- Clinical Prof. of Neurosurgery, School of Medicine, State University of New York at Stony Brook, NY, and c/o Dr. Marc Aglulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA.
Correspondence Address:
Nancy Epstein MD, Clinical Professor of Neurosurgery, School of Medicine, State University of New York at Stony Brook and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA.
DOI:10.25259/SNI_509_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy Epstein. Perspective on morbidity and mortality of cervical surgery performed in outpatient/same day/ambulatory surgicenters versus inpatient facilities. 12-Jul-2021;12:349
How to cite this URL: Nancy Epstein. Perspective on morbidity and mortality of cervical surgery performed in outpatient/same day/ambulatory surgicenters versus inpatient facilities. 12-Jul-2021;12:349. Available from: https://surgicalneurologyint.com/surgicalint-articles/10959/
Abstract
Background: This is an updated analysis of the morbidity and mortality of cervical surgery performed in outpatient/same day (OSD) (Postoperative care unit [PACU] observation 4–6 h), and ambulatory surgicenters (ASC: PACU 23 h) versus inpatient facilities (IF).
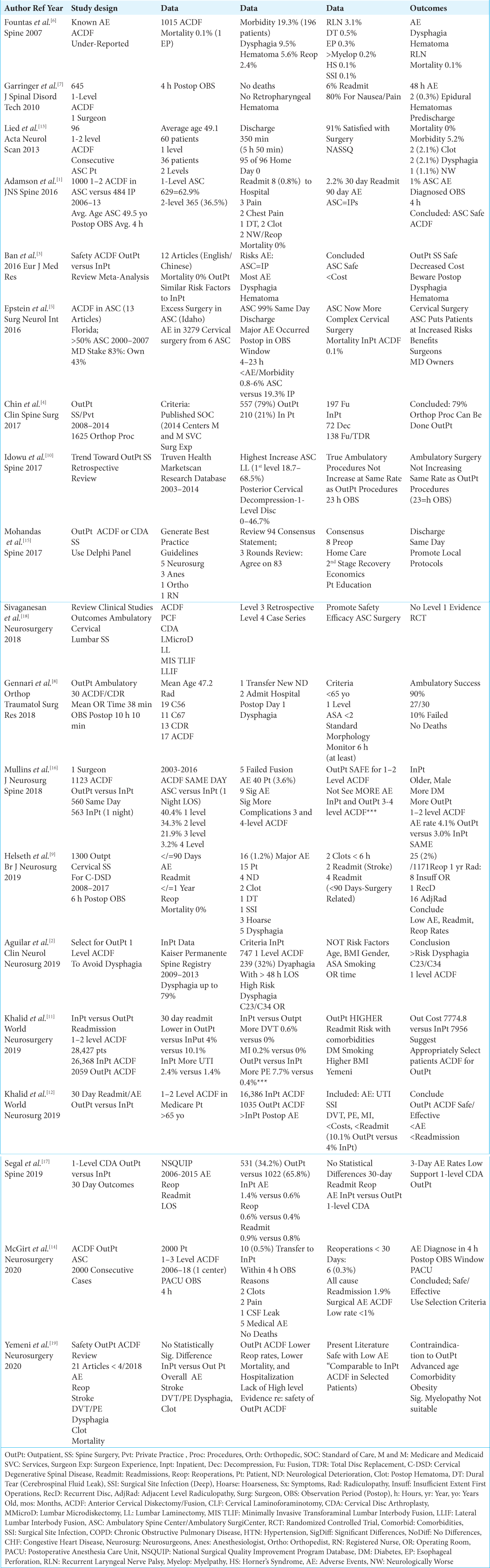
Methods: We analyzed 19 predominantly level III (retrospective) and IV (case series) studies regarding the morbidity/mortality of cervical surgery performed in OSC/ASC versus IF.
Results: A “selection bias” clearly favored operating on younger/healthier patients to undergo cervical surgery in OSD/ASC centers resulting in better outcomes. Alternatively, those selected for cervical procedures to be performed in IF classically demonstrated multiple major comorbidities (i.e. advanced age, diabetes, high body mass index, severe myelopathy, smoking, 3–4 level disease, and other comorbidities) and had poorer outcomes. Further, within the typical 4–6 h. PACU “observation window,” OSD facilities “picked up” most major postoperative complications, and typically showed 0% mortality rates. Nevertheless, the author’s review of 2 wrongful death suits (i.e. prior to 2018) arising from OSD ACDF cervical surgery demonstrated that there are probably many more mortalities occurring following discharges from OSD where cervical operations are being performed that are going underreported/unreported.
Conclusion: “Selection bias” favors choosing younger/healthier patients to undergoing cervical surgery in OSD/ ASC facilities resulting in better outcomes. Atlernatively, choosing older patients with greater comorbidities for IF surgery correlated with poorer results. Although most OSD cervical series report 0% mortality rates, a review of 2 wrongful death suits by just one neurosurgeon prior to 2018 showed there are probably many more mortalities resulting from OSD cervical surgery than have been reported.
Keywords: Ambulatory surgical centers, Cervical disc replacement, Efficacy, Morbidity, Mortality, Multilevel, Outpatient/same day surgery, Safety, Update, anterior cervical diskectomy/fusion
INTRODUCTION
In our 2016 review, the results of cervical spine surgery performed in outpatient/same day (OSD) or ambulatory surgicenters (ASC) were compared to those performed in inpatient facilities (IF) [
LOW LEVEL III (RETROSPECTIVE) AND IV (CASE SERIES) EVIDENCE FOR STUDIES COMPARING OSD/ASC VERSUS IF CERVICAL SURGERY
Two studies questioned the safety/efficacy of performing cervical surgery in OSD/ASC versus IF facilities [
GREATER GROWTH FOR ASC (23 h) VERSUS OSD (4–6 h) SPINE SURGERY
Idowu et al. (2017) documented, using a large research database, greater growth in the number of ASC-performed lumbar laminectomies and posterior cervical procedures versus those performed in OSD facilities [
MAJOR POSTOPERATIVE ADVERSE EVENTS (AE) FOLLOWING CERVICAL SURGERY “PICKED UP” WITHIN POSTOPERATIVE CARE UNIT (PACU) “OBSERVATION WINDOWS” OF 4–6 h FOR OSD AND UP TO 23 h FOR ASC
Multiple studies documented that major postoperative complications following cervical surgery were “picked up” in PACU “observation windows” that respectively ranged from 4 to 6 h for OSD, and up to 23 h for ASC [
TWO STUDIES DOCUMENTED COMPARABLE OUTCOMES FOR OSD/ASC VERSUS IF CERVICAL SURGERY
Two studies demonstrated the non-superiority/comparable outcomes for cervical surgery performed in OSD/ASC versus IF [
RISK FACTORS TO AVOID WHEN SELECTING PATIENTS TO UNDERGO OSD/ASC CERVICAL SURGERY
Multiple studies identified significant risk factors to be avoided when choosing patients for cervical surgery in OSD/ASC vs. IF surgery [
“SELECTION BIAS” FAVORS YOUNGER/ HEALTHIER PATIENTS FOR OSD/ASC CERVICAL SURGERY
Several studies documented a deliberate patient “selection bias” favoring younger/healthier patients to undergo OSD/ ASC versus IF cervical surgery [
COMPARABLE 30-DAY OUTCOMES FOR 1-LEVEL CERVICAL DISC ARTHROPLASTY (CDA) PERFORMED IN ASC VERSUS IF
Segal et al. (2019) looked at 30-day outcomes for patients undergoing 1 level CDA performed in ASC versus IF [
0% MORTALITY RATES REPORTED FOR OSD/ ASC (4–6–10 H) AND ASC (23 H) CERVICAL SURGERY
6 Clinical series showed 0% mortality rates for OSD/ASD versus 0.1% for IF cervical surgery
In 2007, Fountas et al. documented 1 death (0.1%: esophageal perforation) occurring out of 1015 patients undergoing ACDF in an inpatient setting (IF).[
3 Other review articles showed 0% to low mortality rates for OSD/ASC ACDF surgery
Three other review articles found 0% to “low” mortality rates for cervical surgery performed in OSD/ASC versus 0% to higher mortality rates for IF cervical procedures [
2 MEDICOLEGAL SUITS PRIOR TO 2018 REVEALED 2 MORTALITIES OCCURRING AFTER ACDF PERFORMED IN OSC
The author performed expert medicolegal reviews in 2 cases (prior to 2018) involving wrongful deaths occurring after patients were discharged from OSD following ACDF. The first case involved a single-level ACDF with a cardiorespiratory arrest occurring within several hours of discharge; the patient sutained a major hypoxic injury, and expired the following day. The second case had a multilevel ACDF with discharge home within just 4 hours of surgery; this patient also sustained a cardiorespiratory arrest at home but remained vegetative on a respirator for a year prior to their demise. Note, that if just one neurosurgical expert could identify 2 such wrongful death suits following cervical surgery performed in OSD/ASC facilities, there are probably many more that have gone unreported.
CONCLUSION
Selection “bias” favors choosing younger/healthier patients to undergo cervical surgery in OSD/ASC facilities results in better outcomes. Alternatively, performing cervical surgery on older patients with more medical comorbidities in inpatient facilities yields anticipated poorer results. Of interest, few to no mortalities were reported in the literature attributed to cervical surgery performed in OSD/ASC facilities. Nevertheless, the author alone was a plaintiffs’ expert in 2 wrongful death suits prior to 2018 attributed to cervical procedures performed in OSD. Therefore, there are likely more such suits in the medicolegal literature, and more mortalities from these OSC/ ASC cervical procedures that are going under-unreported.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adamson T, Godil SS, Mehrlich M, Mendenhall S, Asher AL, McGirt MJ. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: Analysis of 1000 consecutive cases. J Neurosurg Spine. 2016. 24: 878-84
2. Aguilar DD, Brara HS, Rahman S, Harris J, Prentice HA, Guppy KH. Exclusion criteria for dysphagia for outpatient single-level anterior cervical discectomy and fusion using inpatient data from a spine registry. Clin Neurol Neurosurg. 2019. 180: 28-33
3. Ban D, Liu Y, Cao T, Feng S. Safety of outpatient anterior cervical discectomy and fusion: A systematic review and meta-analysis. Eur J Med Res. 2016. 21: 34
4. Chin KR, Pencle FJ, Coombs AV, Packer CF, Hothem EA, Seale JA. Eligibility of outpatient spine surgery candidates in a single private practice. Clin Spine Surg. 2017. 30: E1352-8
5. Epstein NE. Cervical spine surgery performed in ambulatory surgical centers: Are patients being put at increased risk?. Surg Neurol Int. 2016. 7: S686-91
6. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007. 32: 2310-7
7. Garringer SM, Sasso RC. Safety of anterior cervical discectomy and fusion performed as outpatient surgery. J Spinal Disord Tech. 2010. 23: 439-43
8. Gennari A, Mazas S, Coudert P, Gille O, Vita JM. Outpatient anterior cervical discectomy: A French study and literature review. Orthop Traumatol Surg Res. 2018. 104: 581-4
9. Helseth O, Lied B, Heskestad B, Ekseth K, Helseth E. Retrospective single-centre series of 1300 consecutive cases of outpatient cervical spine surgery: Complications, hospital readmissions, and reoperations. Br J Neurosurg. 2019. 33: 613-9
10. Idowu OA, Boyajian HH, Ramos E, Shi LL, Lee MJ. Trend of spine surgeries in the outpatient hospital setting versus ambulatory surgical center. Spine (Phila Pa 1976). 2017. 42: E1429-36
11. Khalid SI, Carlton A, Wu R, Kelly R, Peeta A, Adogwa O. Outpatient and inpatient readmission rates of 1-and 2-level anterior cervical discectomy and fusion surgeries. World Neurosurg. 2019. 126: e1475-81
12. Khalid SI, Adogwa O, Ni A, Cheng J, Bagley C. A comparison of 30-day hospital readmission and complication rates after outpatient versus inpatient 1 and 2 level anterior cervical discectomy and fusion surgery: An analysis of a medicare patient sample. World Neurosurg. 2019. 129: e233-9
13. Lied B, Ronning PA, Halvorsen CM, Ekseth K, Helseth E. Outpatient anterior cervical discectomy and fusion for cervical disk disease: A prospective consecutive series of 96 patients. Acta Neurol Scand. 2013. 127: 31-7
14. McGirt MJ, Rossi V, Peters D, Dyer H, Coric D, Asher AL. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting: Analysis of 2000 consecutive cases. Neurosurgery. 2020. 86: E310-5
15. Mohandas A, Summa C, Worthington WB, Lerner J, Foley KT, Bohinski RJ. Best practices for outpatient anterior cervical surgery: Results from a Delphi panel. Spine (Phila Pa 1976). 2017. 42: E648-59
16. Mullins J, Poiskic M, Boop FA, Arnautovic KI. Retrospective single-surgeon study of 1123 consecutive cases of anterior cervical discectomy and fusion: A comparison of clinical outcome parameters, complication rates, and costs between outpatient and inpatient surgery groups, with a literature review. J Neurosurg Spine. 2018. 28: 630-41
17. Segal DN, Wilson JM, Staley C, Yoon ST. Outpatient and inpatient single-level cervical total disc replacement: A comparison of 30-day outcomes. Spine (Phila Pa 1976). 2019. 44: 79-83
18. Sivaganesan A, Hirsch B, Philllips FM, McGirt MJ. Spine surgery in the ambulatory surgery center setting: Value-based advancement or safety liability?. Neurosurgery. 2018. 83: 159-65
19. Yemeni K, Burke JF, Chunduru P, Moliinaro AM, Riew KD, Traynelis VC. Safety of outpatient anterior cervical discectomy and fusion: A systematic review and meta-analysis. Neurosurgery. 2020. 86: 30-45