- Department of Neurosurgery, Sawai Man Singh Medical College, Jaipur, Rajasthan, India,
- Department of Preventive and Social Medicine, Sawai Man Singh Medical College, Jaipur, Rajasthan, India.
Correspondence Address:
Mudit Mehrotra, Department of Neurosurgery, Sawai Man Singh Medical College, Jaipur, Rajasthan, India.
DOI:10.25259/SNI_998_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rashim Kataria1, Mudit Mehrotra1, Devendra Kumar Purohit1, Ajay Gupta2, Monika Rathore2. Prediction of the functional and radiological outcome on the basis of independent factors with special emphasis on the use of 3D printed models in craniovertebral junction surgery. 19-Aug-2022;13:369
How to cite this URL: Rashim Kataria1, Mudit Mehrotra1, Devendra Kumar Purohit1, Ajay Gupta2, Monika Rathore2. Prediction of the functional and radiological outcome on the basis of independent factors with special emphasis on the use of 3D printed models in craniovertebral junction surgery. 19-Aug-2022;13:369. Available from: https://surgicalneurologyint.com/surgicalint-articles/11808/
Abstract
Background: The aim of the study was to evaluate the advantage of performing planned surgery using customized three-dimensional (3D) printed models versus performing surgery without using 3D printed models in patients with craniovertebral junction (CVJ) anomalies and traumatic CVJ fractures and dislocations.
Methods: Forty-two patients with CVJ anomalies, who were planned for operative intervention in the Department of Neurosurgery at SMS Hospital from March 2019 to February 2021, were randomly divided into two groups and analyzed. First group was operated after rehearsal on a customized 3D printed model whereas the second group underwent operative intervention without the rehearsal of surgery on the 3D printed model.
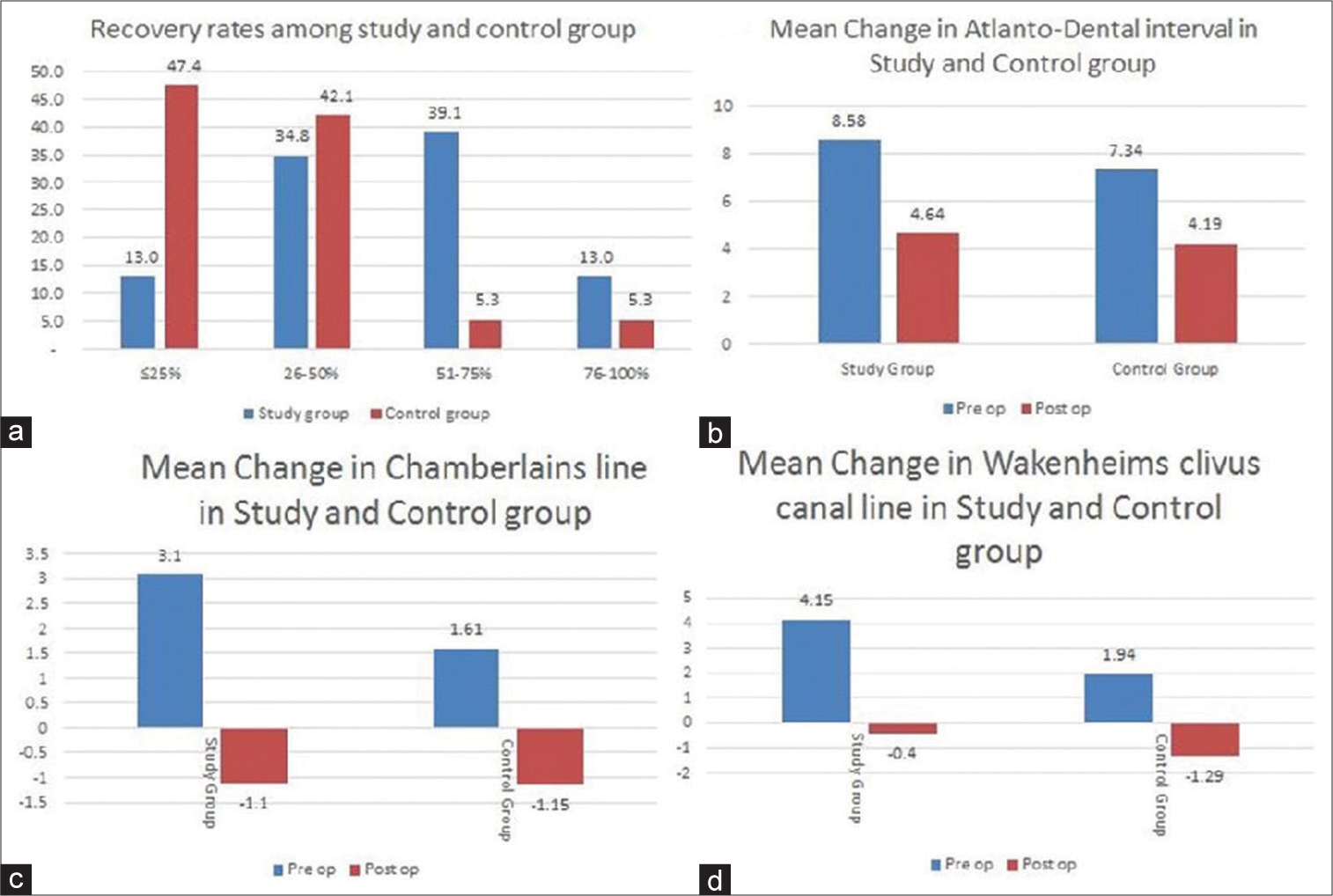
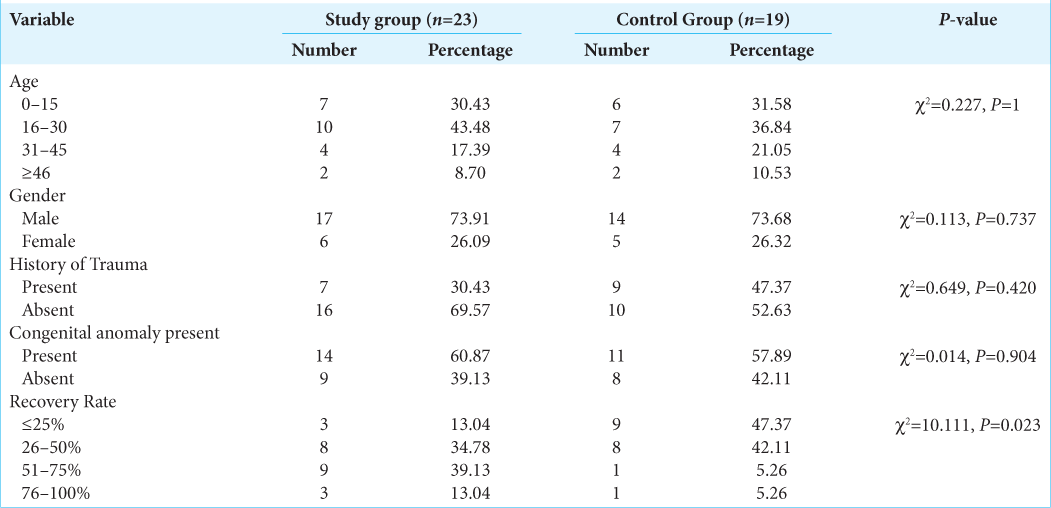
Results: Forty-two patients were enrolled for the study. Twenty-five of these patients had developmental CVJ anomalies, 16 had post traumatic Atlantoaxial dislocation (AAD), and one had congenital AAD. Twenty-three patients underwent surgical intervention using 3D printed models and 19 without using 3D printed models. The outcome in the two groups was compared using modified Japanese orthopedic association score (mJOA), recovery rate, incidence of complications such as screw malposition, postoperative neurological deterioration, vertebral artery (VA) injury, and radiological improvement based on Atlanto-Dental interval, the distance of the tip of dens from Wackhenheims clivus canal line, and the distance of tip of dens from the Chamberlain’s line. The improvement in mJOA score postoperatively was found to be statistically significant in study group (P P = 0.06). Recovery rate was better in study group than in control group (P = 0.023). In study group, the incidence of screw malposition and VA injury was lower than control group. Three patients deteriorated neurologically postoperatively in the control group and none in the study group. The average improvements in the radiological parameters were found to be better in study group as compared to control group postoperatively.
Conclusion: The authors conclude that 3D printed models are extremely helpful in analyzing joints and VA anatomy preoperatively and are helpful in unmasking any abnormal bony and vascular anatomy effectively, making the surgeon confident about the placement of the screws intraoperatively. These 3D models help in intraoperative error minimization with better neurological outcomes in postoperative period. In our opinion, these models should be included as a basic investigation tool in patients of CVJ abnormalities. The models also offer other advantages such as preoperative simulation, teaching modules, and patient education.
Keywords: 3D printed model, Atlantoaxial dislocation, Basilar invagination, Craniovertebral junction abnormality, Occiput–C2, C1–C2
INTRODUCTION
Craniovertebral junction (CVJ) is one of the most complex regions of the body to operate because of the limited space available for operation and unforgiving structures in the surrounding (e.g., the brain stem and vertebral artery [VA]). The course of the VA is often anomalous especially in congenital CVJ anomalies. The patient to patient variability in the size, angulation and orientation in the joints, facets and pedicle of the axis, and Atlas vertebra also adds to the complexity of this region. The use of sharp instruments and screws as well as high speed drills in this space-constrained environment makes the surgery difficult especially for a naive surgeon in this region. Surgery may lead to complications such as such as limb paralysis and VA injury leading to catastrophic hemorrhage causing life-threatening emergencies. The anatomy is further complicated by the presence of congenital osseous anomalies in this region. The risk of VA injury during CVJ surgery can be as high as 4.1%.[
MATERIALS AND METHODS
This prospective study was sanctioned by the ethical committee of Sawai Man Singh Medical College, and signed informed consent was taken from all patients. Forty-two patients (31 males and 11 females; mean age 24.39 ± 12.9 years for 23 cases and 28.11 ± 16.6 for 19 controls, ranging from 7 to 65 years; symptom duration 1 month – 5.5 years) with CVJ abnormalities who were admitted to our neurosurgery department between March 2019 and February 2021 were registered for the study. Clinical manifestations included neck pain (38 cases), weakness or incomplete paralysis (36 cases), posterior column involvement (30 cases), restricted neck movements (25 cases), bladder and bowel involvement (11 cases), dysphagia with dyspnea (six cases), and abnormalities in pain and temperature sensation (four cases).
Inclusion criteria
Patients presenting in outpatient neurosurgery department with CVJ anomalies planned for surgical intervention were included in the study.
Exclusion criteria
Patients presenting in emergency (those who required emergency surgeries) were excluded from the study.
Method and Materials
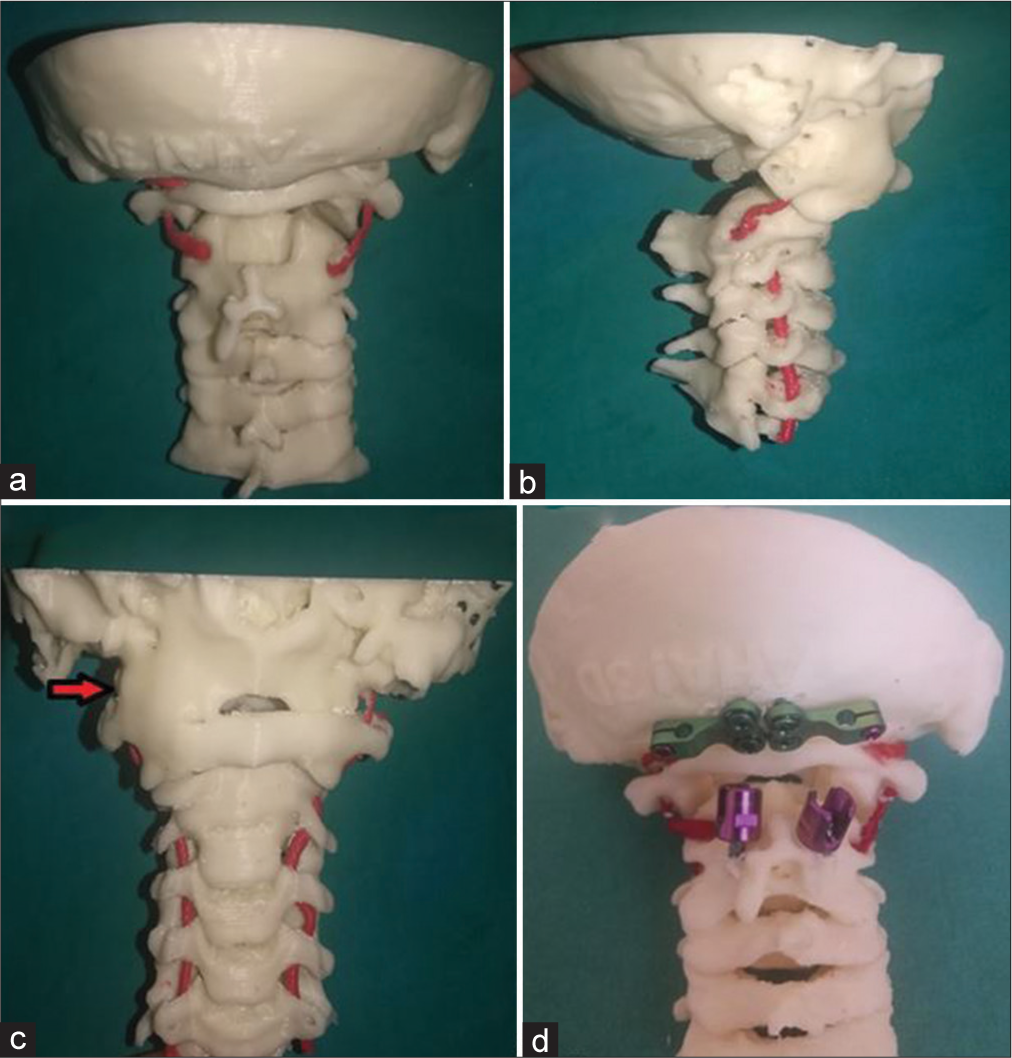
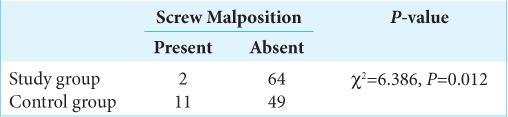
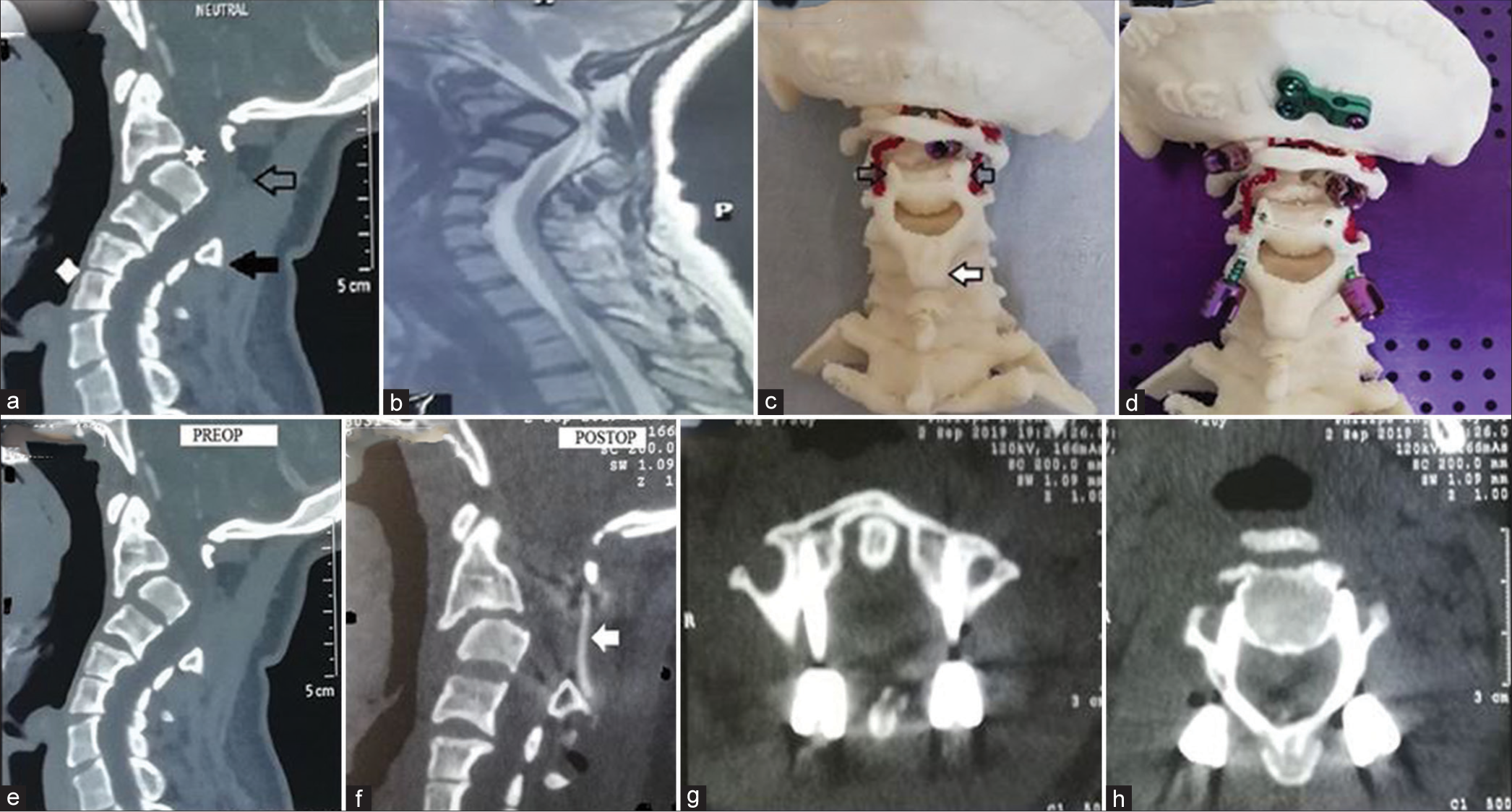
All patients underwent digital X-rays and computed tomography (CT) of the CVJ, CT angiography of the neck vessels, and magnetic resonance imaging (MRI) of the CVJ and cervical spine. 3D-assisted models of the CVJ along with VA were developed for 23 patients in the study groups and the remaining 19 patients were kept in control group, who underwent surgery with taking assistance from 3D models. The group allocation was done on random basis. The scans are obtained from a level extending from the occipital region up to the upper dorsal vertebra. 60 ml of iodinated contrast is injected IV at a rate of 4.5 ml/s. Axial 0.8-mm-thickCT images are obtained at 0.5-mm intervals. These data are in DICOM format. The angiography images of these patients are used to extract 3D file in Surface Tessellation Language (STL) format. This STL file was then sent electronically to a local laboratory with a 3D printer station for printing of 3D model [
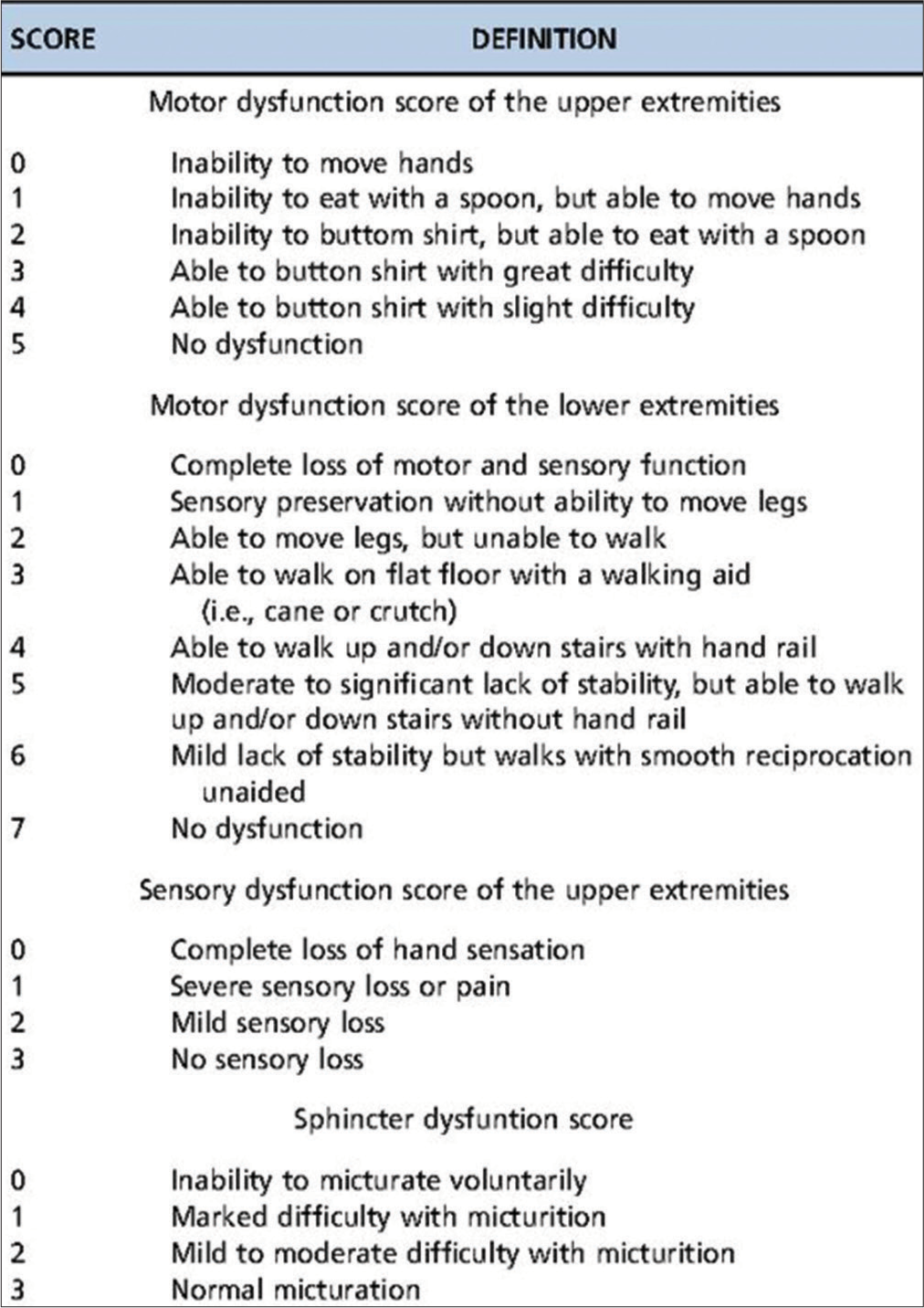
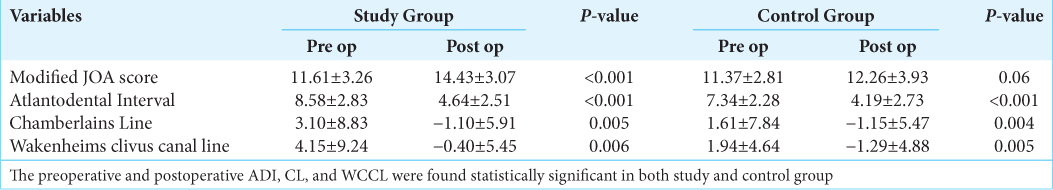
The preoperative and the postoperative values of the craniometric indices: Atlantodental interval (ADI), the distance of the tip of dens from Wackhenheims clivus canal line (WCCL), and finally the distance of tip of dens from the Chamberlain’s line (CL) were calculated in both the study and the control groups. The neurological assessment of patients in the preoperative and the postoperative period was done using the modified Japanese orthopedic association score (mJOA) using motor and sensory functions of the four extremities and the sphincter, which amounted to a total of 18 points [
Screw malposition was an important parameter compared between the two groups. Criteria used for deciding screw malposition were based on the radiological findings in postoperative CT scans and on the neurological status of the patient. The radiological criteria were any cortical breach of pedicle on medial side, cortical breach on lateral and inferior side of more than 2 mm, and finally cortical breach superiorly and anteriorly more than 4 mm. These criteria’s were established using McGill’s scoring system for revision of pedicle screws.[
The underlying principle of this surgery was neural decompression with stabilization of the CVJ complex. The posterior internal fixation surgery was done in each patient according to preoperative CT and MRI findings. In patients with Atlanto-occipital assimilation, internal fixation was performed using occipital plate and C2 pedicle screws, as first described by Olerud et al.[
The patients were followed up for a period of 1 year. Follow-up X-ray and CT of the neck were performed to investigate fusion maturation and bone growth at 1–3 months. Fusion was defined as presence bone trabeculae between the C1 and C2 facets without the presence of any gap. Cystic lucencies around the implants or along the endplates and linear defects within the bridging trabeculae suggested nonfusion.
Statistics
Data were entered into excel sheet. Continuous data were summarized in the form of mean and standard deviation. Difference in mean of two groups was analyzed using student “t” test. Discrete data were expressed in the form of proportions and difference in proportions was analyzed using Chi-square test. The level of significance was kept 95% for all statistical analysis.
RESULTS
Forty-three patients (31 males and 11 females) were enrolled for the study. Twenty-five of these patients had developmental CVJ anomalies, 16 presented as posttraumatic Atlantoaxial dislocation (AAD), and one had AAD with no history of trauma or developmental deformity. Twenty-three patients underwent surgical intervention using 3D printed models and 19 without using the aid of 3D printed models. The two groups were compared using mJOA, recovery rate, incidence of complications such as screw malposition, postoperative neurological deterioration, VA injury and radiological improvement based on ADI, CL, and WCCL.
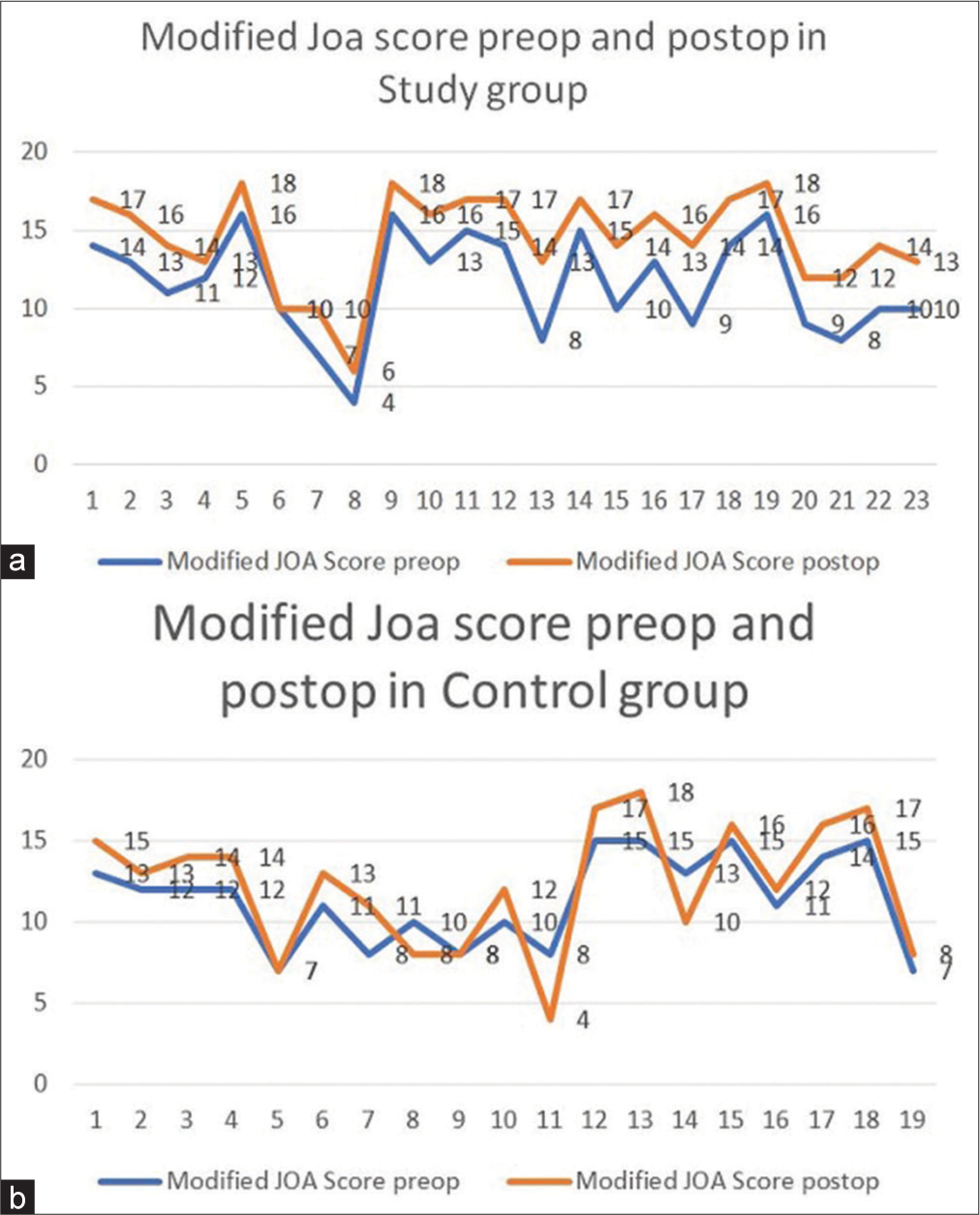
The improvement in modified JOA score postoperatively as compared to the preoperative score was found to be statistically significant in study group [
Figure 4:
(a) Comparision of recovery rates among study and control group, (b) mean change in atlanto-dental interval in study (3.94) versus control group (3.15), (c) mean change in canal line in study (4.2) versus control group (2.76), and (d) mean change in wackhenheims clivus canal line in study (4.55) versus control group (3.26).
After excluding the occipital screw and plate insertion in each patient in both study and control group, screw malposition was studied in both groups. It was observed that only two screws (out of 66 total inserted screws) were malpositioned in the study group (according to the McGill’s criteria), as compared to eleven screws (out of total 60 inserted screws) found to be malpositioned in the control group. This was found to be statistically significant (P = 0.012, i.e., <0.05) [
In the study group, almost all of the patients improved neurologically in the postoperative period as evident by their improved mJOA scoring. There was symptomatic improvement in neck pain and neck movements. There was no incidence of VA injury. One of our cases in study group had malpositioned C2 pedicle screw medially and did not improve neurologically in postoperative period, but there was no evidence of any neurological deterioration in this patient. The patient was advised for screw revision but the patient refused surgery. One of our pediatric patients had a single episode of Generealized Tonic-ClonicSeizures in the postoperative period, his CT scan brain showed no abnormality, and the patient was discharged without any neurological deficit. None of these patients had any implant failure requiring removal of the implant, wound-related complications, or cerebrospinal fluid leakage.
In the control group, out of 19 patients, eight patients showed screw malposition (using the McGills’s criteria). Four of these patients showed only minor improvement in their neurological status in postoperative period as depicted by their postoperative mJOA score and recovery rate. No improvement was seen in other two patients. Three patients deteriorated neurologically in the postoperative period of which one patient expired due to respiratory failure on 3rd postoperative day, his head CT was suggestive of brain stem and cerebellar infarction.
The results showed that posterior internal fixation performed using individualized 3D printed model is realistic and effective in treating CVJ abnormalities [
Figure 5:
Uncommon case of absent C2 posterior elements with C2-C3 spondyloptosis; (a) preoperative computed tomography (CT) scan (MidSagittal cut) showing absent C2 lamina (hollow arrow), C2-C3 spondyloptosis (asterix), hypertrophied spinous process of C3 (solid arrow), and C5-C6 block vertebra (diamond), (b) magnetic resonance imaging T2W image, midsagittal section showing severe cord compression by retropulsed C3 body, (c) 3D model of the craniovertebral junction of the patient showing posterior view with absent C2 lamina, well developed uncinate process of C3 (hollow arrow), and hypertrophied spinous process of C3 (solid arrow), (d) showing hands on practise on the model preoperatively, (e and f) comparison between the preoperative and postoperative CT scan (Mid Saggital view) of the patient showing acceptable reduction and realignment of the C2-C3 body with increased canal diameter at the level of C3 and iliac bone graft between C1 posterior arch and C3 spinous process in situ (solid arrow). The model helped us in better understanding of the complex anatomy and planning preoperatively, and (g and h) C1 lateral mass and C2 pedicle screw insertion.
DISCUSSION
The occipitoatlantal joint provides more stability in comparison to mobility and the reverse is true for the atlantoaxial joint, which offers more mobility leading to higher chances of injury and dislocation at this joint.[
The surgical management of AAD has seen a paradigm shift from transoral decompression followed by fixation to now more popular posterior fixation approaches using the screw-rod system, which includes pedicle screw system; lateral mass screws system, transarticular screws system, and laminar screws system. The most commonly used method of internal fixation for posterior cervical surgery is the pedicle screw system because of its excellent biomechanical property and the ease of surgery.[
The 3D reconstructed CT images are better than the 2D pictures and can help in understanding the complex anatomy but they are of limited use intraoperatively as they can be viewed only on a CT film and provide with only 2D prospective of the region concerned. The newer neuronavigation devices such as CT 3D navigation system, G-arm, and O-arm are able to serve the purpose of providing a 3D perspective of the region intraoperatively but the practical applications of these devices are limited by factors such as lack of equipment, insufficient training, and high costs.[
The 3D model can be used to practice the operation before the actual surgery, the size of the plates and screws to be used and the angle of insertion of the screws can be calculated preoperatively from these 3D models. The model also provides information about the overriding joints angulation, the size of the screwable structures such as pars, pedicle, lateral masses, and lamina. The entry points of the screws can be selected and the screws can be inserted in the model. This saves the operative time during the actual operation and also reduces the blood loss.[
Even though 3D printed models provide invaluable information but they have some limitations too. The most of the models are made of single material, that is, plastic (ABS), hence are brittle, they do not yield to the forces and manipulations (e.g., DCER) and break off; hence, the actual targeted correction of the deformity cannot be achieved in the model. The joints in the model are immobile and, hence, are unable to provide information with regard to the nature of the joint instability and flexibility. No information regarding the venous anatomy and the extent and size of venous plexus in the region of lateral gutters could be deciphered from the models. The model provides details about the osseous anatomy only and does not provide information on the strength and integrity of various ligaments and soft tissues. In redo cases, models with a single material are not able to distinguish between the bones and the implant.
CONCLUSION
Even though there are few shortcomings with 3D models, they provide with hands-on approach preoperatively and help immensely in decoding the complex anatomy of the CVJ which can help us in achieving a complication-free surgery in an otherwise complex region. This is even more relevant in cases of congenital CVJ anomalies where the anatomy is severely deranged and there are more chances of anomalous course of VA. The surgeon can have an excellent understanding of the anatomy by having hands on experience on the model. With further advances in the technology, it can be stated with reasonable surety that 3D printer will continue to prove itself as an important and highly cost-effective tool in the management of CVJ lesions.
Disclosures and acknowledgements
All authors of this research paper have directly participated in the planning, execution, and analysis of this study All authors of this paper have read and approved the final version submitted and each author believes that the manuscript represents honest work No conflict of interest relevant to this article was reported The content of this manuscript has not been copyrighted or published previously The content of this manuscript is not now under consideration for publication elsewhere The content of this manuscript will not be copyrighted, submitted, or published elsewhere, while acceptance by the journal is under consideration There are no directly related manuscripts published or unpublished by any authors of this paper My institute’s (SMS Medical College) representative is fully aware of this submission My research project was not sponsored by any agency.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976). 2000. 25: 962-9
2. Agarwal P, Chopra S, Sinha VD, Kataria R. Three-dimensional-printed model-assisted management of craniovertebral junction abnormalities: An institutional experience with literature review. Asian Spine J. 2020. 14: 204-11
3. Aoude A, Ghadakzadeh S, Alhamzah H, Fortin M, Jarzem P, Ouellet JA. Postoperative assessment of pedicle screws and management of breaches: A survey among Canadian spine surgeons and a new scoring system. Asian Spine J. 2018. 12: 37-46
4. Behari S, Kiran Kumar MV, Banerji D, Chhabra DK, Jain VK. Atlantoaxial dislocation associated with the maldevelopment of the posterior neural arch of axis causing compressive myelopathy. Neurol India. 2004. 52: 489-91
5. Chhabra S, Chopra S, Kataria R, Sinha VD. Use of 3D printer model to study vertebral artery anatomy and variations in developmental craniovertebral junction anomalies and as a preoperative tool-an institutional experience. J Spine Surg. 2017. 3: 572-9
6. Gao F, Wang Q, Liu C, Xiong B, Luo T. Individualized 3D printed model-assisted posterior screw fixation for the treatment of craniovertebral junction abnormality: A retrospective study. J Neurosurg Spine. 2017. 27: 29-34
7. Goel A, Jankharia B, Shah A, Sathe P. Three-dimensional models: An emerging investigational revolution for craniovertebral junction surgery. J Neurosurg Spine. 2016. 25: 740-4
8. Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). 1994. 129: 47-53
9. Goel A. Goel’s classification of atlantoaxial “facetal” dislocation. J Craniovertebr Junction Spine. 2014. 5: 3-8
10. Guo F, Dai J, Zhang J, Ma Y, Zhu G, Shen J. Individualized 3D printing navigation template for pedicle screw fixation in upper cervical spine. PLoS One. 2017. 12: e0171509
11. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001. 26: 2467-71
12. Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981. 6: 354-64
13. Izatt MT, Thorpe PL, Thompson RG, D’Urso PS, Adam CJ, Earwaker JW. The use of physical biomodelling in complex spinal surgery. Eur Spine J. 2007. 16: 1507-18
14. Jain VK, Behari S, Banerji D, Bhargava V, Chhabra DK. Transoral decompression for craniovertebral osseous anomalies: Perioperative management dilemmas. Neurol India. 1999. 47: 188-95
15. Jain VK, Behari S. Management of congenital atlanto-axial dislocation: Some lessons learnt. Neurol India. 2002. 50: 386-97
16. Kataria R, Mehrotra M, Purohit DK, Dharker N. Compressive myelopathy due to C2-C3 spondyloptosis as a consequence of absent C2 posterior elements: A rare case/review of literature. Interdiscip Neurosurg. 2020. 24: 101069
17. Kataria R, Verma PK, Sinha VD. Increasing the safety of surgical treatment for complex Cranio-vertebral anomalies using customized 3D printed models. J Clin Neurosci. 2017. 48: 203-208
18. Lang J. Craniocervical region, osteology and articulations. Neurolorthopedics. 1986. 1: 67-92
19. Magklara EP, Pantelia ET, Solia E, Panagouli E, Piagkou M, Mazarakis A. Vertebral artery variations revised: Origin, course, branches and embryonic development. Folia Morphol (Warsz). 2021. 80: 1-12
20. Menezes AH, VanGilder JC, Graf CJ, McDonnell DE. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980. 53: 444-55
21. Nordt JC, Stauffer ES. Sequelae of atlantoaxial stabilization in two patients with Down’s syndrome. Spine (Phila Pa 1976). 1981. 6: 437-40
22. Olerud C, Larsson BE, Rodriguez M. Subaxial cervical spine subluxation in rheumatoid arthritis. A retrospective analysis of 16 operated patients after 1-5 years. Acta Orthop Scand. 1997. 68: 109-15
23. Onishi E, Sekimoto Y, Fukumitsu R, Yamagata S, Matsushita M. Cerebral infarction due to an embolism after cervical pedicle screw fixation. Spine (Phila Pa 1976). 2010. 35: E63-6
24. Park JH, Roh SW, Rhim SC. A single-stage posterior approach with open reduction and pedicle screw fixation in subaxial cervical facet dislocations. J Neurosurg Spine. 2015. 23: 35-41
25. Passias PG, Wang S, Kozanek M, Wang S, Wang C. Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoxial dislocations. J Spinal Disord Tech. 2013. 26: 15-21
26. Salunke P, Behari S, Kirankumar MV, Sharma MS, Jaiswal AK, Jain VK. Pediatric congenital atlantoaxial dislocation: Differences between the irreducible and reducible varieties. J Neurosurg. 2006. 104: 115-22
27. Sardhara J, Behari S, Mohan BM, Jaiswal AK, Sahu RN, Srivastava A. Risk stratification of vertebral artery vulnerability during surgery for congenital atlanto-axial dislocation with or without an occipitalized atlas. Neurol India. 2015. 63: 382-91
28. Sobolewski BA, Mittiga MR, Reed JL. Atlantoaxial rotary subluxation after minor trauma. Pediatr Emerg Care. 2008. 24: 852-6
29. Sugimoto Y, Tanaka M, Nakahara R, Misawa H, Kunisada T, Ozaki T. Surgical treatment for congenital kyphosis correction using both spinal navigation and a 3-dimensional model. Acta Med Okayama. 2012. 66: 499-502
30. Tetreault L, Kopjar B, Nouri A, Arnold P, Barbagallo G, Bartels R. The modified Japanese orthopaedic association scale: Establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J. 2017. 26: 78-84
31. Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation: Technical description and report of 57 cases. Spine (Phila Pa 1976). 2007. 32: 643-6
32. Wang C, Yan M, Zhou HT, Wang SL, Dang GT. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine (Phila Pa 1976). 2006. 31: E306-13
33. Wang YT, Yang XJ, Yan B, Zeng TH, Qiu YY, Chen SJ. Clinical application of three-dimensional printing in the personalized treatment of complex spinal disorders. Chin J Traumatol. 2016. 19: 31-4
34. White AA, Panjabi MM. The clinical biomechanics of the occipitoatlantoaxial complex. Orthop Clin North Am. 1978. 9: 867-78
35. Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation: Results of a survey of the AANS/ CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998. 88: 634-40
36. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: Case series and technical note. J Spinal Disord Tech. 2004. 17: 158-62
37. Yang M, Zhang N, Shi H, Li H, Liu S, Song Z. Three-dimensional printed model-assisted screw installation in treating posterior atlantoaxial internal fixation. Sci Rep. 2018. 8: 11026
38. Yang YL, Zhou DS, He JL. Comparison of isocentric C-arm 3-dimensional navigation and conventional fluoroscopy for C1 lateral mass and C2 pedicle screw placement for atlantoaxial instability. J Spinal Disord Tech. 2013. 26: 127-34
39. Yin YH, Qiao GY, Yu XG, Tong HY, Zhang YZ. Posterior realignment of irreducible atlantoaxial dislocation with C1-C2 screw and rod system: A technique of direct reduction and fixation. Spine J. 2013. 13: 1864-71
40. Yu X, Li L, Wang P, Yin Y, Bu B, Zhou D. Intraoperative computed tomography with an integrated navigation system in stabilization surgery for complex craniovertebral junction malformation. J Spinal Disord Tech. 2014. 27: 245-52
41. Zhang K, Xu J, Wang Q, Wang G, Wu Z, Xia H. Treatment of dens fractures with posterior atlantoaxial dislocation with transoral atlantoaxial reduction plate surgery: Case report and introduction of a novel treatment option. Spine (Phila Pa 1976). 2012. 37: E451-5