin Avenue Suite 106 Garden City, NY 11530., USA
Correspondence Address:
Nancy E Epstein, M.D, Clinical Professor of Neurosurgery, State University of New York at Stony Brook, NY c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY 11530 and Editor-in-Chief of Surgical Neurology International.
DOI:10.25259/SNI_193_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A Agulnick2. Perspective: Early direct repair of recurrent postoperative cerebrospinal (CSF) fluid leaks: No good evidence epidural blood patches (EBP) work. 31-Mar-2023;14:120
How to cite this URL: Nancy E. Epstein1, Marc A Agulnick2. Perspective: Early direct repair of recurrent postoperative cerebrospinal (CSF) fluid leaks: No good evidence epidural blood patches (EBP) work. 31-Mar-2023;14:120. Available from: https://surgicalneurologyint.com/surgicalint-articles/12222/
Abstract
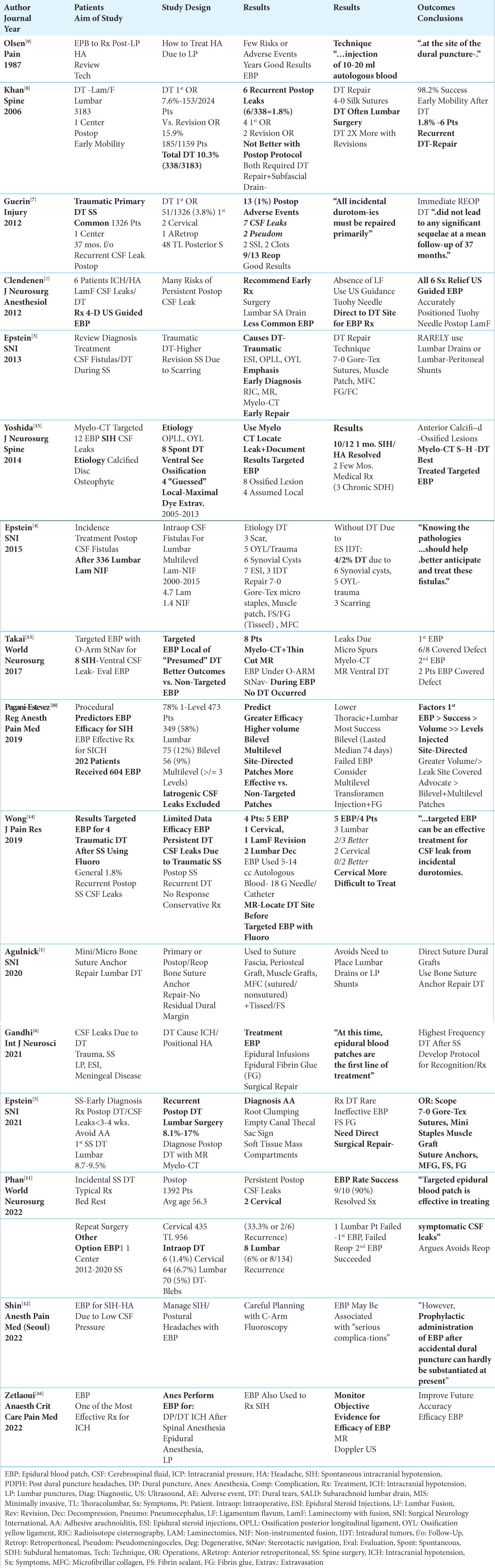
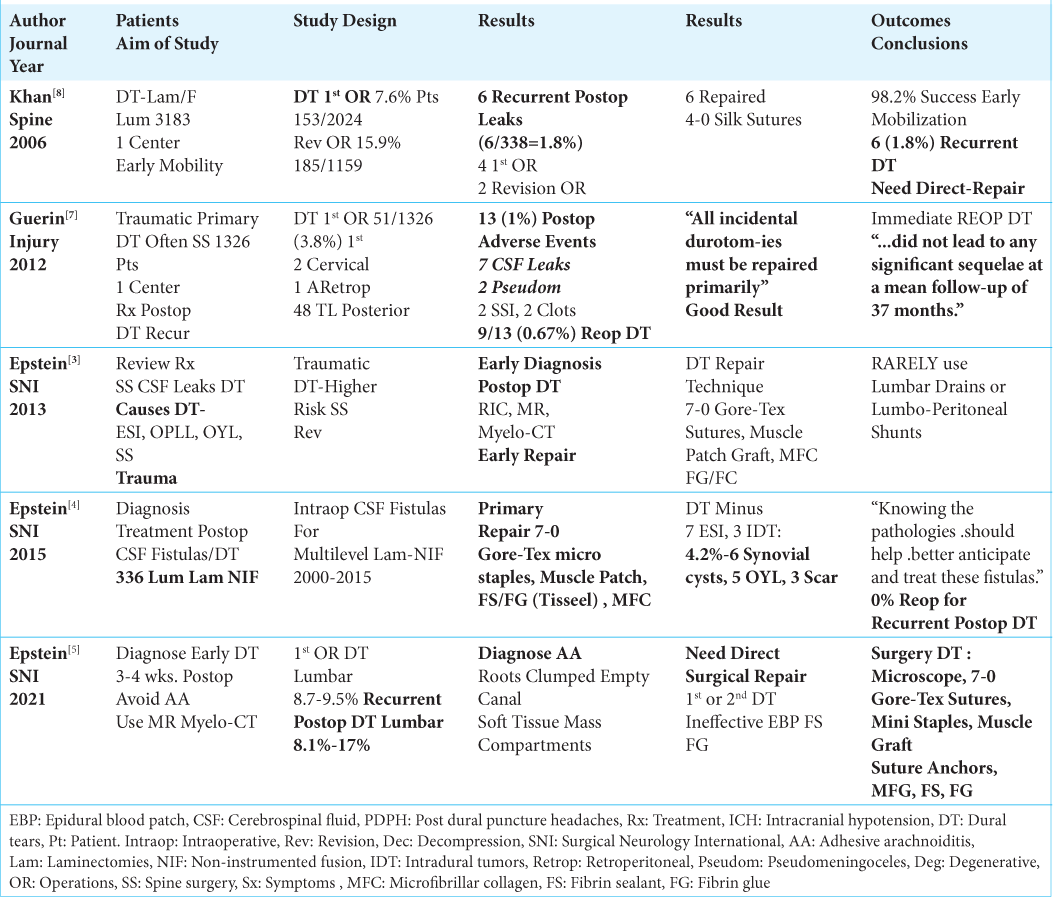
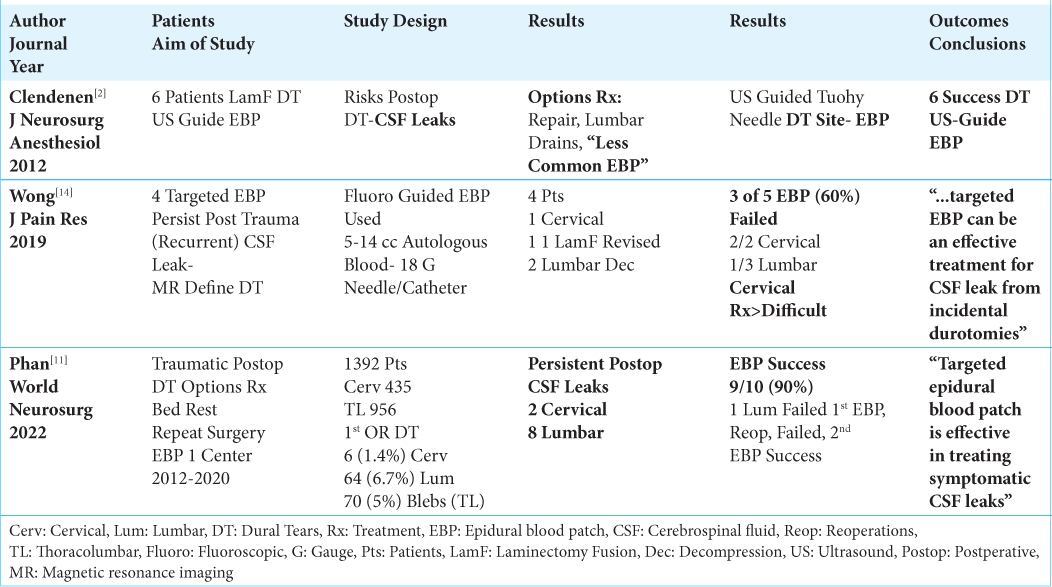
Background: “Targeted” epidural blood patches (EBP)” successfully treat “focal dural tears (DT)” diagnosed on thin-cut MR or Myelo-CT studies. These DT are largely attributed to; epidural steroid injections (ESI), lumbar punctures (LP), spinal anesthesia (SA), or spontaneous intracranial hypotension (SICH). Here we asked whether “targeted EBP” could similarly treat MR/Myelo-CT documented recurrent post-surgical CSF leaks/DT that have classically been effectively managed with direct surgical repair.
Methods: Utilizing ultrasound, fluoroscopy, or O-arm guidance, “targeted EBP” effectively manage “focal DT” attributed to ESI, LP, SA, or SICH. Here we reviewed the literature to determine whether similar “targeted EBP” could effectively manage recurrent postoperative CSF leaks/DT.
Results: We were only able to identify 3 studies involving just 20 patients that attempted to utilize EBP to control postoperative CSF fistulas/DT. EBP controlled CSF fistulas/DT in 6 patients in the first study, and 9 of 10 patients (i.e. 90%: 2/2 cervical; 7/8 lumbar) in the second study. However, in the third study, 3 (60%) of 5 EBP failed to avert recurrent CSF leaks/DT in 4 patients (i.e. 1 cervical patient (2 EBP failed attempts), 3 lumbar patients (1 failed EBP)).
Conclusion: Early direct surgical repair of recurrent postoperative spinal CSF leaks/DT remains the treatment of choice. Our literature review revealed 3 underpowered studies including just 20 patients where 20% of EBP failed to control recurrent postoperative fistulas (range of failure from 0-60% per study). Although there are likely other studies we failed to identify in this review, they too are likely insufficiently powered to document significant efficacy for performing EBP over direct surgical repair for recurrent postoperative CSF leaks/DT.
Keywords: Spontaneous intracranial hypotension (SICH), Dural tear (DT), Dural repair, Cerebrospinal fluid (CSF) leak, Epidural blood patch (EBP), Fluoroscopy, Targeted EBP, Myelo-CT, MR, Postoperative recurrent lumbar CSF leaks, Insufficient evidence
INTRODUCTION
“Focal cerebrospinal fluid (CSF) leaks/dural tears (DT)” identified on Myelo-CT and/or thin-cut MR studies are largely attributed to; epidural steroid injections (ESI), lumbar punctures (LP), spinal anesthesia (SA), or spontaneous intracranial hypotension (SICH) [
Symptoms and Etiology of Intracranial Hypotension
Patients may present with classical symptoms/signs of intracranial hypotension (ICH) due to newly occurrent or recurrent CSF leaks/DT [
Primary or Recurrent Postoperative CSF Fistulas/DT Warranting Direct Surgical Repair
The rates for primary intraoperative (3.0 - 27%) and recurrent postoperative CSF leaks/DT (1.8 - 17.6%) varies [
Direct Dural Repair Techniques Address Primary/ Recurrent Postoperative CSF Fistulas/DT
In multiple studies, patients underwent primary intraoperative and/or recurrent postoperative direct surgical repair of CSF leaks/DT [
“Targeted” EBP Performed Under Ultrasound, Fluoroscopy, or O-Arm Guidance
EBP involve the epidural injection of a small volume of autologous blood (i.e. 5-20 cc) to occlude a CSF fistulas/ DT [
Several Studies Documented SICH Were Effectively Treated With “Targeted EBP”
For SICH, Myelo-CT and thin-cut MR studies documented that DT were effectively treated with ultrasound, fluoroscopy, and/or O-arm guided “targeted EBP” [
Adverse Events Resulting From Epidural Blood Patches (EBP) to Treat Post LP Dural Punctures
Adverse events (AE) resulting from the application of EBP may include; complications of blood directly entering the CSF pathways, (i.e. sterile meningeal response, adhesive arachnoiditis, and hydrocephalus with cephalad migration amongst others), infection, abscess formation, direct neural compression (i.e. potential for acute cauda equina syndrome), creation of additional sites of dural puncture, and persistent intracranial hypotension [
Lack of Evidence that EBP “Effectively” Treat Recurrent Postoperative Lumbar CSF Fistulas/DT
The 3 studies we were able to identify in the literature involving just 20 patients did not document the efficacy for utilizing EBP to treat recurrent postoperative CSF leaks/DT [
CONCLUSION
Epidural blood patches (EBP) successfully treat “focal DT” largely attributed to epidural steroid injections (ESI), lumbar punctures (LP), spinal anesthesia (SA) or spontaneous (SICH). Here, however, as we found insufficient evidence in the 3 studies we identified to support utilizing EBP rather than the classically accepted direct dural repair techniques to treat recurrent postoperative CSF leaks/DT.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agulnick MA, Cohen BR, Epstein NE. Unique Bone suture anchor repair of complex lumbar cerebrospinal fluid fistulas. Surg Neurol Int. 2020. 11: 153
2. Clendenen SR, Pirris S, Robards CB, Leone B, Nottmeier EW. Symptomatic postlaminectomy cerebrospinal fluid leak treated with 4-dimensional ultrasound-guided epidural blood patch. J Neurosurg Anesthesiol. 2012. 24: 222-5
3. Epstein NE. A review article on the diagnosis and treatment of cerebrospinal fluid fistulas and dural tears occurring during spinal surgery. Surg Neurol Int. 2013. 4: S301-17
4. Epstein NE. Incidence and management of cerebrospinal fluid fistulas in 336 multilevel laminectomies with non instrumented fusions. Surg Neurol Int. 2015. 6: S463-8
5. Epstein NE. Perspective: Early diagnosis and treatment of postoperative recurrent cerebrospinal fluid fistulas/dural tears to avoid adhesive arachnoiditis. Surg Neurol Int. 2021. 12: 208
6. Gandhi J, DiMatteo A, Joshi G, Smith NL, Khan SA. Cerebrospinal fluid leaks secondary to dural tears: A review of etiology, clinical evaluation, and management. Int J Neurosci. 2021. 131: 689-95
7. Guerin P, El Fegoun AB, Obeid I, Gille O, Lelong L, Luc S. Incidental durotomy during spine surgery: Incidence, management and complications. A retrospective review. Injury. 2012. 43: 397-401
8. Khan MH, Rihn J, Steele G, Davis R, Donaldson WF, Kang JD. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: A review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976). 2006. 31: 2609-13
9. Olsen KS. Epidural blood patch in the treatment of post-lumbar puncture headache. Pain. 1987. 30: 293-301
10. Pagani-Estevez GL, Cutsforth-Gregory JK, Morris JM, Mokri B, Piepgras DG, Mauck WD, editors. Procedural predictors of epidural blood patch efficacy in spontaneous intracranial hypotension. Reg Anesth Pain Med. Jan 13, 2019. p. rapm-2018-000021
11. Phan A, Shah S, Joo P, Mesfin A. Can cervical and lumbar epidural blood patches help avoid revision surgery for symptomatic postoperative dural tears?. World Neurosurg. 2022. 164: e877-83
12. Shin YH. Recent update on epidural blood patch. Anesth Pain Med (Seoul). 2022. 17: 12-23
13. Takai K, Taniguchi M. Targeted epidural blood patch under O-arm-guided stereotactic navigation in patients with intracranial hypotension associated with a spinal cerebrospinal fluid leak and ventral dural defect. World Neurosurg. 2017. 107: 351-7
14. Wong AK, Rasouli MR, Ng A, Wang D. Targeted epidural blood patches under fluoroscopic guidance for incidental durotomies related to spine surgeries: A case series. J Pain Res. 2019. 12: 2825-33
15. Yoshida H, Takai K, Taniguchi M. Leakage detection on CT myelography for targeted epidural blood patch in spontaneous cerebrospinal fluid leaks: Calcified or ossified spinal lesions ventral to the thecal sac. J Neurosurg Spine. 2014. 21: 432-41
16. Zetlaoui PJ, Buchheit T, Benhamou D. Epidural blood patch: A narrative review. Anaesth Crit Care Pain Med. 2022. 41: 101138