- Department of Neurosurgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
- Department of Neurosurgery, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India.
- Department of Dentistry, Government Medical College, Chandigarh, India.
- Department of Radiotherapy, Postgraduate Institute of Medical Education and Reserach, Chandigarh, India.
Correspondence Address:
Manjul Tripathi
Department of Radiotherapy, Postgraduate Institute of Medical Education and Reserach, Chandigarh, India.
DOI:10.25259/SNI_729_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Manjul Tripathi1, Nishanth Sadashiva2, Anand Gupta3, Parth Jani1, Sachin Jose Pulickal2, Harsh Deora2, Rupinder Kaur1, Parwinder Kaur1, Aman Batish1, Sandeep Mohindra1, Narendra Kumar4. Please spare my teeth! Dental procedures and trigeminal neuralgia. 22-Dec-2020;11:455
How to cite this URL: Manjul Tripathi1, Nishanth Sadashiva2, Anand Gupta3, Parth Jani1, Sachin Jose Pulickal2, Harsh Deora2, Rupinder Kaur1, Parwinder Kaur1, Aman Batish1, Sandeep Mohindra1, Narendra Kumar4. Please spare my teeth! Dental procedures and trigeminal neuralgia. 22-Dec-2020;11:455. Available from: https://surgicalneurologyint.com/surgicalint-articles/10480/
Abstract
Background: The correct diagnosis of trigeminal neuralgia (TN) is still a far cry and the patients suffer from unnecessary dental procedures before getting the definite treatment. In this study, we evaluated, if the patients have undergone dental procedures for their misdiagnosed TN before receiving definite treatment for the same.
Methods: A total of 187 patients received GKRS for their TN (excluding secondary TN) in two institutes from 2010 to 2019. We did a retrospective analysis of these patients’ primary complaints on a standard questionnaire.
Results: One hundred and seventeen of the 187 patients responded. About 55.5% of patients had a toothache and 65.8% did visit a dentist for the pain. About 41.8% of patients underwent one dental procedure; 18.8% suffered from worsening of the pain while 8.5% received some partial improvement. About 19.6% also underwent root canal treatment while 6.8% had a nerve block. Mean of 1.6 teeth was extracted per person. About 71% of patients were satisfied with their Gamma Knife radiosurgery for TN at a median follow-up of 49 months.
Conclusion: There is a need for a better understanding of the disease among the dentists and the patients for the timely and correct treatment, without losing their teeth. The onus lies on neurosurgeons/neurologists disseminate knowledge regarding proper diagnosis and treatment modalities.
Keywords: Facial pain, Gamma knife radiosurgery, Microvascular decompression, Tooth extraction, Trigeminal neuralgia
INTRODUCTION
“It is very common that patients experiencing neuralgia of the second or third branch of the trigeminal nerve, at the beginning of their suffering, will have extracted all teeth of the affected region. Generally, on a thorough examination, it will be easily recognized, whether the pain originates from the teeth or not.”
-Fedor Krause (1857–1937)
Trigeminal neuralgia (TN) is a serious health problem characterized by recurrent unilateral brief electric shock-like pains, abrupt in onset and termination, limited to the distribution of one or more divisions of the trigeminal nerve, and triggered by innocuous stimuli.[
Usually, patients with TN have triggers that cause these painful attacks. These triggers may be laughing, chewing, shaving, brushing their teeth, or even cold breeze over the face. The pain usually involves the maxillary division of trigeminal nerve, often in combination with the mandibular division, but involvement of the supraorbital nerve is infrequent.[
MATERIALS AND METHODS
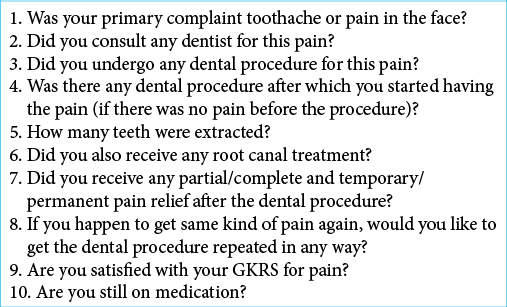
All patients, who have undergone primary GKRS at two institutes for TN from 2010 to 2019, were retrospectively reviewed for the history of toothache and previous visits to the dentist. All patients who had secondary TN were excluded from the study. The available information from the chart reviews was recorded and later they were contacted on the phone. Consent was taken for their telephonic interview. Details of their initial pain pattern, any visit to the dentist, treatment received, postprocedural pain relief, the need for medications, and time taken for them to visit specialists were recorded [
RESULTS
During the study period, a total of 187 patients were treated with GKRS. One hundred and seventeen patients could be contacted for this study. The mean age was 57 years and 134 (71.65%) were male. Sixty-five (55.5%) patients had described that they felt like they had perceived toothache associated with the symptoms, and 77 (65.8%) of the patients had visited a dentist before visiting the neurosurgeon. Out of these patients, 49 (41.8%) had undergone some procedure during their visit to a dentist. Interestingly, 22 patients reported that their pain had actually either started or aggravated after their dental procedure and 10 of the patients reported temporary partial relief from their pain after the dental procedure. Forty-nine patients had their tooth extracted ranging from 1 to 4 in number with a mean of 1.6 teeth extracted per person. Twenty-three patients also had root canal treatments and eight patients received regional nerve blocks 1–3 times, along with tooth extraction. On asking patients, if they would undergo another dental procedure if required for pain relief only 2 patients out of 10 who had initially got partial relief replied that they would repeat a similar procedure. Eighty-three (71%) patients replied that they were satisfied with their expectations after GKRS treatment though 90 (77%) patients were still on some sort of medications for their facial pain at a median follow-up of 49 months (1–108 months).
DISCUSSION
The correct diagnosis: onus is on the dentist
Our study and available literature show that many patients visit dentists for their TN.[
Essentially, the diagnosis of TN remains clinical. Dental pain is usually provoked by direct percussion to a tooth or application of cold/hot beverages.[
A substantial number of patients may have concurrent dental problems due to poor oral hygiene or other reasons that may exacerbate the symptoms of TN. This is especially true considering the severe pain triggered by brushing in patients with TN. Any patient complaining of continuous pain in the tooth or periodontal structures is most commonly suffering from dental disease. Rarely, TN may also feature with pain arising from trigger areas in the mouth.[
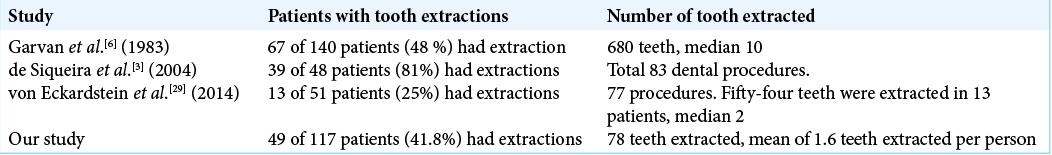
In a study done by Garvan et al. in Zurich in 1983, 73% of patients with a history of TN had already taken a dental consultation and 48% had at least one tooth extracted.[
In a study done by de Siqueira et al. in 2004, 31 (65%) of the 48 interviewed patients had undergone a total of 83 dental procedures.[
A recent study done by von Eckardstein et al. in 2014, they reported that 41 patients (82%) of the 51 evaluated patients had initially consulted their dentists out of which 27 (53%) patients received invasive dental treatment including extractions, root canal treatments, and implants. The majority of the patients in that study had reported that their dentist had not recognized the exact problem. A total of 54 teeth were extracted in 13 patients with a median of 2 and a maximum of 20 teeth extractions. Of patients that reported to a dentist, 70.6 % did so within 4 weeks of the onset of symptoms, but more than 2 years elapsed before neurological or neurosurgical attention in 42.5% of patients.[
Our study showed similar results compared to the previous studies [
Postprocedure TGN: dental procedures and TGN: cause or effect
Many times, the patient is operated for a dental procedure and the patient reports TN as a temporal event secondary to the procedure. This again raises the question if the primary diagnosis was TN or otherwise. There remain chances of some iatrogenic injury to the inferior alveolar nerve/lingual nerve, leading to sensory neuropathy. The prevalence of temporarily impaired lingual and inferior alveolar nerve function is thought to range between 0.15 and 0.54%, whereas permanent injury caused by an injection of local analgesics is less frequent at 0.0001–0.01%.[
In a dentist analysis in the German population, only 74.5% of dentists felt competent enough to clinically diagnose TN from other orofacial pain syndromes. The majority (76.6%) felt that there is a need for further information and ongoing medical education regarding TN.[
iTGN and oral hygiene
Patients with TN often get reluctant to shave, brush, or floss as they may act as a triggering event hence such patients may not brush for many days to months.[
Limitations of the study
We have conducted a retrospective interview of our patients who have received GKRS for TN. We relied on patients charts and interview for the assessment of the prior history, whenever details were incomplete in case records. We did not contact the dentists for their evaluation, prior investigations, and their rationale for the treatment. It cannot be outrightly denied that individual dental treatment was justified in some patients as the dental problem may have coexisted with TN. However, with this analysis, we can easily identify that the risk of missed/wrong diagnosis is very high.
CONCLUSION
This is a high time to increase awareness about TN among dentists and primary caregivers. It requires a team approach to rule out dental causes before finalizing the diagnosis. Both are highly specialized specialties (neurosurgery and maxillofacial/dentistry) where each one has to complement each other for the best patient care. The onus equally lies on neurosurgeons/neurologists to differentiate typical TN from atypical TN and odontogenic pain. There are consensus guidelines for all the treatment modalities that should be regularly updated and published for the best of the treatment option. Moreover, the patient needs an early referral if the pain control is not satisfactory despite a prior dental procedure. If it is TN, even extraction of 32 teeth would not make the patient better, but only miserable.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Ethics Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge the guidance and case management by late Professor Kanchan Kumar Mukherjee, PGIMER, Chandigarh, for his vision and effort in successfully managing patients.
References
1. Adams H, Pendleton C, Latimer K, Cohen-Gadol AA, Carson BS, Quinones-Hinojosa A. Harvey cushing’s case series of trigeminal neuralgia at the johns hopkins hospital: A surgeon’s quest to advance the treatment of the suicide disease. Acta Neurochir (Wien). 2011. 153: 1043-50
2. Baad-Hansen L. Atypical odontalgia-pathophysiology and clinical management. J Oral Rehabil. 2008. 35: 1-11
3. de Siqueira SR, Nobrega JC, Valle LB, Teixeira MJ, de Siqueira JT. Idiopathic trigeminal neuralgia: Clinical aspects and dental procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 98: 311-5
4. Deora H, Tripathi M, Modi M, Mohindra S, Batish A, Gurnani J. Letter to the editor. Microsurgical rhizotomy as treatment for trigeminal neuralgia in patients with multiple sclerosis: Turnpike or dirt road?. J Neurosurg. 2018. 1: 1-4
5. Devor M, Wood I, Sharav Y, Zakrzewska JM. Trigeminal neuralgia during sleep. Pain Pract. 2008. 8: 263-8
6. Garvan NJ, Siegfried J. Trigeminal neuralgia-earlier referral for surgery. Postgrad Med J. 1983. 59: 435-7
7. . Headache Classification committee of the international headache society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia. 2018. 38: 1-211
8. Hillerup S. Iatrogenic injury to the inferior alveolar nerve: Etiology, signs and symptoms, and observations on recovery. Int J Oral Maxillofac Surg. 2008. 37: 704-9
9. Katusic S, Beard CM, Bergstralh E, Kurland LT. Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. Ann Neurol. 1990. 27: 89-95
10. Kim JH, Yu HY, Park SY, Lee SC, Kim YC. Pulsed and conventional radiofrequency treatment: Which is effective for dental procedure-related symptomatic trigeminal neuralgia?. Pain Med. 2013. 14: 430-5
11. Klazen Y, van der Cruyssen F, Vranckx M, van Vlierberghe M, Politis C, Renton T. Iatrogenic trigeminal post-traumatic neuropathy: A retrospective two-year cohort study. Int J Oral Maxillofac Surg. 2018. 47: 789-93
12. Law AS, Lilly JP. Trigeminal neuralgia mimicking odontogenic pain. A report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995. 80: 96-100
13. Maarbjerg S, di Stefano G, Bendtsen L, Cruccu G. Trigeminal neuralgia-diagnosis and treatment. Cephalalgia. 2017. 37: 648-57
14. Mumford JM. Role of the dentist in trigeminal neuralgia. Pain. 1978. 5: 83-92
15. Obermann M. Treatment options in trigeminal neuralgia. Ther Adv Neurol Disord. 2010. 3: 107-15
16. Olesen J. International classification of headache disorders. Lancet Neurol. 2018. 17: 396-7
17. Ram S, Teruel A, Kumar SK, Clark G. Clinical characteristics and diagnosis of atypical odontalgia: Implications for dentists. J Am Dent Assoc. 2009. 140: 223-8
18. Remick RA, Blasberg B, Barton JS, Campos PE, Miles JE. Ineffective dental and surgical treatment associated with atypical facial pain. Oral Surg Oral Med Oral Pathol. 1983. 55: 355-8
19. Renton T, Adey-Viscuso D, Meechan JG, Yilmaz Z. Trigeminal nerve injuries in relation to the local anaesthesia in mandibular injections. Br Dent J. 2010. 209: E15
20. Renton T, Thexton A, Crean SJ, Hankins M. Simplifying the assessment of the recovery from surgical injury to the lingual nerve. Br Dent J. 2006. 200: 569-73
21. Renton T. Tooth-related pain or not?. Headache. 2020. 60: 235-46
22. Rodriguez-Lozano FJ, Sanchez-Perez A, Moya-Villaescusa MJ, Rodriguez-Lozano A, Saez-Yuguero MR. Neuropathic orofacial pain after dental implant placement: Review of the literature and case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 109: e8-12
23. Siqueira SR, Teixeira MJ, de Siqueira JT. Severe psychosocial compromise in idiopathic trigeminal neuralgia: Case report. Pain Med. 2010. 11: 453-5
24. Tinastepe N, Oral K. Neuropathic pain after dental treatment. Agri. 2013. 25: 1-6
25. Tripathi M, Batish A.editors. Letter to the editor. Cafeteria approach to management of trigeminal neuralgia: Stereotactic radiosurgery as a preferred option. J Neurosurg. 2018. 1: 1-2
26. Tripathi M. Trigeminal neuralgia: An orphan with many fathers. Neurol India. 2019. 67: 414-6
27. Truelove E. Management issues of neuropathic trigeminal pain from a dental perspective. J Orofac Pain. 2004. 18: 374-80
28. Viana M, Tassorelli C, Allena M, Nappi G, Sjaastad O, Antonaci F. Diagnostic and therapeutic errors in trigeminal autonomic cephalalgias and hemicrania continua: A systematic review. J Headache Pain. 2013. 14: 14
29. von Eckardstein KL, Keil M, Rohde V. Unnecessary dental procedures as a consequence of trigeminal neuralgia. Neurosurg Rev. 2015. 38: 355-60