- Department of Surgery, Division of Neurosurgery, King Abdulaziz Medical City, Ministry of National Guard - Health Affairs, Riyadh, Saudi Arabia.
- College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
- King Abdullah International Medical Research Center, Riyadh, Saudi Arabia.
Correspondence Address:
Ahoud Alharbi, Department of Surgery, Division of Neurosurgery, King Abdulaziz Medical City, Ministry of National Guard -Health Affairs, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_994_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahoud Alharbi1,2,3, Sami Khairy1,3, Ahmed Alkhani1,3. Pneumocephalus after subcutaneous emphysema. 17-Jun-2022;13:249
How to cite this URL: Ahoud Alharbi1,2,3, Sami Khairy1,3, Ahmed Alkhani1,3. Pneumocephalus after subcutaneous emphysema. 17-Jun-2022;13:249. Available from: https://surgicalneurologyint.com/surgicalint-articles/11664/
Abstract
Background: Pneumocephalus is the presence of air in the intracranial cavity secondary to communication with the extracranial compartment. It occurs spontaneously, after trauma, or after a cranial surgery.
Case Description: A 62-year-old female, a known case of diabetes mellitus, presented to our emergency department with a sudden thunderclap headache. She was diagnosed with subarachnoid hemorrhage secondary to ruptured anterior communicating artery aneurysm. Twenty days later, she developed pneumonia and subsequently had a cardiac arrest. She was revived after 26 min of cardiopulmonary resuscitation. She developed pneumothorax requiring a chest tube insertion. After the first trial, she developed a diffuse subcutaneous emphysema, and the chest tube was reinserted. Afterward, she became unresponsive with dilated pupils. A computed tomography (CT) scan of the brain showed a diffuse subcutaneous emphysema reaching up to the face with air around the ventriculoperitoneal shunt distal catheter and extending through the burr hole to the ventricles causing pneumocephalus. There was no evidence of skull base fractures on brain CT. Unfortunately, the patient did not recover and passed away 3 days later.
Conclusion: This report describes the presentation and radiological findings of an interesting case of pneumocephalus following iatrogenic diffuse subcutaneous emphysema. It aims to increase the emphasis on early anticipation of such rare complication after subcutaneous emphysema.
Keywords: Emphysema, Iatrogenic, Pneumocephalus, Trauma
CLINICAL IMAGE
A 62-year-old female, known case of diabetes mellitus, presented to our emergency department with a sudden thunderclap headache accompanied by decreased level of consciousness. She was diagnosed with subarachnoid hemorrhage secondary to ruptured anterior communicating artery aneurysm; therefore, she underwent coiling of the aneurysm and insertion of ventriculoperitoneal (VP) shunt to treat the hydrocephalus. Her level of consciousness improved and she was started on physical therapy.
Twenty days after the surgery, she developed pneumonia that was complicated by a cardiac arrest. She was revived after 26 min of cardiopulmonary resuscitation. She developed pneumothorax requiring a chest tube insertion. After the first trial, she developed a diffuse subcutaneous emphysema, and the chest tube was reinserted. Afterward, she became unresponsive with dilated pupils.
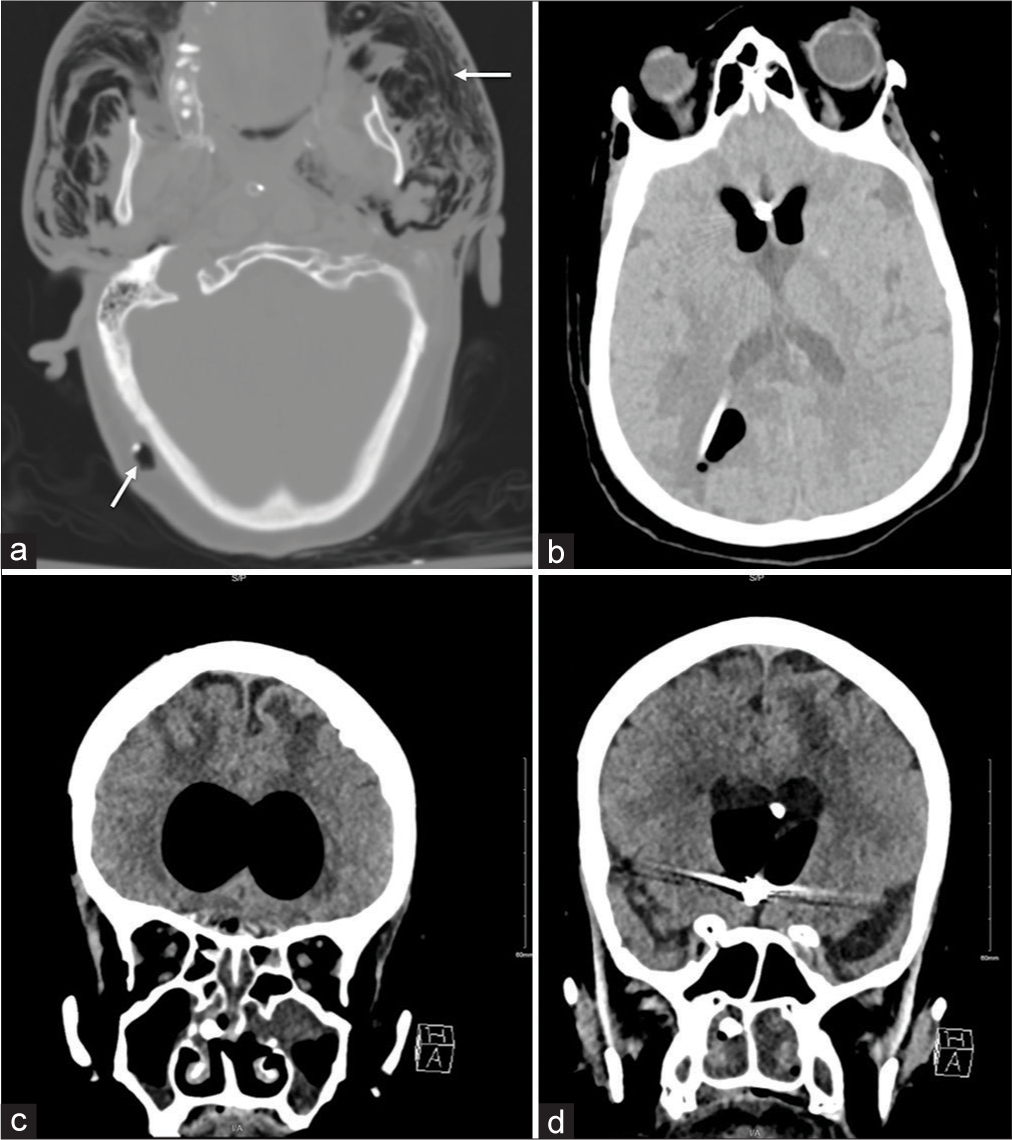
A computed tomography (CT) scan of the brain was done which showed diffuse subcutaneous emphysema reaching up to the face with air around the VP shunt distal catheter [
Figure 1:
Axial CT scan of the brain showing diffuse subcutaneous emphysema (a) reaching the face with air around the VP shunt distal catheter [arrows], (b) extending through the burr hole to the ventricles causing pneumocephalus, and (c and d) coronal CT scan of the brain showing intact skull base with no evidence of fractures.
Pneumocephalus is the presence of air in the intracranial cavity secondary to communication with the extracranial compartment. It occurs spontaneously, after trauma, or after a cranial surgery.[
There are two theories that can explain the pathophysiology of pneumocephalus. Ball valve theory states that air moves in one direction from outside to inside through cerebrospinal fluid (CSF) leakage.[
CONCLUSION
Upon review of the literature, pneumocephalus is an extremely rare complication after iatrogenic subcutaneous emphysema and remains insufficiently reported. We are reporting the presentation and radiological findings of an interesting case of pneumocephalus following iatrogenic diffuse subcutaneous emphysema. This report aims to increase the emphasis on early anticipation of such rare complication after subcutaneous emphysema.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dabdoub CB, Salas G, do Silveira EN, Dabdoub CF. Review of the management of pneumocephalus. Surg Neurol Int. 2015. 6: 155
2. Das JM, Bajaj J.editors. Pneumocephalus. Treasure Island, FL: StatPearls; 2020. p.
3. Ruiz-Juretschke F, Mateo-Sierra O, Iza-Vallejo B, CarrilloYagüe R. Intraventricular tension pneumocephalus after transsphenoidal surgery: A case report and literature review. Neurocirugia (Astur). 2007. 18: 134-7
4. Solomiichuk VO, Lebed VO, Drizhdov KI. Posttraumatic delayed subdural tension pneumocephalus. Surg Neurol Int. 2013. 4: 37