- Department of Orthopaedics and Spine Surgery, Dr. B.A.M. Hospital, Mumbai, Maharashtra, India.
- Spine Services, KEM Hospital, Mumbai, Maharashtra, India.
- Department of Orthopaedics, ESIC Hospital, Mumbai, Maharashtra, India.
Correspondence Address:
Akash Shakya, Department of Orthopaedics and Spine Surgery, Dr. B.A.M. Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_1151_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Akash Shakya1, Ayush Sharma1, Vijay Singh1, Ajay Jaiswal1, Nandan Marathe2, Vinayak Garje3. Preoperative T1 magnetic resonance imaging changes carry a poor postoperative prognosis in cervical myelopathy: A retrospective study of 182 patients. 30-Dec-2021;12:629
How to cite this URL: Akash Shakya1, Ayush Sharma1, Vijay Singh1, Ajay Jaiswal1, Nandan Marathe2, Vinayak Garje3. Preoperative T1 magnetic resonance imaging changes carry a poor postoperative prognosis in cervical myelopathy: A retrospective study of 182 patients. 30-Dec-2021;12:629. Available from: https://surgicalneurologyint.com/surgicalint-articles/11311/
Abstract
Background: T2 scans are widely used to determine the prognosis for patients undergoing surgery for cervical myelopathy. In this study, we determined whether T1 MR changes in addition to T2 MR changes could have prognostic importance.
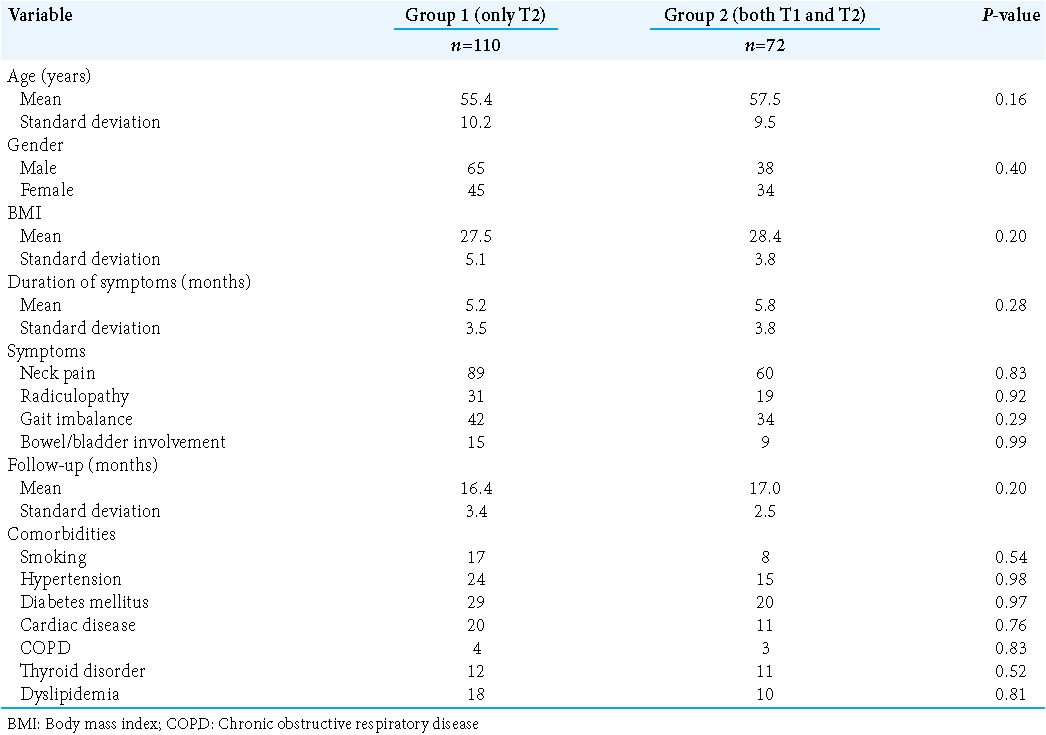
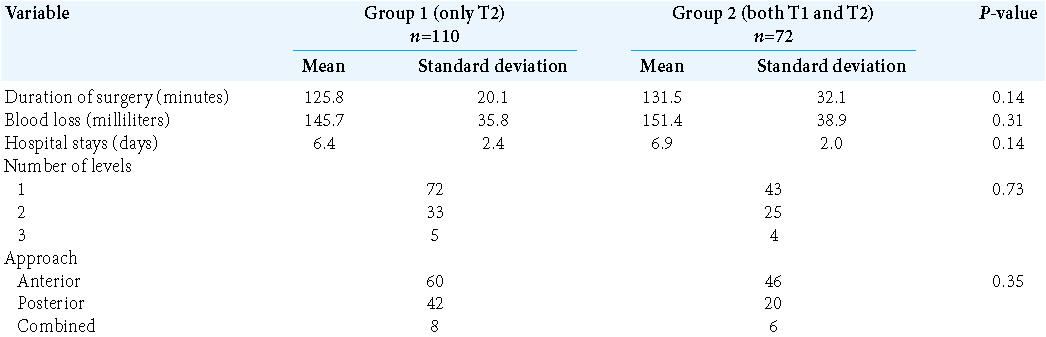
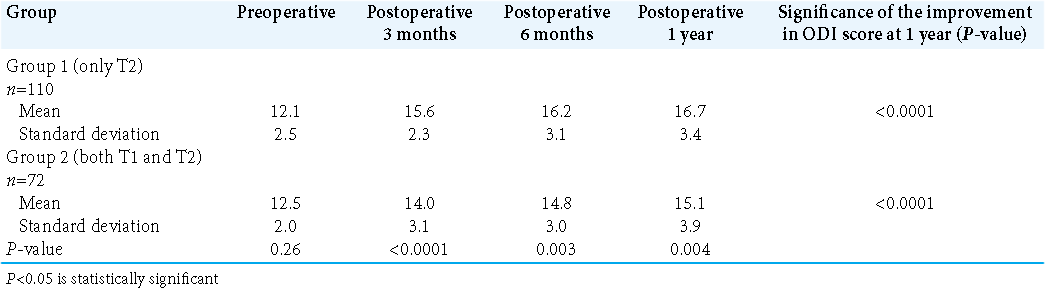
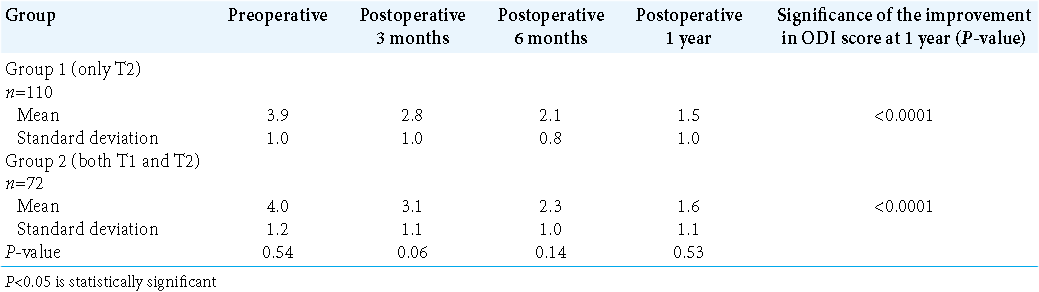
Methods: This retrospective analysis involved 182 patients undergoing surgery for cervical myelopathy (2017–2020). There were 110 patients in Group 1 (only T2 MR changes) and 72 in Group 2 (both T1 and T2 MR changes). In addition, demographic, visual analog score (VAS), modified Japanese Orthopaedic Association (mJOA) scores, and operative details were recorded at 1 month, 3 months, 6 months, and 1 year postoperatively.
Results: Notably, VAS scores were comparable at each point in time and were significantly better than the preoperative scores at 1 year postoperatively. Although mJOA scores were comparable at 1 month in both groups, they were better thereafter for Group 1 patients.
Conclusion: The presence of T1 changes on the preoperative magnetic resonance imaging represented a poor prognostic indicator for the postoperative outcome compared to the presence of T2 changes alone.
Keywords: Cervical myelopathy, Magnetic resonance imaging changes, Modified Japanese Orthopaedic Association, Prognostic, Visual analog score
INTRODUCTION
The prognostic impact of T1 MR findings in patients with myelopathy undergoing surgery needs to be further studied.[
MATERIALS AND METHODS
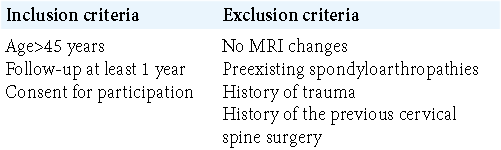
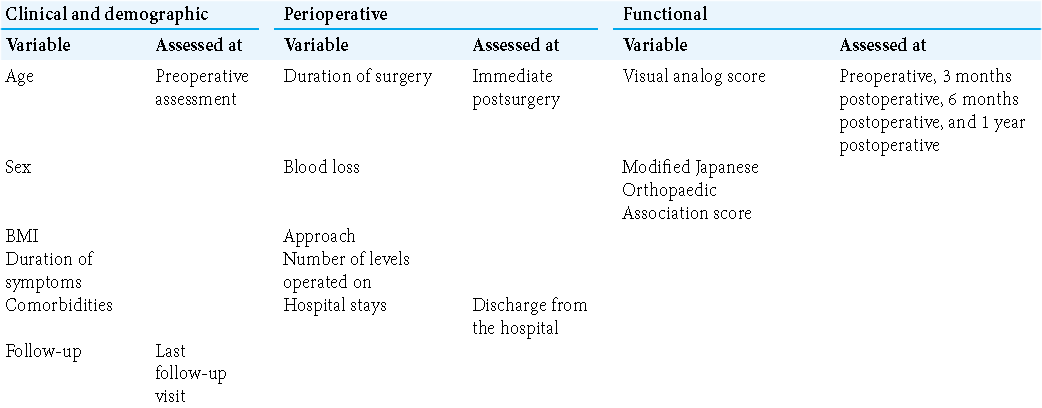
This retrospective analysis involved 182 patients undergoing cervical surgery for myelopathy (2017–2020) [
The criteria used in the study and the respective times of assessment are shown in [
Statistical analysis
The statistical analysis was performed using SPSS version 23.0. Paired Student’s t-test was used for statistical testing of difference in mean values for comparing between preoperative and postoperative outcomes. P = 0.05 was considered to be statistically significant. Pearson’s correlation was used to analyze the association between two variables. The analysis of variance test was used to analyze multiple variables. Values were reported as mean ± standard deviation of the mean.
RESULTS
The demographic, baseline characteristics, baseline functional scores, and operative were comparable for the two groups [
Visual analog score (VAS) was also comparable preoperatively. However, in contrast to the mJOA scores, the VAS was comparable among the two groups at each point of assessment postoperatively [
DISCUSSION
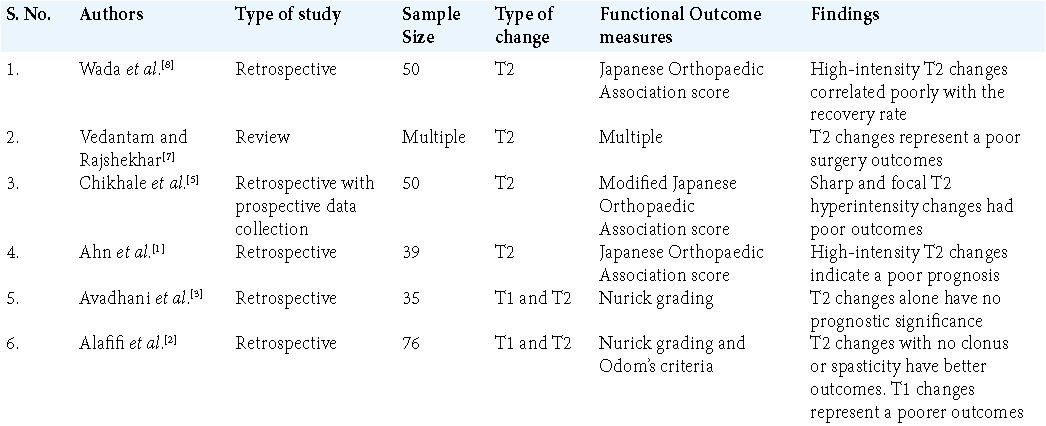
MRI and the wide and huge data that it provides have led to various prognostic factors being increasingly studied.[
Grading T2 changes
Grading of T2 changes on the MRI ranged from no change to mild with fuzzy borders, intense, and well-defined border of the hyperintensity in the cord,[
T1 cord changes on MRI
T1 changes have also been studied and have been shown to be independent predictors of functional outcomes. T1 changes most likely represent irreversible changes that occur in the cord and thus provide a better indication regarding prognosis after the surgery. T2 changes, typically due to cord edema, obstruction of the cerebrospinal fluid, degeneration of the gray matter, or myelomalacia, have a greater chance of being reversible. Thus, in the absence of T1 changes, T2 changes alone might represent an ideal window for intervention to prevent further and permanent deterioration.
Are T1 and T2 changes combined better predictors of outcome?
The combined T1 and T2 MR cord changes in patients with cervical myelopathy are more predictive of poorer outcomes.[
CONCLUSION
Both T1 and T2 MR changes constitute a poorer prognostic sign versus T2 changes alone for those about to undergo cervical spine surgery for myelopathy.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahn JS, Lee JK, Kim BK. Prognostic factors that affect the surgical outcome of the laminoplasty in cervical spondylotic myelopathy. Clin Orthop Surg. 2010. 2: 98-104
2. Alafifi T, Kern R, Fehlings M. Clinical and MRI predictors of outcome after surgical intervention for cervical spondylotic myelopathy. J Neuroimaging. 2007. 17: 315-22
3. Avadhani A, Rajasekaran S, Shetty AP. Comparison of prognostic value of different MRI classifications of signal intensity change in cervical spondylotic myelopathy. Spine J. 2010. 10: 475-85
4. Chen H, Pan J, Nisar M, Zeng HB, Dai LF, Lou C. The value of preoperative magnetic resonance imaging in predicting postoperative recovery in patients with cervical spondylosis myelopathy: A meta-analysis. Clinics (Sao Paulo Brazil). 2016. 71: 179-84
5. Chikhale CB, Khurjekar KS, Shyam AK, Sancheti PK. Correlation between preoperative magnetic resonance imaging signal intensity changes and clinical outcomes in patients surgically treated for cervical myeloradiculopathy. Asian Spine J. 2017. 11: 174-80
6. Suri A, Chabbra RP, Mehta VS, Gaikwad S, Pandey RM. Effect of intramedullary signal changes on the surgical outcome of patients with cervical spondylotic myelopathy. Spine J. 2003. 3: 33-45
7. Vedantam A, Rajshekhar V. Does the type of T2-weighted hyperintensity influence surgical outcome in patients with cervical spondylotic myelopathy? A review. Eur Spine J. 2013. 22: 96-106
8. Wada E, Yonenobu K, Suzuki S, Kanazawa A, Ochi T. Can intramedullary signal change on magnetic resonance imaging predict surgical outcome in cervical spondylotic myelopathy?. Spine. 1999. 24: 455-62
9. Yone K, Sakou T, Yanase M, Ijiri K. Preoperative and postoperative magnetic resonance image evaluations of the spinal cord in cervical myelopathy. Spine. 1992. 17: S388-92