- Department of Neurosurgery, Naresuan University, Phitsanulok, Thailand.
- Department of Radiology, Naresuan University, Phitsanulok, Thailand.
Correspondence Address:
Jiroje Jiranukool
Department of Radiology, Naresuan University, Phitsanulok, Thailand.
DOI:10.25259/SNI_506_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jiroje Jiranukool1, Peeraphong Thiarawat1, Waneerat Galassi2. Prevalence of intracranial aneurysms among acute ischemic stroke patients. 15-Oct-2020;11:341
How to cite this URL: Jiroje Jiranukool1, Peeraphong Thiarawat1, Waneerat Galassi2. Prevalence of intracranial aneurysms among acute ischemic stroke patients. 15-Oct-2020;11:341. Available from: https://surgicalneurologyint.com/surgicalint-articles/10328/
Abstract
Background: The prevalence of unruptured intracranial aneurysms varies with age, sex, and genetic diseases, including atherosclerotic diseases. The objectives of this study are to determine the prevalence of intracranial aneurysms among acute ischemic stroke patients and the clinical outcomes of the patients.
Methods: The authors included patients with acute ischemic stroke within 7 days of onset. Demographic data, stroke subtypes, risk factors, and modified Rankin scale (mRS) scores at 6 months after stroke were collected. Magnetic resonance angiography was performed to diagnose intracranial aneurysms. The occurrence of aneurysmal subarachnoid hemorrhage (aSAH) was recorded during the follow-up at 6 months.
Results: Thirteen (7%) of the 186 patients were found to have incidental intracranial aneurysms. Age and sex were not different between the patients with and without aneurysms (P > 0.999, P > 0.999). Ten patients (76.9%) had a saccular aneurysm. The most common site of the aneurysm was the cavernous part of the internal carotid artery (n = 6). Nine patients (69.2%) had very small (P = 0.665).
Conclusion: A higher prevalence of intracranial aneurysms was observed among acute ischemic stroke patients than among the general population. However, the variability of the general population should be considered. The functional outcomes of acute ischemic stroke patients are not affected by the presence of an intracranial aneurysm.
Keywords: Acute ischemic stroke, Intracranial aneurysms, Prevalence
INTRODUCTION
Ruptured intracranial aneurysm is a serious condition with high morbidity and mortality. In the modern era, the detection of unruptured intracranial aneurysms is increasing due to the high quality and higher frequency of cerebral vascular imaging. According to a systematic review and meta-analysis, the overall prevalence of unruptured intracranial saccular aneurysms is 3–3.2%.[
MATERIALS AND METHODS
This study was a descriptive study. The authors included patients diagnosed with acute ischemic stroke within 7 days of onset or with the transient ischemic attack. The patients were admitted to our institutions between July 2012 and December 2017, and magnetic resonance angiography (MRA) was performed to assess the cerebral vessels. Brain MRI and MRA were performed with a 1.5T MR scanner (Ingenia 1.5T, Philips Medical Systems). MRA was performed using an intravenous injection of contrast, and then, the cerebral vessels were reconstructed into three dimensions. The MRI and MRA data of all patients were reviewed by one experienced neuroradiologist. Demographic data, stroke subtypes according to the modified Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification,[
Descriptive statistics (the mean, median, and standard deviation) were used for demographic data. Fisher’s exact test was used to identify between-group differences among the factors related to the presence of unruptured intracranial aneurysms.
RESULTS
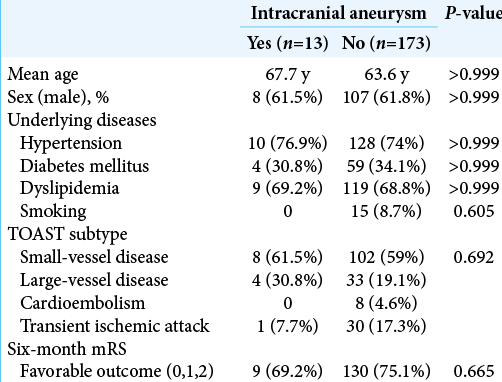
One hundred ninety-one acute ischemic stroke patients were admitted and underwent MRI/MRA. Five patients were excluded due to incomplete data. Of a total of 186 patients, 13 (7%) were found to have incidental intracranial aneurysms. All intracranial aneurysm patients were diagnosed by MRA. The demographic data are shown in [
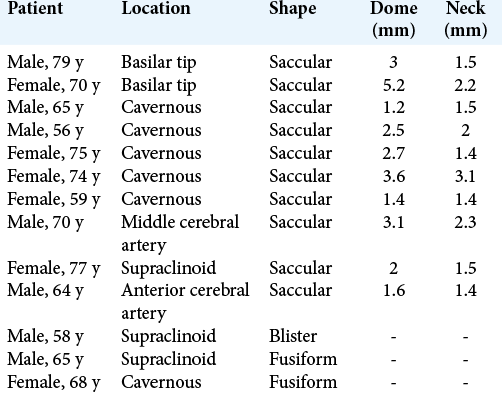
Ten patients had a saccular aneurysm, two patients had a fusiform aneurysm, and one patient had a blister aneurysm. No thrombosed aneurysm related to ischemic stroke was identified. The most common location of the incidental intracranial aneurysms was the cavernous part of the internal carotid artery (n = 6), followed by the supraclinoid part of the internal carotid artery (n = 3), basilar tip artery (n = 2), middle cerebral artery (n = 1), and anterior cerebral artery (n = 1). The size of the neck aneurysms ranged from 1.4 to 3.1 mm, and the dome of the aneurysm ranged from 1.2 to 5.2 mm. Nine patients had very small (<4 mm) aneurysms. All aneurysm data are shown in [
After 6 months of follow-up, no aSAH occurred. The patients with aneurysms are still stable, and neurological deficits related to the aneurysms have not been found. Moreover, no patient underwent surgical or interventional treatment for 6 months. Regarding favorable outcomes according to mRS scores at 6th months, no difference was found between the patients with aneurysms and those without aneurysms (9/13 [69.2%] vs. 130/173 [75.1%], P = 0.665).
DISCUSSION
This is the first study to report the prevalence of unruptured intracranial aneurysms among acute ischemic stroke patients in Thailand. The prevalence of unruptured intracranial aneurysms is approximately 3–3.2%.[
In our study, a high proportion of the patients with unruptured intracranial aneurysms had large-vessel disease, possibly because the pathology of large-vessel disease is atherosclerosis. Atherosclerosis can change the morphology of arterial vessels, leading to weakened vessel walls, dilation, and aneurysmal formation.[
According to the international study of unruptured intracranial aneurysms, the natural history of unruptured intracranial aneurysms depends on the size and location of the aneurysm. Aneurysms <7 mm in size have 5-year cumulative rupture rates of approximately 0–2.5%, and cavernous carotid artery aneurysms have the lowest rates of rupture.[
The limitations of this study include the single-center study design and the small number of patients. The study population cannot represent the general Thai population. In addition, no healthy control group was established. Second, the patients with aneurysms were diagnosed by MRA alone, which can have a high false-positive rate. Four-vessel conventional cerebral angiography, which is the gold standard, was not performed to confirm the diagnosis in all patients. Third, the films were analyzed by only one neuroradiologist. Fourth, the intracranial aneurysm patients did not undergo investigations for genetic diseases, which might be a confounding factor.
CONCLUSION
The prevalence of incidental unruptured intracranial aneurysms among acute ischemic patients in a single center in Thailand is 7%, which seems higher than that in the general population, although differences in the baseline characteristics of the population and confounding by indication for screening should be considered. No rupture of the unruptured intracranial aneurysms was observed during the 6-month follow-up period. Functional outcomes did not differ between the patients with and without aneurysms.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge the stroke unit team and the department of radiology for data collection.
References
1. Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial, TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993. 24: 35-41
2. Brown RD, Broderick JP. Unruptured intracranial aneurysms: Epidemiology, natural history, management options, and familial screening. Lancet Neurol. 2014. 13: 393-404
3. Da Costa LB, Gunnarsson T, Wallace MC. Unruptured intracranial aneurysms: Natural history and management decisions. Neurosurg Focus. 2004. 17: E6
4. Etminan N, Rinkel GJ. Unruptured intracranial aneurysms: Development, rupture and preventive management. Nat Rev Neurol. 2016. 12: 699-713
5. Griffiths PD, Worthy S, Gholkar A. Incidental intracranial vascular pathology in patients investigated for carotid stenosis. Neuroradiology. 1996. 38: 25-30
6. Hokari M, Isobe M, Imai T, Chiba Y, Iwamoto N, Isu T. The impact of atherosclerotic factors on cerebral aneurysm is location dependent: Aneurysms in stroke patients and healthy controls. J Stroke Cerebrovasc Dis. 2014. 23: 2301-7
7. Ishikawa Y, Hirayama T, Nakamura Y, Ikeda K. Incidental cerebral aneurysms in acute stroke patients: Comparison of asymptomatic healthy controls. J Neurol Sci. 2010. 298: 42-5
8. Oh YS, Lee SJ, Shon YM, Yang DW, Kim BS, Cho AH. Incidental unruptured intracranial aneurysms in patients with acute ischemic stroke. Cerebrovasc Dis. 2008. 26: 650-3
9. Shiue I, Arima H, Hankey GJ, Anderson CS, Group A. Modifiable lifestyle behaviours account for most cases of subarachnoid haemorrhage: A population-based case-control study in Australasia. J Neurol Sci. 2012. 313: 92-4
10. Thien A, See AA, Ang SY, Primalani NK, Lim MJ, Ng YP. Prevalence of asymptomatic unruptured intracranial aneurysms in a Southeast Asian population. World Neurosurg. 2017. 97: 326-32
11. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 2011. 10: 626-36
12. Wiebers DO, Whisnant JP, Huston J, Meissner I, Brown RD, Piepgras DG. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003. 362: 103-10
13. Zheng Y, Zhou B, Wang X, Chen H, Fang X, Jiang P. Size, aspect ratio and anatomic location of ruptured intracranial aneurysms: Consecutive series of 415 patients from a prospective, multicenter, observational study. Cell Transplant. 2019. 28: 739-46