- Skull Base Research Center, Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Correspondence Address:
Ehsan Nazari Maloumeh
Skull Base Research Center, Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
DOI:10.4103/sni.sni_247_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Omidvar Rezaee, Kaveh Ebrahimzadeh, Ehsan Nazari Maloumeh, Armin Jafari, Misagh Shafizad, Mohammad Hallajnejad. Prepontine arachnoid cyst presenting with headache and diplopia: A case report study. 06-Dec-2017;8:289
How to cite this URL: Omidvar Rezaee, Kaveh Ebrahimzadeh, Ehsan Nazari Maloumeh, Armin Jafari, Misagh Shafizad, Mohammad Hallajnejad. Prepontine arachnoid cyst presenting with headache and diplopia: A case report study. 06-Dec-2017;8:289. Available from: http://surgicalneurologyint.com/surgicalint-articles/prepontine-arachnoid-cyst-presenting-with-headache-and-diplopia-a-case-report-study/
Abstract
Background:Arachnoid cysts are found everywhere in cerebrospinal axis, most often in the middle cranial fossa. They are very rare in prepontine location.
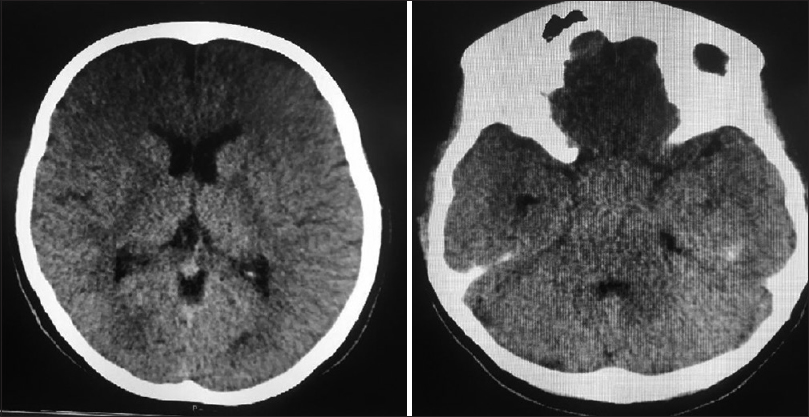
Case Description:In this study, we report a 26-year-old female presenting with a 3-month history of headache and diplopia. On physical examination, she had clinical manifestations of sixth cranial nerve palsy. Magnetic resonance imaging revealed a prepontine arachnoid cyst with extension into interpeduncular and suprasellar cisterns. Computed tomography scan demonstrated no evidence of hydrocephalus. The patient was treated surgically by endoscopic fenestration of the cyst with endonasal transsphenoidal approach. The cyst was opened to prepontine, interpeduncular, and suprasellar cisterns.
Conclusion:Endoscopic endonasal fenestration of the cyst to adjacent cistern may be safe in prepontine arachnoid cysts with sellar and suprasellar extension; it may be effective and less invasive compare to transcranial approach.
Keywords: Arachnoid cysts, diplopia, prepontine arachnoid cyst, retroclival arachnoid cyst, sixth cranial nerve palsy
INTRODUCTION
Arachnoid cysts are benign, fluid-filled, cyst-liked malformations related to the arachnoid mater.[
CASE REPORT
A 26-year-old female presented with a 3-month history of headache and diplopia. Gait problems, different types of seizures, and endocrine dysfunctions were not found. She had no history of any disease in the past. On physical examination, she had clinical manifestations of sixth cranial nerve palsy. Other neurological examinations were normal.
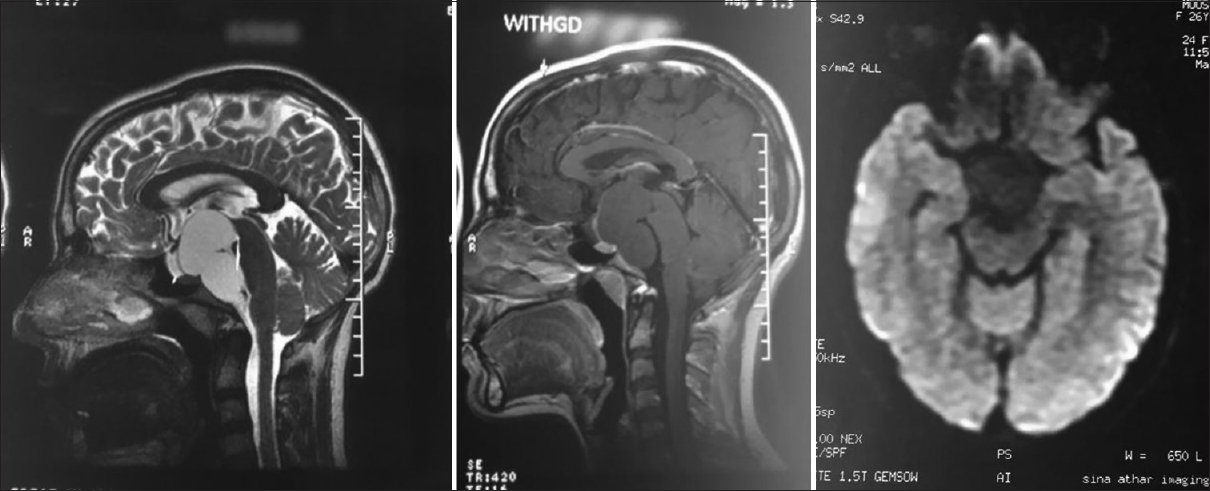
Magnetic resonance imaging (MRI) revealed a prepontine arachnoid cyst extending into the interpeduncular and suprasellar cisterns along with brainstem compression [
Figure 1
Preoperative magnetic resonance imaging. The T2-weighted sagittal image (left) shows a large hyperintense retroclival cystic mass extending into interpeduncular and suprasellar cisterns, causing compression and posterior displacement of brain stem. The T1-weighted postgadolinium sagittal image (middle) shows a nonenhancing mass. Diffusion weighted image (right) demonstrates a mass lesion in interpeduncular cistern without restricted pattern
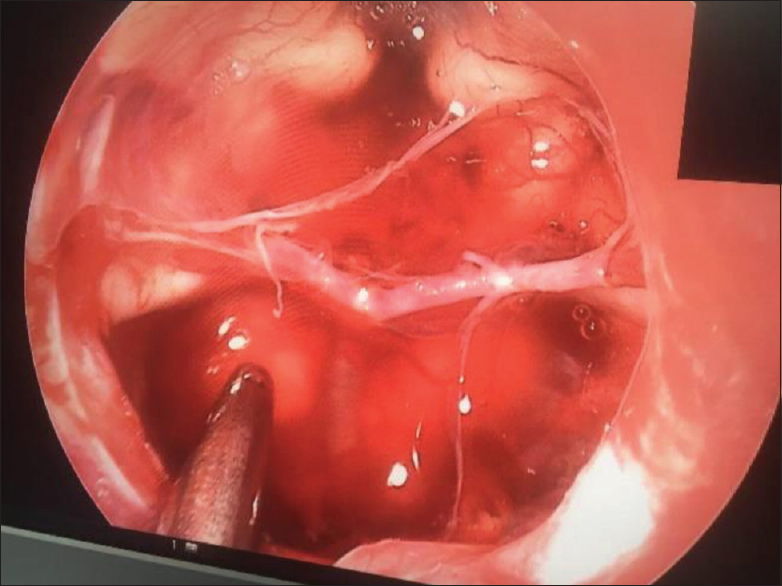
The patient was treated surgically by endoscopic fenestration of the cyst with endonasal transsphenoidal approach. The cyst was opened into the prepontine, interpeduncular, and suprasellar cisterns [
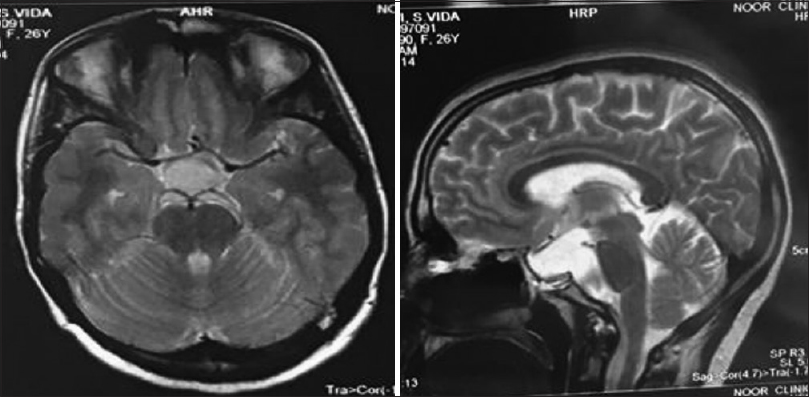
Postoperatively, she had impressive improvement in the function of sixth cranial nerve, and was discharged with no complications. Follow-up MRI showed a decrease in the size of the cyst and decompression of the adjacent tissues [
We reported this case due to rare occurrence of prepontine arachnoid cyst, nonclassic clinical manifestation in this case, and the different surgical approach that we adopted to treat the cyst. We discuss these concerns below.
DISCUSSION
Arachnoid cysts are benign, fluid-filled, cyst-liked malformations related to the arachnoid mater.[
Furthermore, there have been some case reports regarding the atypical presentations of arachnoid cyst. In 1992, Bourekas et al. reported a case of a 54-year-old woman who presented with a 6-month history of ataxia, quadraparesis, headaches, intermittent slurred speech, and urinary incontinence. She was also suffering from a progressive 10-year history of decreasing hearing in the right ear. MRI revealed a large extra-axial retroclival mass extending from the posterior suprasellar region into the upper cervical spinal canal and into both CPAs, right being greater than left. Compression and posterior displacement of the brainstem was noted. She was treated surgically by fenestration of the cyst through a right retromastoid craniectomy and C1 laminectomy.[
In 2008, De Bonis et al. reported a case of a 64-year-old man with a clinical history of gait disturbance and urge incontinence. Radiologic studies showed evidence of a supratentorial normal pressure hydrocephalus, with enlarged pericephalic spaces caused by a 4-cm prepontine arachnoid cyst.[
In 2008, Bonde et al. presented a 26-year-old woman with a 10-year history of right hemifacial spasm controlled by botulinum injections. On examination, she had right sensorineural hearing loss, right hemifacial spasm and ataxia. MRI showed a retroclival cyst vertically extending all the way from the suprasellar region, over the clivus up to the level of the body of the axis. It also extended into the both cerebellopontine angles, more on the right side. She underwent retrosigmoid craniectomy in the sitting position and wide marsupialization of the cyst was performed.[
In 2009, Akyuz et al. reported a case of a 40-year-old woman who had a sudden onset of occipitocervical pain and vomiting for a week. MRI revealed a retroclival cystic lesion complicated with intracystic hemorrhage. The cystic lesion was treated surgically by a right lateral suboccipital approach.[
In 2014, Rao et al. reported a case of 9-year-old boy with a history of precocious puberty of several months. MRI revealed a giant 51 × 52 × 52-mm well-circumscribed suprasellar arachnoid cyst. They concluded that suprasellar arachnoid cysts may present with endocrinopathies months to years prior to development of visual symptoms.[
In 2015, Ramesh et al. presented three cases with bobble-head doll syndrome (anteroposterior bobbling of the head and neck on the trunk every 2–3 seconds) associated with a large suprasellar arachnoid cyst and obstructive hydrocephalus, which were treated with endoscopic cystoventriculocisternostomy and marsupialization of the cyst.[
Our patient presented with unilateral (left) abducens nerve palsy reported for the first time as a clinical manifestation of arachnoid cysts. Although arachnoid cysts are often described as cystic masses with a MRI signal intensity similar to CSF on all sequences, such as T1-weighted, T2- weighted, and diffusion-weighted images, the cyst in our patient was isointense on T1-weighted, hyperintense on T2-weighted and nonrestricted on diffusion-weighted sequences. We could not locate any such case in the literature. The fluid of an uncomplicated arachnoid cyst without intracystic hemorrhage or infection is indistinguishable from CSF (low protein), thus the intensity of the cyst fluid is similar to CSF on all MRI sequences. Neoplastic, inflammatory, and hemorrhagic cysts (complicated cysts) have a greater amount of protein and cellular debris resulting in different intensities compared to CSF on at least one sequence.[
CONCLUSION
For patients presenting with headache or other neurological symptoms who have occupying lesions in suprasellar and prepontine or retroclival locations in further evaluation, arachnoid cysts should be considered as a differential diagnosis which can be only followed up in asymptomatic cases because of their benign nature; whereas in symptomatic cases, different surgical methods can be considered as the most effective treatment. In prepontine arachnoid cysts with sellar and suprasellar extension, endoscopic endonasal fenestration of the cyst to adjacent cistern may be safe, effective, and less invasive compared to the transcranial approach.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank the Clinical Research Development Unit(CRDU) of Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran for their support, cooperation and assistance throughout the period of study.
References
1. Al-Holou WN, Terman S, Kilburg C, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in adults. J Neurosurg. 2013. 118: 222-31
2. Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in children. J Neurosurg. 2010. 5: 578-85
3. Akyuz M, Goksu E, Aralasmak A, Tuncer R. Retroclival arachnoid cyst presenting with haemorrhage: A brief report of a special case. Acta Neurochir. 2010. 152: 161-2
4. Bayrakli F, Okten AI, Kartal U, Menekse G, Guzel A, Oztoprak I. Intracranial arachnoid cyst family with autosomal recessive trait mapped to chromosome 6q22. Acta Neurochir. 2012. 1: 1287-92
5. Behrens P, Ostertag CB. Zystische Fehlbildungen des Gehirns: Stereotaktische Diagnostik und Therapie. Nervenarzt. 1992. 63: 725-30
6. Bourekas EC, Raji MR, Dastur KJ, Francken GJ, Engle DJ, Nayak NT. Retroclival arachnoid cyst. Am J Neuroradiol. 1992. 13: 353-4
7. Bonde V, Muzumdar D, Goel A. Retroclival arachnoid cyst with hemifacial spasm. Singapore Med J. 2008. 49: 281-2
8. Contreras C, Copty M, Langelier R, Gagne F. Traumatic suprasellar arachnoid cyst. Surg Neurol. 1977. 8: 196-8
9. Clemenceau S, Carpentier A. Intracranial arachnoid cysts. Rev Neurol. 1999. 155: 604-8
10. Cilluffo JM, Onofrio BM, Miller RH. The diagnosis and surgical treatment of intracranial arachnoid cysts. Acta Neurochir. 1983. 67: 215-29
11. De Bonis P, Novegno F, Tamburrini G, Anile C, Pompucci A, Mangiola A. Teaching NeuroImage: Prepontine-suprasellar arachnoid cyst presenting with signs of normal pressure hydrocephalus. Neurology. 2008. 70: e26-
12. Helland CA, Lund-Johansen M, Wester K. Location, sidedness, and sex distribution of intracranial arachnoid cysts in a population-based sample. J Neurosurg. 2010. 113: 934-9
13. Helland CA, Wester K. Intracystic pressure in patients with temporal arachnoid cysts: A prospective study of preoperative complaints and postoperative outcome. J Neurol Neurosurg Psychiatry. 2007. 78: 620-3
14. Helland CA, Wester K. A population based study of intracranial arachnoid cysts: Clinical and neuroimaging outcomes following surgical cyst decompression in adults. J Neurol Neurosurg Psychiatry. 2007. 78: 1129-35
15. Heier LA, Zimmerman RD, Amster JL, Gandy SE, Deck MD. Magnetic resonance imaging of arachnoid cysts. Clin Imaging. 1989. 13: 281-91
16. Ivan ME, Iorgulescu JB, El-Sayed I, McDermott MW, Parsa AT, Pletcher SD. Risk factors for postoperative cerebrospinal fluid leak and meningitis after expanded endoscopic endonasal surgery. J Clin Neurosci. 2015. 22: 48-54
17. Lange M, Oeckler R. Results of surgical treatment in patients with arachnoid cysts. Acta Neurochir. 1987. 1: 99-104
18. Mørkve SH, Helland CA, Aßmus J, Lund-Johansen M, Wester KG. Surgical decompression of arachnoid cysts leads to improved quality of life: A prospective study. Neurosurgery. 2015. 78: 613-25
19. Oertel JM, Wagner W, Mondorf Y, Baldauf J, Schroeder HW, Gaab MR. Endoscopic treatment of arachnoid cysts: A detailed account of surgical techniques and results. Neurosurgery. 2010. 67: 824-36
20. Rengachary SS, Kennedy JD. Intracranial arachnoid and ependymal cysts. Neurosurgery. 1985. 3: 2160-72
21. Rengachary SS, Watanabe I. Ultrastructure and pathogenesis of intracranial arachnoid cysts. J Neuropathol Exp Neurol. 1981. 40: 61-83
22. Rousseaux M, Lesoin F, Dhellemmes P, Jomin M. Retroclival cysts. Neurochirurgia. 1986. 29: 244-7
23. Rao K, Levy ML, Crawford JR. Giant suprasellar arachnoid cyst presenting with precocious puberty. BMJ Case Rep. 2014. p. 1-2
24. Ramesh S, Raju S. Suprasellar arachnoid cyst presenting with bobble-head doll syndrome: Report of three cases. J Pediatr Neurosci. 2015. 10: 18-
25. Van Tassel P, Curé JK. Nonneoplastic intracranial cysts and cystic lesions. Semin Ultrasound CT MR. 1995. 16: 186-211
26. Van der Meche FG, Braakman R. Arachnoid cysts in the middle cranial fossa: Cause and treatment of progressive and non-progressive symptoms. J Neurol Neurosurg Psychiatry. 1983. 46: 1102-7
27. Wester K. Peculiarities of intracranial arachnoid cysts: Location, sidedness, and sex distribution in 126 consecutive patients. Neurosurgery. 1999. 45: 775-9
28. Westermaier T, Schweitzer T, Ernestus RI. Arachnoid cysts. Adv Exp Med Biol. 2012. 724: 37-50
29. Yamakawa H, Ohkuma A, Hattori T, Niikawa S, Kobayashi H. Primary intracranial arachnoid cyst in the elderly: A survey on 39 cases. Acta Neurochir. 1991. 113: 42-7