- Department of Neurosurgery, Burrell College of Osteopathic Medicine, Las Cruces, New Mexico,
- Department of Neurosurgery, Lake Erie College of Osteopathic Medicine, Bradenton, Florida,
- Department of Neurosurgery, Riverside University Health System, Moreno Valley, California, United States.
Correspondence Address:
Mackenzie Eileen Goodrich
Department of Neurosurgery, Riverside University Health System, Moreno Valley, California, United States.
DOI:10.25259/SNI_503_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mackenzie Eileen Goodrich1, Adam M. Wolberg2, Samir Kashyap3, Stacey Podkovik3, Jacob Bernstein3, James Wiginton IV3, Raed Sweiss3. Pneumocephalus causing oculomotor nerve palsy: A case report. 25-Sep-2020;11:302
How to cite this URL: Mackenzie Eileen Goodrich1, Adam M. Wolberg2, Samir Kashyap3, Stacey Podkovik3, Jacob Bernstein3, James Wiginton IV3, Raed Sweiss3. Pneumocephalus causing oculomotor nerve palsy: A case report. 25-Sep-2020;11:302. Available from: https://surgicalneurologyint.com/surgicalint-articles/10291/
Abstract
Background: Pneumocephalus, the presence of gas or air within the intracranial cavity, is a common finding after cranial procedures, though patients often remain asymptomatic. Rare cases of cranial nerve palsies in patients with pneumocephalus have been previously reported. However, only two prior reports document direct unilateral compression of the third cranial nerve secondary to pneumocephalus, resulting in an isolated deficit.
Case Description: A 26-year-old male developed a unilateral oculomotor (III) nerve palsy after repair of a cerebrospinal fluid leak. The pneumocephalus was treated with a combination of an epidural drain, external ventricular drain (EVD), and high-flow oxygen. Following treatment, repeat computed tomography imaging of the head demonstrated that the pneumocephalus was progressively resorbed and the patient’s deficit resolved.
Conclusion: In rare cases, isolated cranial nerve palsies, specifically of the third cranial nerve, can result from pneumocephalus following cranial procedures. Acute cranial nerve palsy secondary to pneumocephalus will often resolve without intervention as the air is resorbed, but direct decompression with an epidural drain and an EVD may expedite the resolution of deficits.
Keywords: Cranial nerve, Oculomotor, Pneumocephalus
INTRODUCTION
Pneumocephalus by definition is the presence of gas or air within the intracranial cavity. This collection may be localized to various compartments and potential spaces, including epidural, subdural, subarachnoid, intracerebral, or intraventricular. Although commonly found postoperatively in craniectomy or craniotomy surgical procedures, pneumocephalus is a rare finding outside of surgery, often caused by trauma (75%), infection (9%, most commonly chronic otitis media), or tumors with involvement of the intracranial space, sinuses, orbit, or nasal passages.[
A review of the literature highlights a shortage of reports on isolated cranial nerve deficits related to pneumocephalus.[
CASE PRESENTATION
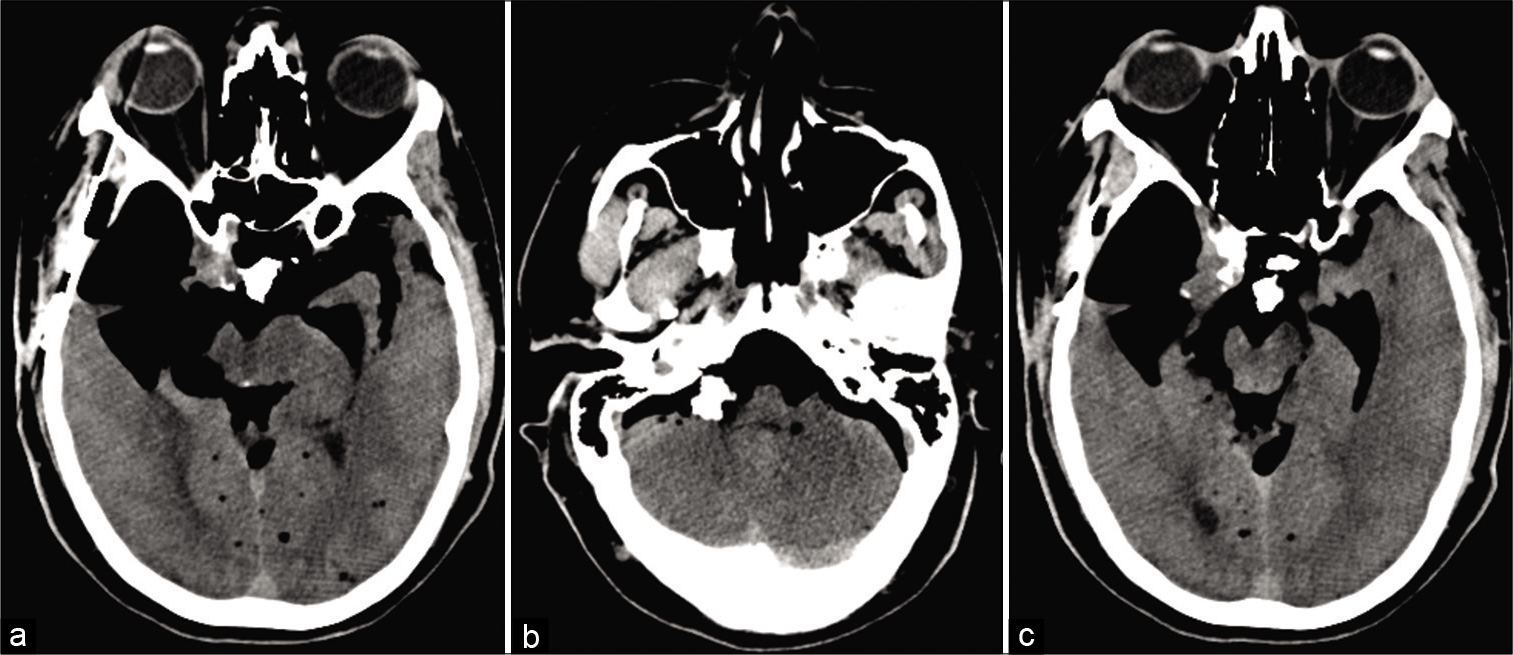
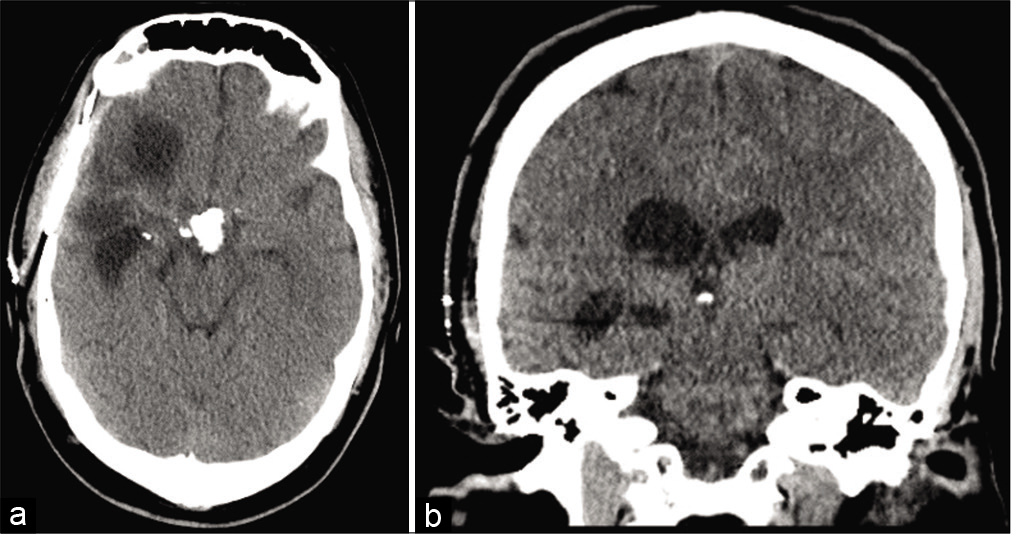
A 26-year-old male with a history of the right temporal chondrosarcoma resected in 2010 with subsequent self-limiting CSF rhinorrhea presented 8 years later with new-onset left temporal headaches. MRI of his brain at this time showed a right temporal contrast enhancing lesion suspicious for recurrent intracranial chondrosarcoma measuring 2.1 cm × 1.9 cm. He was monitored at 3 month intervals with repeat MRIs which showed stability of the mass. Approximately 1 year later, he presented with new-onset seizures and MRI findings that demonstrated an increase in size to 2.4 cm × 2.4 cm with evidence of encephalomalacia of the right temporal lobe. He subsequently underwent a repeat right craniotomy for resection. Pathology confirmed the lesion was World Health Organization Grade 1 chondrosarcoma. Several weeks later, he presented with a pseudomeningocele and a history of fevers. Seventy milliliters of subgaleal fluid were drained followed by a reexploration of his cranial incision and a wound washout. At this time, a small defect was noted in the frontal bone near the frontal sinus. The mucosa of the defect was obliterated with electrocautery, packed with muscle graft, then covered with Duragen® (Integra LifeSciences) and sealed with DuraSeal® (Integra LifeSciences). A subgaleal drain was placed and discontinued 2 days postoperatively. Cultures from CSF and pseudomeningocele specimens grew MSSA and he was started on appropriate antibiotics. Two months later, he presented with positional headaches and intermittent fluid leaking from his nose that started 2–3 weeks after his wound washout. A fluid sample was collected and was positive for β2-transferrin. He was admitted from the clinic and a lumbar drain was placed for CSF diversion. Shortly after, he complained of severe nuchal rigidity and headaches. CT head without contrast was performed [
The lumbar drain was clamped and the patient subsequently underwent right craniotomy which exposed a small dural opening in the temporal region, as well as a small opening in the previously repaired frontal sinus. The frontal sinus defect was repaired by removing the remaining mucosa and muscle in the sinus, and cauterizing the walls. Temporalis muscle was packed into the sinus and Mimix® bone cement was used to close off the frontal sinus. Duragen was subsequently laid over the hardened cement as well as the temporal dural defect and sealed with DuraSeal. A larger piece of Duragen was used to cover the remainder of the surgical exposure. The bone flap was secured to the skull with titanium plates and screws. The temporalis muscle was approximated and the galea and skin were closed. CT imaging preoperatively demonstrated large frontal pneumocephalus in the right cerebral hemisphere [
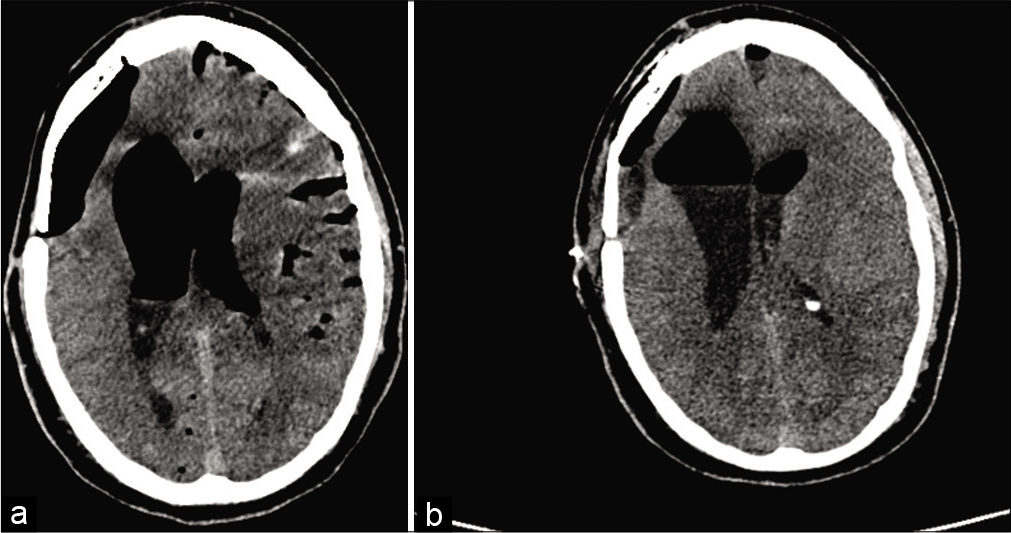
On postoperative day (POD) 2, the patient developed a large and minimally reactive right pupil consistent with an oculomotor nerve III palsy. Repeat imaging showed persistent right pneumocephalus [
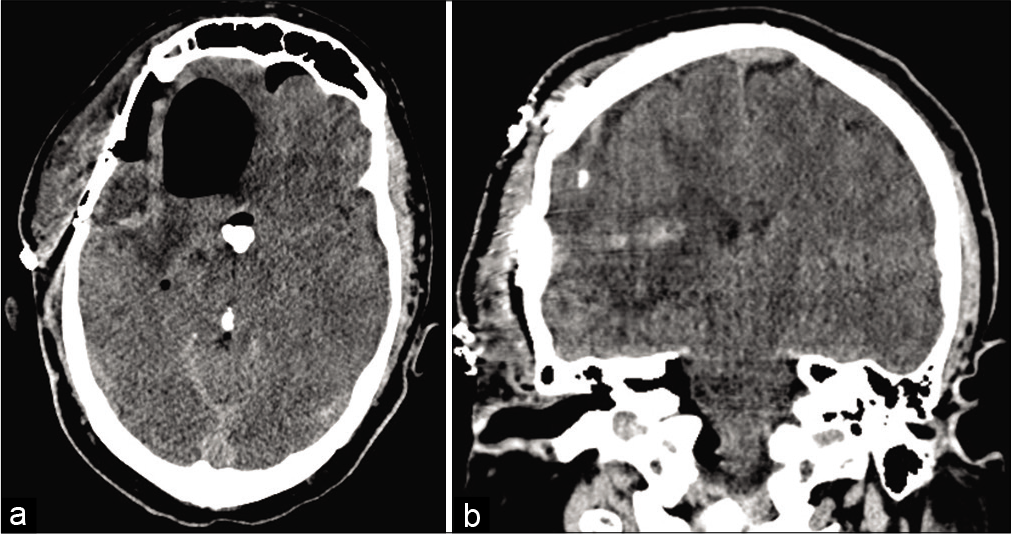
On POD 3, the patient was found to have a right CN III and VI palsy. The patient then underwent placement of a right-sided epidural drain and external ventricular drain (EVD) with subsequent improvement in pupil size and reactivity over the next couple of days [
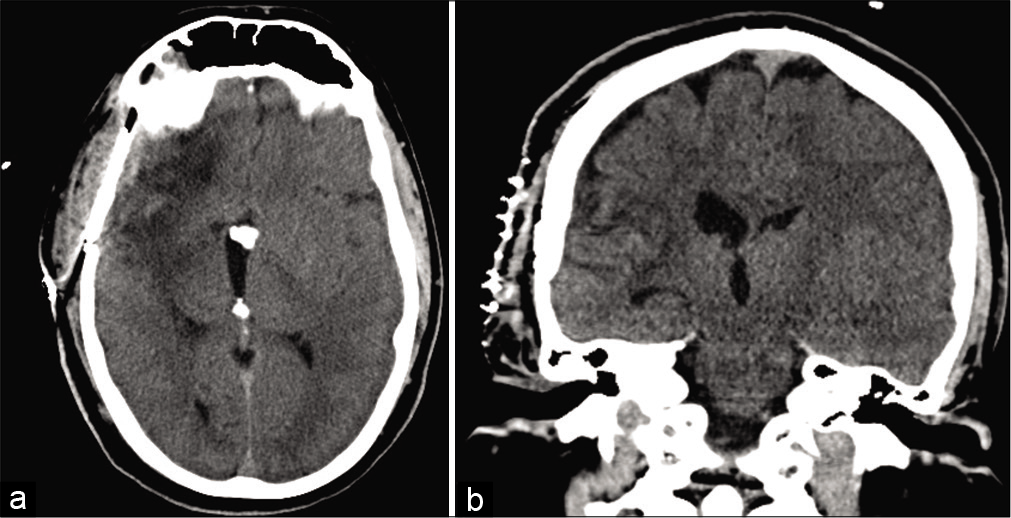
Subsequent imaging demonstrated improved pneumocephalus, and the epidural and ventricular drains were removed on days 6 and 9, respectively. The patient was discharged POD 10 with no recurrence of cranial nerve palsy. A follow-up CT scan was done on POD 15 revealing decreased amounts of pneumocephalus [
DISCUSSION
Pneumocephalus is almost inevitable after cranial surgery, most specifically after supratentorial craniotomies as was the case with our patient. Reasoner et al. examined 240 scans of patients undergoing supratentorial craniotomies between 1986 and 1990 and found air in 100% of the scans within the first 2 PODs.[
Review of the literature demonstrated reports ranging from no neurological symptoms to severe neurological deficits caused by distortion and displacement of the normal brain which required emergent surgery to evacuate the air. However, there are very few case reports of pneumocephalus postcraniotomy causing isolated cranial nerve palsies.
Marupudi et al. described a case of a patient who developed a bilateral pupil-sparing oculomotor nerve palsy from pneumocephalus after a right occipital craniotomy with complete resection of the cystic pineal mass through a transtentorial interhemispheric approach.[
To the best of our knowledge, there are only two cases reported depicting a unilateral nonpupil sparing oculomotor nerve palsy caused by pneumocephalus. This seems remarkably low considering the long course these nerves traverse, starting in the midbrain, and travelling along the lateral walls of the cavernous sinus to innervate the extraocular muscles and pupillary sphincter, which gives a significant amount of places for compression to occur.[
Our patient developed a nonpupil sparing oculomotor palsy on POD 2 with substantial improvement in pupil size after high-flow oxygen and placement of both epidural and EVD. Comparing our patient’s rapid improvement to the previously mentioned patients’ resolution over months, there may be an indication for an epidural and/or EVD in addition to high-flow oxygen. High-flow oxygen is thought to resolve pneumocephalus by reducing the partial pressure of nitrogen in the blood and brain parenchyma. Nitrogen gas makes up 78% of atmospheric air and is fairly insoluble in the blood. Its absorption depends on its partial pressure which is inversely proportional to the fraction of inspired oxygen. By giving 100% oxygen to treat pneumocephalus, the concentration of nitrogen gas is decreased, thus increasing its absorption concentration gradient.[
CONCLUSION
Pneumocephalus is an extremely common finding following craniotomy. This pathology is often caused by the trapping of air on closure, leakage through breaks in dural integrity, or traction secondary to negative intracranial pressure as a result of drainage. Our patient developed such severe pneumocephalus that it resulted in a unilateral oculomotor nerve palsy. Other causes of mass effect, such as tumor or hematoma, are more often associated with oculomotor nerve palsy, however, it is uncommon for pneumocephalus to cause similar symptoms. Although rare, the direct relationship between this cranial nerve deficit and pneumocephalus requires further research, as the oculomotor nerve pathway is relatively lengthy in comparison to the other cranial nerve tracts. In addition, presentation of a third nerve palsy is unique in regards to pupil and nonpupil-sparing symptomatology, which depends on central versus peripheral nerve fibers, respectively. Acute cranial nerve palsy secondary to pneumocephalus will often resolve without intervention as the air is resorbed, however, direct decompression may expedite resolution of deficits as seen in our case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dabdoub CB, Salas G, Silveira EN, Dabdoub CF. Review of the management of pneumocephalus. Surg Neurol Int. 2015. 6: 155
2. Han Y, Sun J, Wang Z. Pneumocephalus-induced oculomotor nerve palsy after atlanto-occipital decompression with dural plasty. J Craniofac Surg. 2017. 28: e543-5
3. Leong KM, Vijayananthan A, Sia SF, Waran V. Pneumocephalus: An uncommon finding in trauma. Med J Malaysia. 2008. 63: 256-8
4. Li WF, Kovacs K, Fisayo AA. Pneumocephalus and sixth nerve palsy after epidural steroid injection: Case report and review of the literature. J Emerg Med. 2017. 53: e89-92
5. Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien). 1967. 16: 1-78
6. Marupudi NI, Mittal M, Mittal S. Delayed pneumocephalus-induced cranial neuropathy. Case Rep Med. 2013. 2013: 105087
7. McIntosh BC, Strugar J, Narayan D. Traumatic frontal bone fracture resulting in intracerebral pneumocephalus. J Craniofac Surg. 2005. 16: 461-3
8. Modi P, Arsiwalla T.editors. Cranial Nerve III Palsy. Treasure Island, FL: StatPearls Publishing; 2019. p.
9. Nadeau SE, Trobe JD. Pupil sparing in oculomotor palsy: A brief review. Ann Neurol. 1983. 13: 143-8
10. Onur OO, Demir H, Guneysel O. Asymptomatic pneumocephalus after head trauma: Case report. BMJ Case Rep. 2009. 2009: 1028
11. Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of pneumocephalus after supratentorial craniotomy, Observations on the disappearance of intracranial air. Anesthesiology. 1994. 80: 1008-12
12. Steele WJ, Barber SM, Lee AG, West GA. Isolated, transient, pneumocephalus-induced oculomotor neuropathy after microvascular decompression of the trigeminal nerve. World Neurosurg. 2016. 88: 690.e17-22
13. Stevens QE, Colen CB, Ham SD, Kattner KA, Sood S. Delayed lateral rectus palsy following resection of a pineal cyst in sitting position: Direct or indirect compressive phenomenon?. J Child Neurol. 2007. 22: 1411-4
14. Third Cranial Nerve (Oculomotor Nerve) Palsy in Adults-UpToDate. Available from: https://www.uptodate.com/contents/third-cranial-nerve-oculomotor-nerve-palsy-in-adults [Last accessed on 2019 Sep 11].