- Departments of Spine, King Fahad Specialist Hospital, Dammam, Saudi Arabia,
- Neurology, Neuroscience Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia,
- Department of Anesthesia, King Fahad Specialist Hospital, Dammam, Saudi Arabia,
- King Faisal Medical City, Abha, Saudi Arabia,
- McMaster University, Hamilton, Canada.
Correspondence Address:
Elamir Bachar Harfouch, Department of Spine, Neuroscience Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia.
DOI:10.25259/SNI_67_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Elamir Bachar Harfouch1, Reem Fahd Bunyan2, Mona Al Faraidy3, Haitham H. Alnemari4,5, Shahid Bashir2. Ponte osteotomies increase risk of intraoperative neuromonitoring alerts in adolescent idiopathic scoliosis surgery. 15-Apr-2022;13:154
How to cite this URL: Elamir Bachar Harfouch1, Reem Fahd Bunyan2, Mona Al Faraidy3, Haitham H. Alnemari4,5, Shahid Bashir2. Ponte osteotomies increase risk of intraoperative neuromonitoring alerts in adolescent idiopathic scoliosis surgery. 15-Apr-2022;13:154. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11529
Abstract
Background: Ponte osteotomies (PO) are commonly used in adolescent idiopathic scoliosis (AIS) surgeries to improve the coronal and sagittal deformity correction. Here, we compared the incidence of perioperative neurologic complications for patients undergoing AIS with versus without PO.
Methods: In a retrospective cohort study of 80 consecutive AIS patients undergoing scoliosis correction, 40 underwent PO, while 40 did not. All operations were performed by one surgeon at one tertiary care center. Patients’ demographics, Lenke classifications, surgical data, and deformity characteristics were comparable in both groups. Perioperative neurologic complications, defined as spinal cord or nerve root injuries identified by the surgeon, were tracked for those undergoing AIS surgery with or without PO being performed.
Results: The risk of IOM alerts was significantly higher in the PO patients (12.5%: 5 patients) versus those in the No-PO group (0%, P = 0.021). Despite these changes, no patient incurred an increased postoperative deficit. Nevertheless, PO group patients demonstrated a higher coronal deformity correction rate (PO: 71% ± 10.9 vs. NoPO: 64.2% ± 11.5, P = 0.008) and a greater kyphosis Cobb angle (PO: 25.2 ± 6 vs. No-PO: 17.5 ± 9.4, P = 0.0001) on postoperative follow-up.
Conclusion: While PO improved 3D correction of AIS, it increased the risk of IOM alerts in 12.5% of cases.
Keywords: Adolescent idiopathic scoliosis, Ponte osteotomies, Spine deformity
INTRODUCTION
The incidence of new neurological deficits for adolescent idiopathic scoliosis (AIS) surgery with intraoperative monitoring is low (i.e., overall rate of 0.73% and rate for deformity/kyphosis, reaching 3.43%). [
Ponte osteotomy (PO) is one of the most frequently used to achieve three-dimensional correction of a spinal deformity. PO or Grade 2 Schwab’s osteotomy corrects long-segment thoracic kyphosis by shortening the posterior column in a single posterior stage.[
MATERIALS AND METHODS
After obtaining approval from the Institutional Review Board, data for 80 consecutive operations performed by one spine surgeon for AIS at a tertiary care center were collected (2014–2018). Exclusion criteria were non-idiopathic cases, lenke type 5 cases, and revision cases.
Clinical analysis
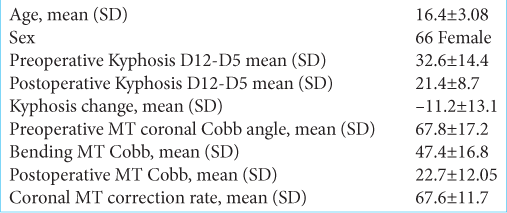
Eighty cases were included in the study. The mean patient age was 16.4 ± 3.08 years [
Out of 80 patients, half had PO. There were no statically significant differences between the two groups in age, sex, Lenke type, preoperative thoracic Cobb, postoperative coronal thoracic Cobb, and thoracic coronal Cobb in the bending view [
Intraoperative neural monitoring (IOM)
An IOM alert was considered significant, if there was a decrease of more than 50% of the motor or somatosensory signal. IOM alerts related to anesthesia, systemic causes, and technical neurophysiologic causes were not counted. Only cases that did not improve after the above-mentioned causes were counted.
Summary of surgical technique
All procedures were performed on a Jackson table using IONM Bilateral pedicle screws that were placed at all levels using a free hand technique.[
Statistical analysis
The two groups with and without PO were compared using the Student’s t-test and Fisher’s exact test, and results were confirmed by the nonparametric Mann–Whitney U-test. Data analysis was done using SPSS version 25.
RESULTS
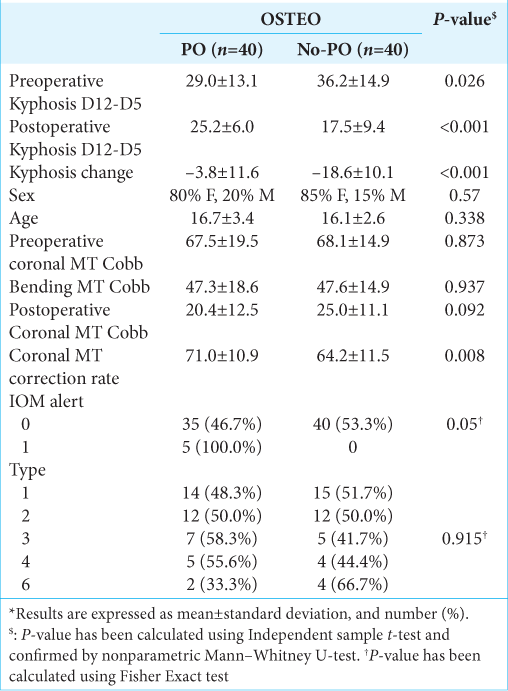
The correction rate was higher in the PO group: 71% ± 10.9 versus 64.2% ± 11.5 for the No-PO group [P = 0.008,
The preoperative T5–T12 kyphosis was smaller in the PO group: 29 ± 13.1 versus 36.2 ± 14.9 for the No-PO group [P = 0.026,
The postoperative kyphosis was higher in the PO group: 25.2 ± –6.0 versus 17.5 ± 9.4 for the No-PO group [P = 0.0001,
The kyphosis change was less in the PO group: –3.8 ± 11.6 versus –18.6 ± 10.1 for the No-PO group [P = 0.0001,
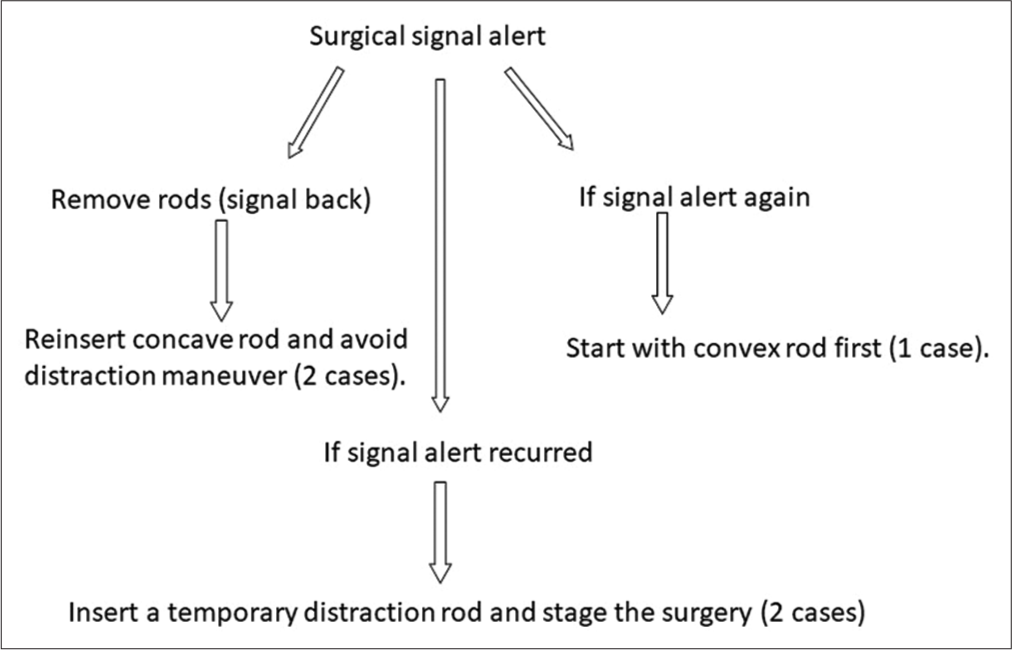
IOM alerts happened in five cases, all among the PO group [P = 0.02,
Advantages of PO accompanying AIS surgery
The 40 patients undergoing PO procedures with AIS surgery demonstrated a higher overall correction rate, a lesser degree of average change in postoperative kyphosis. However, five patients having PO during AIS surgery (12.5%) demonstrated significant intraoperative IOM changes versus none observed, where no PO were performed. Nevertheless, none of the five patients with such IOM changes during their AIS procedures ended up with new postoperative neurological deficits. [
DISCUSSION
Complication rates for PO used in AIS surgery
Although PO help in the 3D correction of the AIS deformity,[
Higher correction rate in PO patients undergoing AIS surgery
In a multicenter study of 191 subjects comparing PO and NoPO subjects, Samadani et al. 2015 showed a higher correction rate in the PO group (67.1% vs. 61.8%, P = 0.01). [
Better kyphosis outcomes with PO in AIS surgery
The kyphosis outcome was significantly better in the PO group (25.2 ± 6 vs. No-PO: 17.5 ± 9.4, P = 0.0001). We had a kyphosis decrease in both groups, which was more obvious in the PO group, where the kyphosis change was higher (-3.8 ± 11.6 vs. No-PO: -18.6 ± 10.1, P = 0.0001). This study showed the importance of good intraoperative neurophysiology monitoring during spinal deformity surgeries, especially when three-dimensional correction of the deformity is the goal.
CONCLUSION
In 40 patients, PO improved AIS correction in all planes, but increased the risk of IOM alerts in 5 (12.5%) of cases. Utilizing resuscitative techniques to address these alerts/ significant changes, we avoided postoperative neurological deficits in all five cases.
Declaration of the patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dickson RA, Lawton JO, Archer IA, Butt WP. The pathogenesis of idiopathic scoliosis. Biplanar spinal asymmetry. J Bone Joint Surg Br. 1984. 66: 8-15
2. Feng B, Qiu G, Shen J, Zhang J, Tian Y, Li S. Impact of multimodal intraoperative monitoring during surgery for spine deformity and potential risk factors for neurological monitoring changes. J Spinal Disord Tech. 2012. 25: E108-14
3. Hamilton DK, Smith JS, Sansur CA, Glassman SD, Ames CP, Berven SH. Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: A report of the scoliosis research society morbidity and mortality committee. Spine (Phila Pa 1976). 2011. 36: 1218-28
4. Imrie M, Yaszay B, Bastrom TP, Wenger DR, Newton PO. Adolescent idiopathic scoliosis: Should 100% correction be the goal?. J Pediatr Orthop. 2011. 31: S9-13
5. Nash CL, Lorig RA, Schatzinger LA, Brown RH. Spinal cord monitoring during operative treatment of the spine. Clin Orthop Relat Res. 1977. 126: 100-5
6. Samdani AF, Bennett JT, Singla AR, Marks MC, Pahys JM, Lonner BS. Do Ponte Osteotomies enhance correction in adolescent idiopathic scoliosis? An analysis of 191 Lenke 1A and 1B curves. Spine Deform. 2015. 3: 483-8
7. Shah SA, Dhawale AA, Oda JE, Yorgova P, Neiss GI, Holmes L. Ponte osteotomies with pedicle screw instrumentation in the treatment of adolescent idiopathic scoliosis. Spine Deform. 2013. 1: 196-204
8. Vauzelle C, Stagnara P, Jouvinroux P. Functional monitoring of spinal cord activity during spinal surgery. Clin Orthop Relat Res. 1973. 93: 173-8