- Department of Neurosurgery, Medical School, University of the Witwatersrand, Johannesburg, Gauteng, South Africa.
DOI:10.25259/SNI_309_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: John Ouma. Primary empty sella syndrome associated with visual deterioration salvaged by chiasmapexy: Report of a case and discussion of the literature. 21-Mar-2020;11:48
How to cite this URL: John Ouma. Primary empty sella syndrome associated with visual deterioration salvaged by chiasmapexy: Report of a case and discussion of the literature. 21-Mar-2020;11:48. Available from: https://surgicalneurologyint.com/surgicalint-articles/9921/
Abstract
Background: Empty sella syndrome (ESS) is a condition in which there is loss of volume of the pituitary gland, which is the normal constituent of the sella turcica. There may be visual and endocrine deficits associated with this condition, and radiologically, there may be downward prolapse of the optic chiasm. It occurs in a primary ESS, poorly understood form, as well as a secondary ESS form that follows medical or surgical treatment of a pituitary macroadenoma, or else spontaneous hemorrhage into such a tumor.
Case Description: A 56-year-old man presenting with deficits of both visual acuity and visual fields in the setting of radiological ESS without associated optic chiasm prolapse is discussed. He underwent endoscopic endonasal chiasmapexy with gradual improvement of his visual function over the following 6 months.
Conclusion: ESS is a potentially potent cause of visual deterioration that lends itself to reversal through a relatively simple neurosurgical technique. This case illustrates that actual prolapse of the chiasm is neither a prerequisite for visual deterioration nor its reversal the mechanism of visual improvement after chiasmapexy, raising the question of the mechanisms at play in cases such as this. It confirms the role of chiasmapexy in the management of selected cases of ESS.
Keywords: Chiasmapexy, Empty sella syndrome, Vision
INTRODUCTION
This paper seeks to draw attention to the entity of empty sella syndrome, how it might present with visual deterioration and how that can be improved through a simple surgical technique.
CASE DESCRIPTION
A 56-year-old man with no chronic or comorbid conditions presented with deterioration of vision, mainly in respect of visual fields but also visual acuity over a period of 9 months. He had been using prescription eyeglasses over the past couple of decades, but his situation was not helped by two alterations of their power.
He had no constitutional symptoms of note.
Clinical examination was noteworthy for early bilateral optic atrophy associated with bitemporal hemianopia and diminished visual acuity (left 6/12, right 6/18) when corrected with eyeglasses.
The remainder of the neurological and systemic examination was unremarkable.
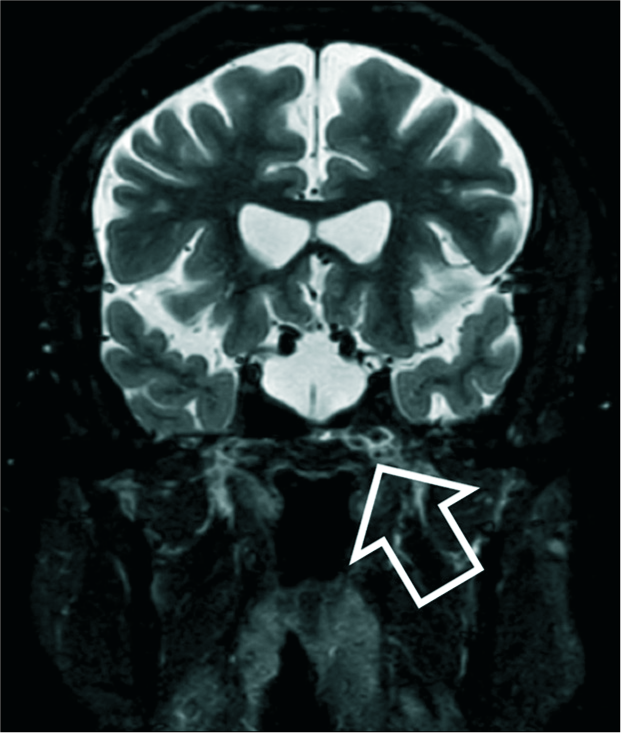
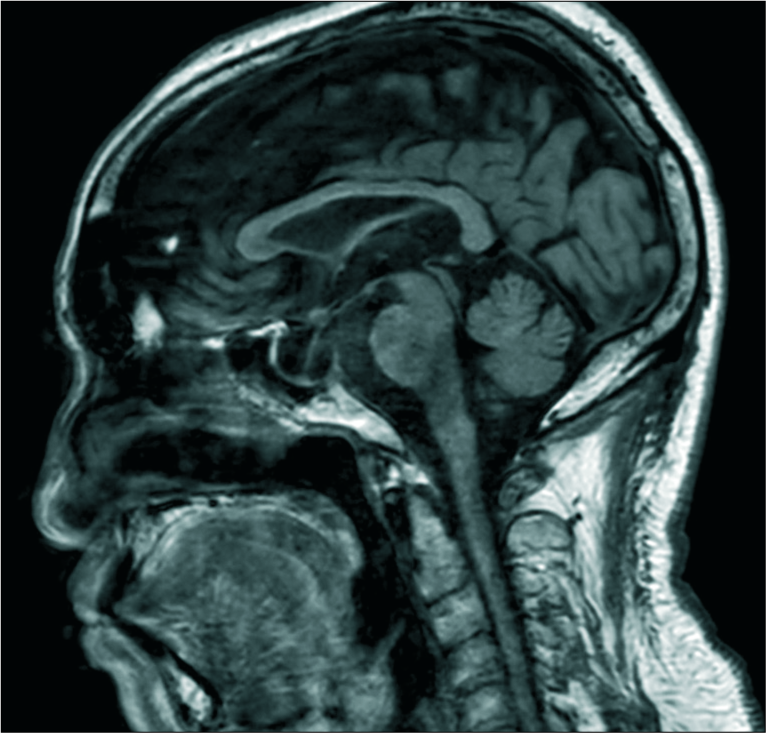
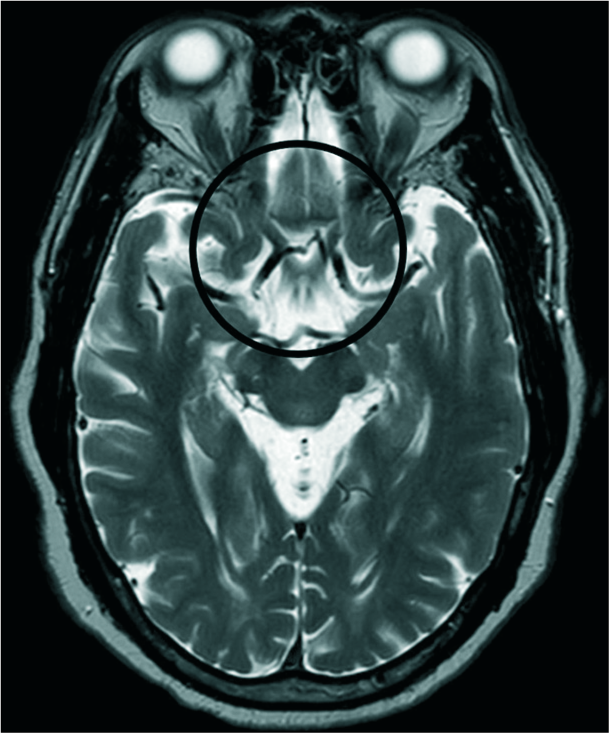
Magnetic resonance imaging (MRI) of the brain showed that he had an empty sella with normal-appearing optic nerves and chiasm [
Lab investigations for pituitary and renal function as well as peripheral blood counts were all within normal limits.
He underwent endoscopic endonasal chiasmapexy with approach to the sella turcica through a transsphenoidal route. Cerebrospinal fluid egress followed the opening of the dura and the optic chiasm was visualized. Fat and fascia harvested from the right upper lateral thigh were introduced into the sella and kept in position by bone harvested from the nasal septum. BioGlue (synthetic tissue glue) was used to cement the repair and an external lumbar drain set at negative 10 cm pressure maintained for 5 days postprocedure.
He experienced an improvement in his vision over a period of some 6 months following the procedure. Visual acuity improved to the left 6/9 and right 6/12 with virtual return of fields to normal.
Due to limited resources in the hospital where he was treated, a follow-up postoperative MRI scan of the brain was not done as would have been desired, to check the position of the graft.
DISCUSSION
Empty sella syndrome (ESS) occurs in both a primary ESS (PESS) and secondary ESS (SESS) form, respectively.[
PESS occurs due to poorly understood factors, but conditions like benign intracranial hypertension (BIH) as well as incompetence of the diaphragma sella have been implicated.[
SESS occurs as a result of pituitary surgery, medical treatment of prolactinomas with shrinkage of the tumor, pituitary apoplexy, and Sheehan’s syndrome.
Regardless of the cause, prolapse of the optic apparatus such as the chiasm into the sella turcica may result in compression of these structures against the bony edges of the sella. Further, downward displacement of the third ventricle above the optic apparatus, as well as postsurgical intrasellar arachnoid adhesions, may all play a role in visual compromise. In the case of PESS, due to BIH, there is the added problem of raised intracranial pressure causing primary optic atrophy.
Among the clinical features associated with ESS apart from visual compromise are headaches and hormonal disturbances;[
When a diagnosis of ESS associated with visual deterioration is made, it is important that an ophthalmologist rules out any other diagnosis as the cause.
Should it be a case of PESS due to BIH, the treatment of the condition by either weight loss, medical (carbonic anhydrase inhibitors, salt restriction), or surgical means (cerebrospinal fluid diversion shunts, optic nerve fenestration) may help to halt the visual decline and actually reverse the problem.[
In the rest of the cases of PESS and all the cases of SESS, elevation of the prolapsed optic chiasm back to its original position by a procedure called chiasmapexy holds the promise of restoring vision. This procedure is usually done via a transsphenoidal route and involves introduction of materials – both synthetic and natural (fat, fibrous tissue) into the sella in the space below the chiasm.[
The reversal of this patient’s visual decline following chiasmapexy procedure lends credence to the belief that, at least in some cases where there is visual deterioration associated with the appearance of an empty sella on MRI examination, the situation can be helped by this procedure.
Of note, in this case, is the fact that the optic chiasm was not radiologically shown to have prolapsed into the sella turcica, yet there was bitemporal hemianopia (pathognomonic of chiasmal pathology), as well as visual acuity loss that benefitted from the chiasmapexy procedure. This raises the question of what exactly was the cause of the visual problem and how did the procedure arrest and reverse it?
Some theories can be advanced to explain this phenomenon.
It is possible that the CSF dynamics in an ESS situation, with pressure emanating from the third ventricle with each systole, can dynamically compress the chiasm against the bony sella edges, in a manner that would not be captured by static MRI scans. Chiasmapexy would then halt this process. It is also possible that adhesions form and tent the chiasm and surrounding vasculature in unfavorable positions in an ESS setting, leading to local hypoperfusion; this is improved by the support created by chiasmapexy.
The role of the percussion wave bouncing off the sella floor with each systole, arching the chiasm can also be considered.
CONCLUSION
Such patients should at the very least be subjected to a full ophthalmological assessment to exclude other possible diagnoses and the question of whether chiasmapexy is indicated should be actively considered in appropriate cases.
Declaration of patient consent
Patients consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aijazi I, Abdullah Al Shama FM, Adam Mukhtar SH. Primary empty sella syndrome presenting with severe hyponatremia and minimal salt wasting. J Ayub Med Coll Abbottabad. 2016. 28: 605-8
2. Auer MK, Stieg MR, Crispin A, Sievers C, Stalla GK, Kopczak A. Primary empty sella syndrome and the prevalence of hormonal dysregulation. Dtsch Arztebl Int. 2018. 115: 99-105
3. Barzaghi LR, Donofrio CA, Panni P, Losa M, Mortini P. Treatment of empty sella associated with visual impairment: A systematic review of chiasmapexy techniques. Pituitary. 2018. 21: 98-106
4. Chiloiro S, Giampietro A, Bianchi A, Tartaglione T, Capobianco A, Anile C. Diagnosis of endocrine disease: Primary empty sella: A comprehensive review. Eur J Endocrinol. 2017. 177: R275-85
5. Cobb MI, Crowson M, Mintz-Cole R, Husain AM, Berger M, Jang D. Transnasal transsphenoidal elevation of optic chiasm in secondary empty sella syndrome following prolactinoma treatment. World Neurosurg. 2018. 112: 250-3
6. Evans RW. Incidental findings and normal anatomical variants on MRI of the brain in adults for primary headaches. Headache. 2017. 57: 780-91
7. Nizamani WM, Siddiqui M, Ali Momin SN, Waqas M, Jooma R. Resolution of symptomatic secondary empty sella syndrome following lumbar-peritoneal shunt. Surg Neurol Int. 2018. 9: 72-
8. Sethuraman VK, Viswanathan S, Aghoram R. Refractory hypoglycemia and seizures as the initial presenting manifestation of empty sella syndrome. Cureus. 2018. 10: e2803-
9. Taieb A, Maha KN, El Abed YH, Beizig AM, Chadli MC, Ach K. Macroprolactinemia and empty sella syndrome. Pan Afr Med. J. 2017. 27: 278-
10. Tsukiyama A, Hattori Y, Tahara S, Ishisaka E, Morimoto D, Oyama K. New technique for chiasmapexy using iliac crest bone graft: 2 Cases of visual impairment caused by empty sella syndrome. World Neurosurg. 2017. 107: 1051.e19-25