- National Centre for Neurosurgery, Beaumont Hospital/RCSI, Dublin, Ireland,
- Department of Neuropathology, Beaumont Hospital, Dublin, Ireland.
Correspondence Address:
Daniel B Murray
National Centre for Neurosurgery, Beaumont Hospital/RCSI, Dublin, Ireland,
DOI:10.25259/SNI_766_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daniel B Murray1, Jack Horan1, Alan Beausang2, Mohammed Ben Husien1. Primary intradural/extradural Ewing’s sarcoma of the sacral spine: A case report and literature review. 13-Jan-2021;12:17
How to cite this URL: Daniel B Murray1, Jack Horan1, Alan Beausang2, Mohammed Ben Husien1. Primary intradural/extradural Ewing’s sarcoma of the sacral spine: A case report and literature review. 13-Jan-2021;12:17. Available from: https://surgicalneurologyint.com/surgicalint-articles/10522/
Abstract
Background: Ewing’s sarcoma (ES) is a malignant mesenchymal tumor, most often found in the long bones, and usually affecting children and adolescents in the second decade of life. ES of the spine is a clinical rarity.
Case Description: A 45-year-old male presented with a 3-month history of lower back pain which acutely worsened in conjunction with urinary retention. The magnetic resonance imaging revealed a mass extending from L5 to S2 with additional extension through the left S2-3 neural foramen. The metastatic workup was negative. At surgery, the lesion was both intradural and extradural. Following complete surgical resection, the patient was later treated with radiation and chemotherapy.
Conclusion: Here, we report an adult male who acutely presented with low back pain attributable to primary intradural/extradural sacral ES.
Keywords: Ewing’s sarcoma, Extradural, Intradural, Primary neuroectodermal tumor, Sacrum
INTRODUCTION
Ewing’s sarcoma (ES) is a rare and highly malignant mesenchymal tumor, representing less than 10% of all primary bone sarcomas. It typically presents in the second decade of life.[
Here, we present the case of a 45-year-old male who presented with an acute exacerbation of back pain and urinary retention, attributed to an intradural/extradural lumbosacral primary ES, which was treated with gross total surgical resection followed by adjuvant radiation and chemotherapy.
CASE REPORT
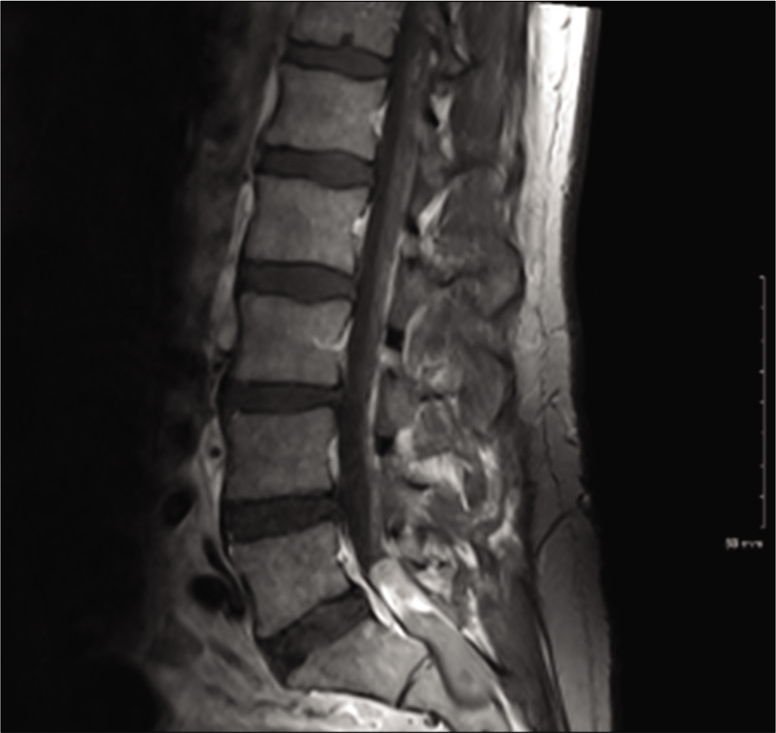
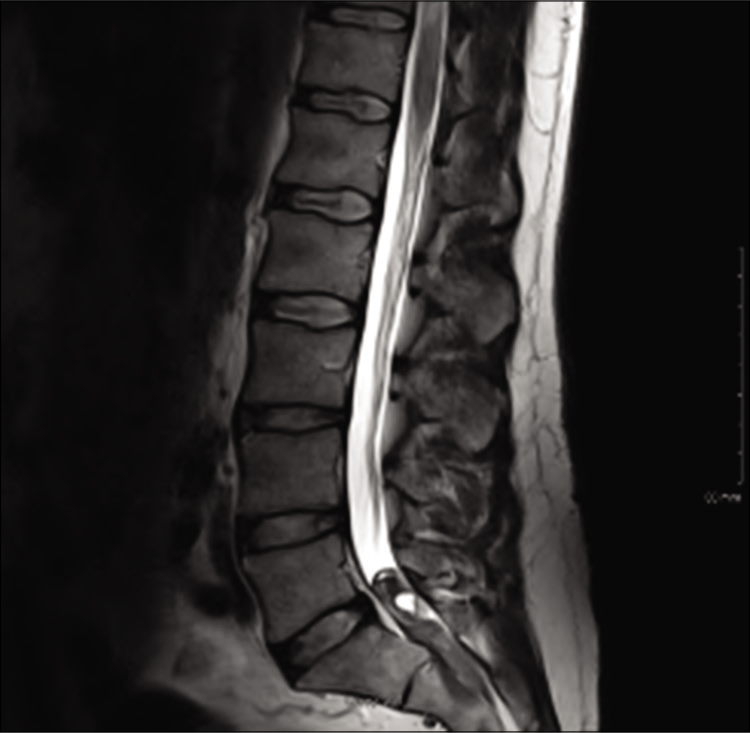
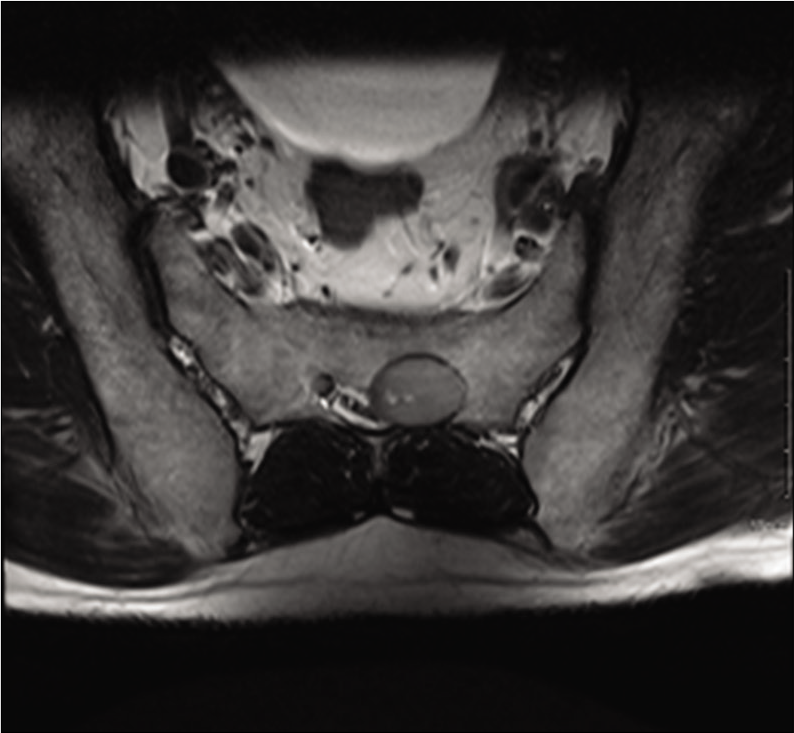
A 45-year-old male presented with a 3-month history of increasing lower back pain, which had worsened acutely with associated urinary retention over the preceding 48 h. The physical examination revealed paraspinal tenderness only, with no neurological deficits. Magnetic resonance imaging (MRI) showed a large 2 × 2 × 6 cm lobulated mass resulting in cauda equina compression from L5–S2, which extended through the left S2–3 neural foramen [
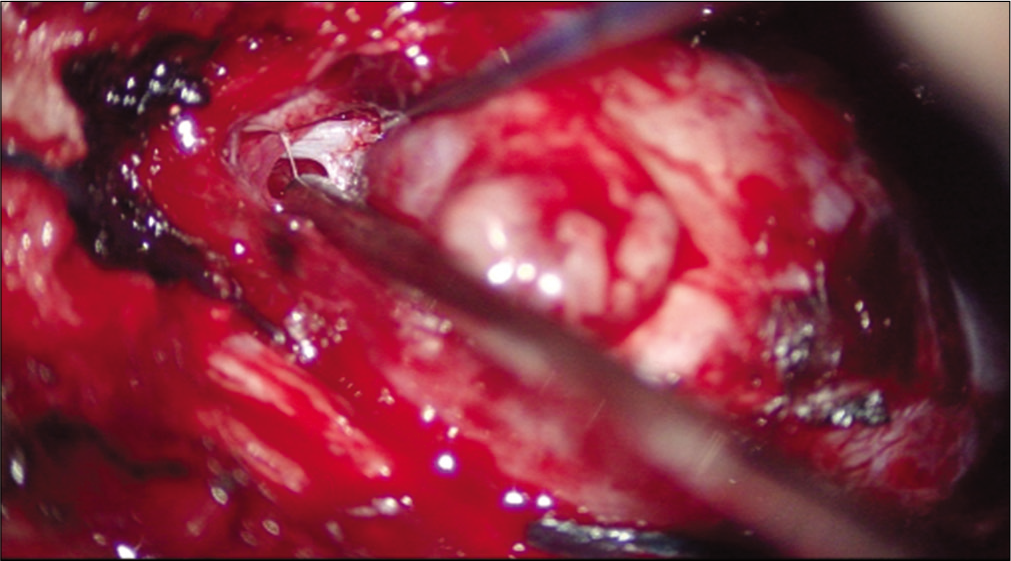
Surgery
Surgery consisted of wide bilateral laminectomies at L5–S2. The extradural component was pushing the thecal sac to the right side; it was excised en bloc. The dura was then incised and the intradural component of the tumor was also excised en bloc [
Pathology
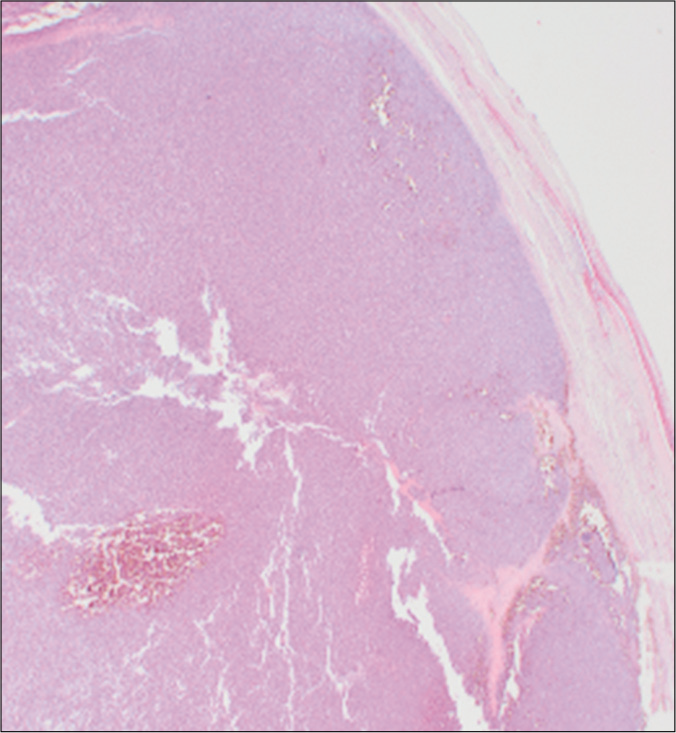
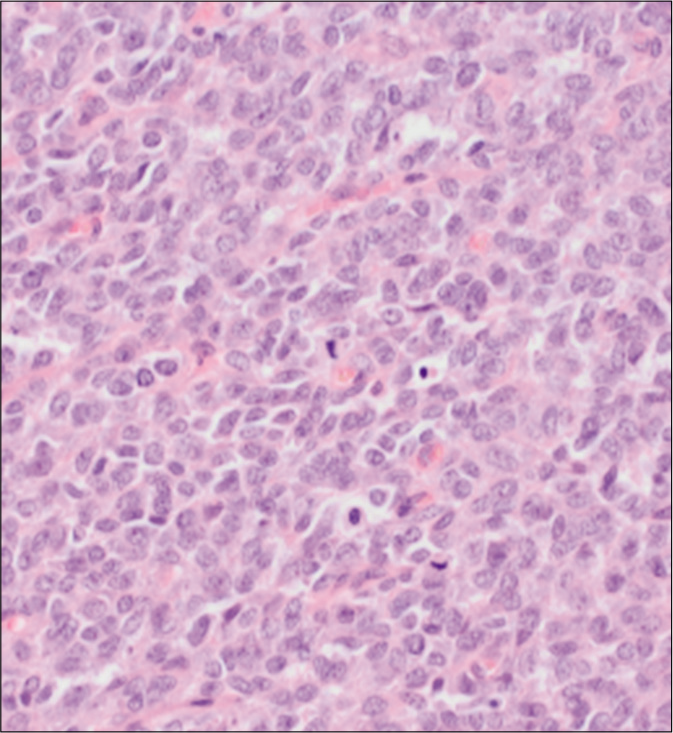
The histologic examination demonstrated a rather well-circumscribed, densely cellular neoplasm, surrounded by fibroconnective tissue, adipose tissue, and attenuated fascicles of peripheral nerve and ganglion cells [
Immunohistochemistry
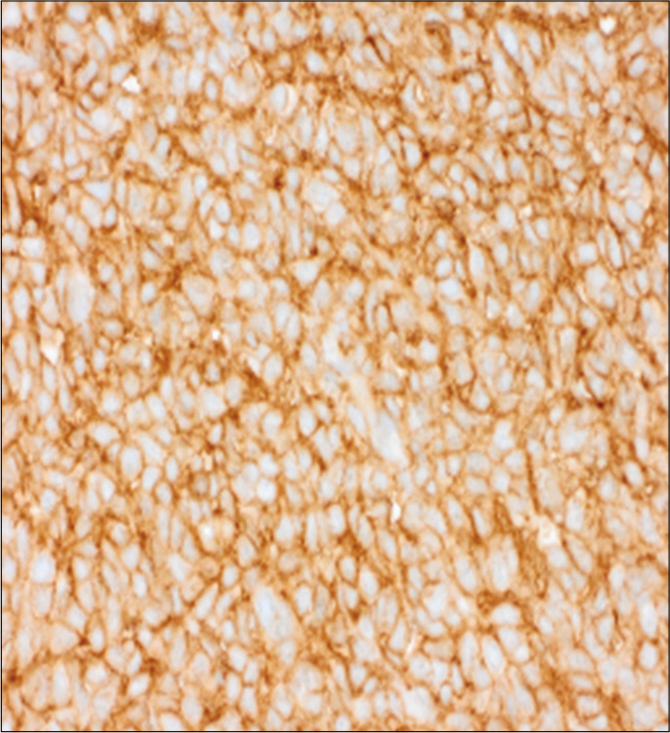
The cells within the tumor showed diffuse membranous immunopositivity with CD99 immunohistochemical stain [
DISCUSSION
Bone and soft tissue – in particular pelvis, femur, ribs, and spine – are the main sites of tumor development in ES, but less common extraosseous sites such as lung, neck and intradural extramedullary spinal ES have been reported in the literature.[
CONCLUSION
Primary intradural/extradural ES of the sacrum is exceedingly rare and is best managed with gross total excision followed by adjuvant chemotherapy and radiation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cash T, McIlvaine E, Krailo MD, Lessnick SL, Lawlor ER, Laack N. Comparison of clinical features and outcomes in patients with extraskeletal versus skeletal localized Ewing sarcoma: A report from the Children’s oncology group. Pediatr Blood Cancer. 2016. 63: 1771-9
2. Choi EY, Gardner JM, Lucas DR, McHugh JB, Patel RM. Ewing sarcoma. Semin Diagn Pathol. 2014. 31: 39-47
3. Dangoor A, Seddon B, Gerrand C, Grimer R, Whelan J, Judson I. UK guidelines for the management of soft tissue sarcomas. Clin Sarcoma Res. 2016. 6: 20
4. Esiashvili N, Goodman M, Marcus RB. Changes in incidence and survival of Ewing sarcoma patients over the past 3 decades: Surveillance epidemiology and end results data. J Pediatr Hematol Oncol. 2008. 30: 425-30
5. Gerrand C, Athanasou N, Brennan B, Grimer R, Judson I, Morland B. UK guidelines for the management of bone sarcomas. Clin Sarcoma Res. 2016. 6: 7
6. Lee J, Hoang BH, Ziogas A, Zell JA. Analysis of prognostic factors in Ewing sarcoma using a population-based cancer registry. Cancer. 2010. 116: 1964-73
7. Lu VM, Goyal A, Alvi MA, Kerezoudis P, Haddock MG, Bydon M. Primary intradural Ewing’s sarcoma of the spine: A systematic review of the literature. Clin Neurol Neurosurg. 2019. 177: 12-19
8. Paterakis K, Brotis A, Tasiou A, Kotoula V, Kapsalaki E, Vlychou M. Intradural extramedullary Ewing’s sarcoma: A case report and review of the literature. Neurol Neurochir Pol. 2017. 51: 106-10
9. Paterakis KN, Brotis A, Dardiotis E, Giannis T, Tzerefos C, Fountas KN. Multimodality treatment of intradural extramedullary Ewing’s sarcomas. A systematic review. Clin Neurol Neurosurg. 2018. 164: 169-81
10. Pilepich MV, Vietti TJ, Nesbit ME, Tefft M, Kissane J, Burgert O. Ewing’s sarcoma of the vertebral column. Int J Radiat Oncol Biol Phys. 1981. 7: 27-31