- Neurosurgery Department, Hospital de Clínicas “José de San Martín”, School of Medicine, University of Buenos Aires, Buenos Aires, Argentina.
- Department of Neurological Surgery, Trauma and Emergency Hospital “Dr. Federico Abete”, Buenos Aires, Argentina.
- Department of Neurosurgery, Pediatric Hospital “Prof. Dr. Juan P. Garrahan”, Buenos Aires, Argentina.
- Department of Radiology, Pediatric Hospital “Prof. Dr. Juan P. Garrahan”, Buenos Aires, Argentina.
Correspondence Address:
Federico E. Minghinelli, Neurosurgery Department, Hospital de Clínicas “José de San Martín”, School of Medicine, University of Buenos Aires, Buenos Aires, Argentina.
DOI:10.25259/SNI_211_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Federico E. Minghinelli1, Yamila Basilotta Marquez2, Derek Orlando Pipolo3, Rodolfo José Recalde1, Beatriz Mantese2, Carlos Rugilo4. “Ping-pong” fracture: An exclusive entity of neonates and infants? A case analysis and literature review. 12-May-2023;14:170
How to cite this URL: Federico E. Minghinelli1, Yamila Basilotta Marquez2, Derek Orlando Pipolo3, Rodolfo José Recalde1, Beatriz Mantese2, Carlos Rugilo4. “Ping-pong” fracture: An exclusive entity of neonates and infants? A case analysis and literature review. 12-May-2023;14:170. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12320
Abstract
Background: “Ping-pong” fractures are a type of depressed fracture in which there is no rupture of the inner or outer table of the skull. It is produced by incomplete bone mineralization. Its appearance is frequent during neonatal and infant ages and is extremely rare outside of these age periods. The objective of this article is to present the case of a 16-year-old patient who presented a “ping-pong” fracture after a traumatic brain injury (TBI) and discuss the underlying physiopathogenesis of these types of fractures.
Case Description: A 16-year-old patient presented to the emergency department with a TBI, referring headaches and nausea. Non-contrast brain computed tomography displayed a left parietal “ping-pong” fracture. Laboratory tests showed hypocalcemia, subsequently diagnosing hypoparathyroidism. The patient remained under observation for 48 h. He was managed conservatively and started on calcium carbonate and vitamin D supplements with a favorable evolution. Hospital discharge was granted with TBI discharge instructions and warning signs.
Conclusion: The age of presentation of our case was atypical, according to the reported literature. When faced with a “ping-pong” fracture outside of an early age, underlying bone pathologies must be ruled out, which could potentially generate incomplete bone mineralization of the skull.
Keywords: Age, Bone mineralization, Depressed, Fracture, “Ping-pong”
INTRODUCTION
“Ping-pong” fractures are a type of depressed fracture, in which there is no rupture of the inner or outer table of the skull.[
Rahimi et al. described that Albucasis (Arabic surgeon who lived in the Middle Ages from 936 to 1013 AD) defined “ping-pong” fracture as follows: It is a fracture due to a fall or blow from a stone or similar, causing a dent in the surface of the bone, this occurs mainly in heads whose bones are soft, such as those of babies.[
There is abundant information in the literature regarding the appearance of these fractures during neonatal and infant periods, but little is known about their appearance at later ages. The objective of this article is to present the case of a 16-year-old patient who presented a “ping-pong” fracture after a traumatic brain injury (TBI) and discuss the underlying physiopathogenesis of these types of fractures.
CLINICAL CASE
A 16-year-old patient with no relevant history presented a TBI without loss of consciousness. The patient reported headaches, nausea, and dizziness. On physical examination, the patient was alert, oriented in all spheres, with reactive intermediate isochoric pupils, mobilizing 4 extremities on command, without sensory-motor deficits or gait disturbances.
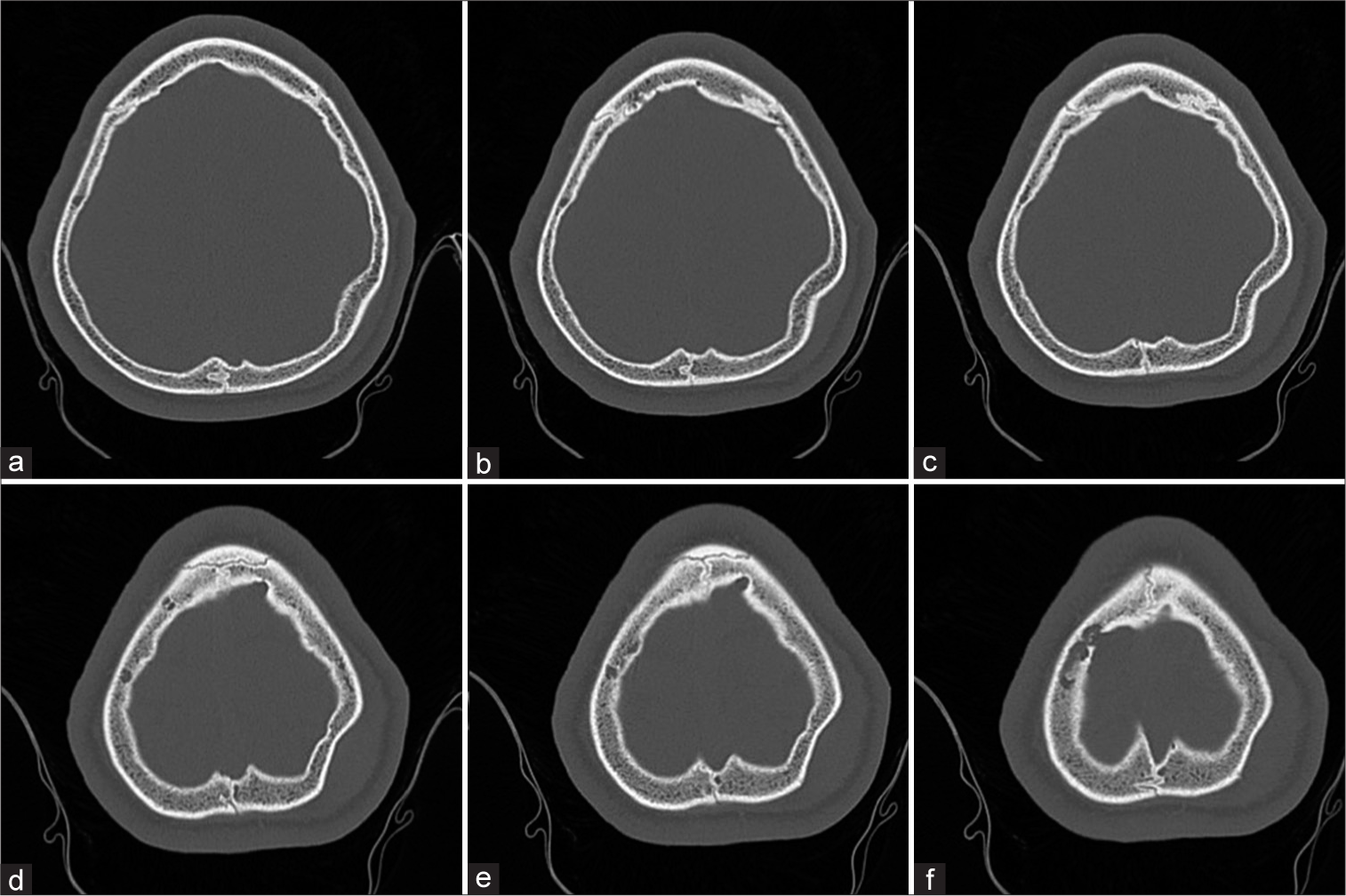
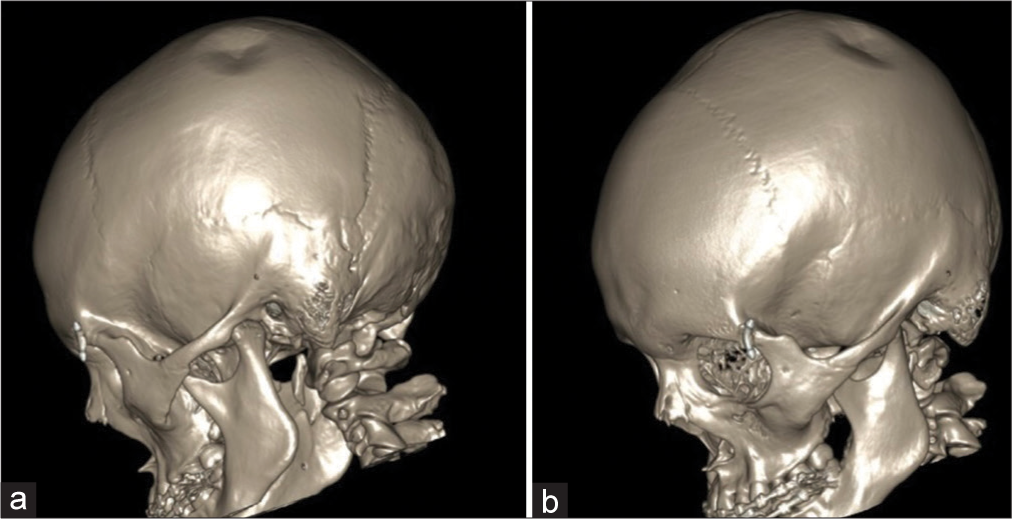
A brain computed tomography (CT) without contrast was performed, displaying a “ping-pong” fracture with a diameter of 30.5 mm and depression of 9.2 mm. No intraparenchymal lesions were identified. Brain CT bone window and 3D reconstruction showed the fracture in the left parietal bone [
Laboratory tests were performed and showed low values of ionic and total serum calcium (4.8 mg/dL and 7.8 mg/dL, respectively). With this result, the serum parathyroid hormone (PTH) levels were analyzed, which showed a low value as well (6 mg/dL), diagnosing hypocalcemia and hypoparathyroidism. Consultation with the endocrinology service was made and the patient started on calcium carbonate and vitamin D supplements, remaining under observation in the general ward for 48 h with a favorable evolution. Due to the absence of neurological deficits, intraparenchymal lesions, large cosmetic defects, and/or symptomatic progression, conservative management was performed. Hospital discharge was granted with follow-up instructions and TBI warning signs. The patient did not attend the last control (6 months after the trauma), so the evolution of the depressed “ping pong” fracture is unknown. In the previous control (1 month after the trauma), there were no complications.
DISCUSSION
Bone mineralization begins during the embryonic phase of human development, but most of this process occurs in the third trimester of gestation. Osteoblasts control organic bone matrix production and subsequent calcium and phosphate deposition, generating progressive expansion of bone volume through an increase in trabecular thickness.[
There are two types of depressed fractures, those with rupture of the inner and outer table of the skull and those without rupture of them. These last ones are called “ping-pong” fractures.[
Rubin et al. conducted a study to measure the characteristics of bone tissue in patients with hypoparathyroidism before and after the administration of recombinant human PTH (rh PTH). The authors concluded that while rh PTH may have short-term beneficial effects on cancellous bone microarchitecture, further studies are required to explore whether the treatment of hypoparathyroidism with rh PTH affects skeletal strength and fracture incidence.[
A possible explanation for the appearance of “ping-pong” fractures outside the neonatal and infant period is undiagnosed nutritional, endocrinological, and/or autoimmune disorders (among others), which could potentially generate incomplete mineralization of the skull.[
CONCLUSION
We have presented the case of a 16-year-old patient who presented a “ping-pong” fracture after a TBI. The age of presentation was atypical, according to the reported literature. When faced with a “ping-pong” fracture outside of an early age, underlying bone pathologies (nutritional, endocrinological, and/or autoimmune, among others) must be ruled out, which could potentially generate incomplete bone mineralization of the skull. However, we believe that more cases must be studied to accurately reveal the physiopathogenesis of these fractures outside their predominant age range.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Haddad SA, Kirollos R. A 5-year study of the outcome of surgically treated depressed skull fractures. Ann R Coll Surg Engl. 2002. 84: 196-200
2. Ballestero MF, De Oliveira RS. Closed depressed skull fracture in childhood reduced with suction cup vacuum method: Case report and a systematic literature review. Cureus. 2019. 11: e5205
3. De Paul Djientcheu V, Njamnshi AK, Ongolo-Zogo P, Ako S, Essomba A, Sosso MA. Depressed skull fractures in children: Treatment using an obstetrical vacuum extractor. Pediatr Neurosurg. 2006. 42: 273-6
4. Faienza MF, D’Amato E, Natale MP, Grano M, Chiarito M, Brunetti G. Metabolic bone disease of prematurity: Diagnosis and management. Front Pediatr. 2019. 7: 143
5. Hung KL, Liao HT, Huang JS. Rational management of simple depressed skull fractures in infants. J Neurosurg. 2005. 103: 69-72
6. Kovacs CS. Bone development and mineral homeostasis in the fetus and neonate: Roles of the calciotropic and phosphotropic hormones. Physiol Rev. 2014. 94: 1143-218
7. Lafita J. Bone physiology and pathophysiology. Ann Health Syst Navar. 2003. 26: 7-17
8. López-Elizalde R, Leyva-Mastrapa T, Muñoz-Serrano JA, Godínez-Rubí M, Preciado-Barón K, Velázquez-Santana H. Ping pong fractures: Treatment using a new medical device. Childs Nerv Syst. 2013. 29: 679-83
9. Minghinelli FE, Recalde R, Socolovsky M, Houssay A. A new, low-cost device to treat depressed “ping-pong” fractures non-surgically: Technical note. Childs Nerv Syst. 2021. 37: 2045-9
10. Minghinelli FE, Recalde R, Socolovsky M, Houssay A. A new, readily accessed and low-cost, device for treating depressed ping pong fractures non-surgically: Technical note. Neurocirugia (Astur: Engl Ed). 2022. 33: 328-33
11. Muresan GC, Hedesiu M, Lucaciu O, Boca S, Petrescu N. Effect of Vitamin D on bone regeneration: A review. Medicina (Kaunas). 2022. 58: 1337
12. Murgio A, Andrade FA, Muñoz MA, Boetto S, Leung KM. International multicenter study of head injury in children. ISHIP Group. Childs Nerv Syst. 1999. 15: 318-21
13. Murguía-González A, Hernández-Herrera RJ, Nava-Bermea M. Risk factors of birth obstetric trauma. Ginecol Obstet Mex. 2013. 81: 297-303
14. Muzzo BS, Cordero J, Ceresa S, Buchel E, Gajardo LH, Leiva BL. Bone mineralization in patients with liver failure. Chil J Nutr. 2004. 31: 40-5
15. Prakash A, Harsh V, Gupta U, Kumar J, Kumar A. Depressed fractures of skull: An institutional series of 453 patients and brief review of literature. Asian J Neurosurg. 2018. 13: 222-6
16. Rahimi SY, McDonnell DE, Ahmadian A, Vender JR. Medieval neurosurgery: Contributions from the Middle East, Spain, and Persia. Neurosurg Focus. 2007. 23: E14
17. Rho JY, Ashman RB, Turner CH. Young’s modulus of trabecular and cortical bone material: Ultrasonic and microtensile measurements. J Biomech. 1993. 26: 111-9
18. Rodríguez MC, Medina BR, Jiménez EG, Pérez CF, Schmidt-Riovalle J. Bone mineralization levels are influenced by body composition in children and adolescents. Hosp Nutr. 2014. 30: 763-8
19. Rubin MR, Zwahlen A, Dempster DW, Zhou H, Cusano NE, Zhang C. Effects of parathyroid hormone administration on bone strength in hypoparathyroidism. J Bone Miner Res. 2016. 31: 1082-8
20. Rustico SE, Calabria AC, Garber SJ. Metabolic bone disease of prematurity. J Clin Transl Endocrinol. 2014. 1: 85-91
21. Samuel N, Jacob R, Eilon Y, Mashiach T, Shavit I. Falls in young children with minor head injury: A prospective analysis of injury mechanisms. Brain Injury. 2015. 29: 946-50
22. Steinbok P, Flodmark O, Martens D, Germann ET. Management of simple depressed skull fractures in children. J Neurosurg. 1987. 66: 506-10