- Department of Neurosurgery, Aga Khan University Hospital, Karachi, Pakistan.
- Department of Neurosurgery, Bahria University Medical and Dental College, Karachi, Pakistan.
- Department of Radiology, Fauji Foundation Hospital, Jhelum Road, Rawalpindi, Punjab, Pakistan.
Correspondence Address:
Syed Sarmad Bukhari
Department of Radiology, Fauji Foundation Hospital, Jhelum Road, Rawalpindi, Punjab, Pakistan.
DOI:10.25259/SNI_274_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Syed Sarmad Bukhari, Muhammad Junaid, Ali Afzal, Anisa Kulsoom. Primary pediatric cerebellar gliosarcoma. 09-May-2020;11:96
How to cite this URL: Syed Sarmad Bukhari, Muhammad Junaid, Ali Afzal, Anisa Kulsoom. Primary pediatric cerebellar gliosarcoma. 09-May-2020;11:96. Available from: https://surgicalneurologyint.com/surgicalint-articles/10014/
Abstract
Background: Primary gliosarcomas of the central nervous are rare and very few have been reported in the infratentorial compartment. Here, we describe such a lesion in a 12-year-old male.
Case Description: A 12-year-old male presented with headache, ataxia, and vomiting. When Magnetic resonance studies documented a posterior fossa lesion, he underwent placement of a right ventriculoperitoneal shunt followed by a suboccipital craniectomy. The lesion proved to be a primary gliosarcoma. Unfortunately, it recurred 2 years later and required repeated resection.
Conclusion: Here, we reviewed the rare case of a 12-year-old male requiring shunt placement and suboccipital craniectomy for a primary gliosarcoma that recurred 2 years later.
Keywords: Gliosarcoma, Pediatric, Primary
INTRODUCTION
Gliosarcomas are malignant brain tumors that usually involve the temporal lobe in the supratentorial compartment; only rarely do they involve the cerebellum.[
CASE DESCRIPTION
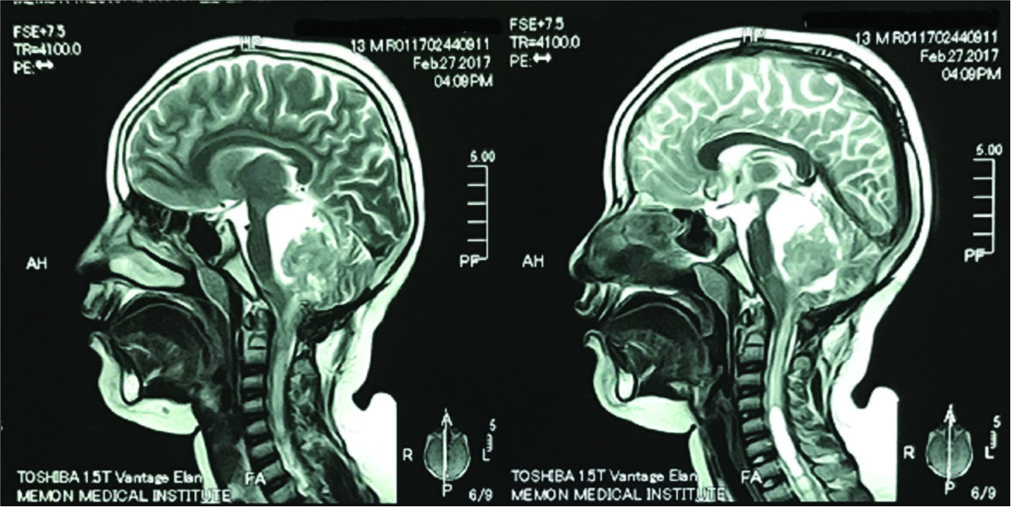
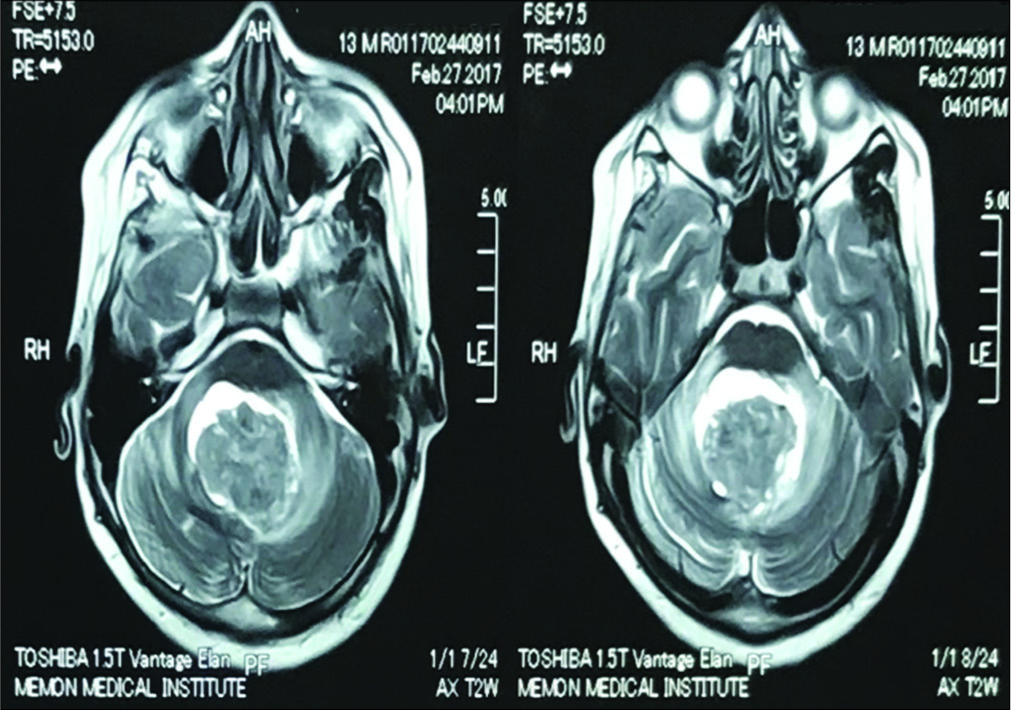
Clinical and magnetic resonance (MR) presentation
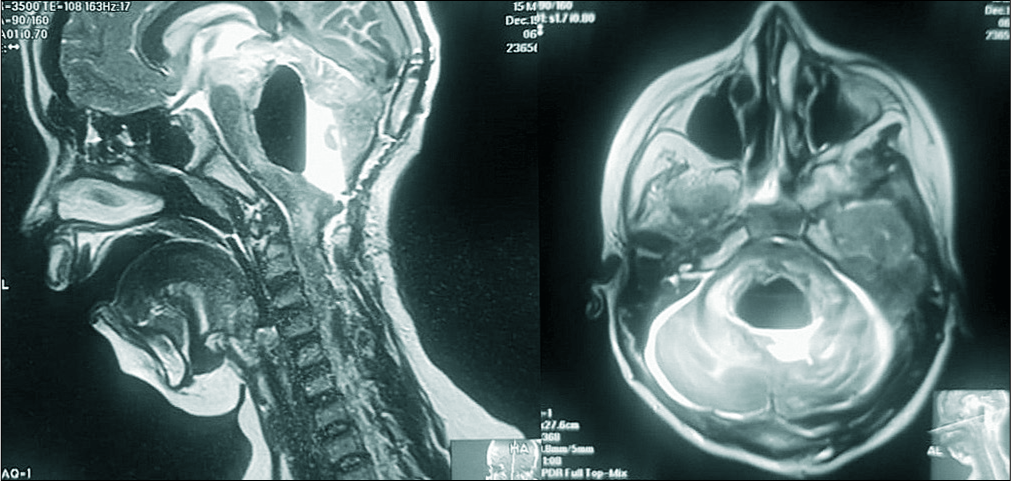
A 12-year-old male presented with headache, ataxia, and vomiting of 3 months duration. The brain MRI with/without contrast revealed a heterogenous appearing lesion within the fourth ventricle measuring 3.18 × 3.26 × 3.90 cm. There was also a small cystic component noted along the right lateral aspect which was isointense on T1, iso to hyperintense on T2, and hyperintense on the FLAIR study. Anteriorly, the tumor was causing marked compression of the medulla oblongata, pons, and midbrain; this resulted in obstructive hydrocephalus.
Surgery
The patient first underwent placement of a right-sided ventriculoperitoneal shunt. This was followed by a suboccipital craniotomy for subtotal excision of tumor. At surgery, the lesion was firm pseudo-encapsulated, and partially adherent to the brainstem on the left; due to the adhesions, a portion of the left-sided lesion was unresectable.
Pathology and immunohistochemistry
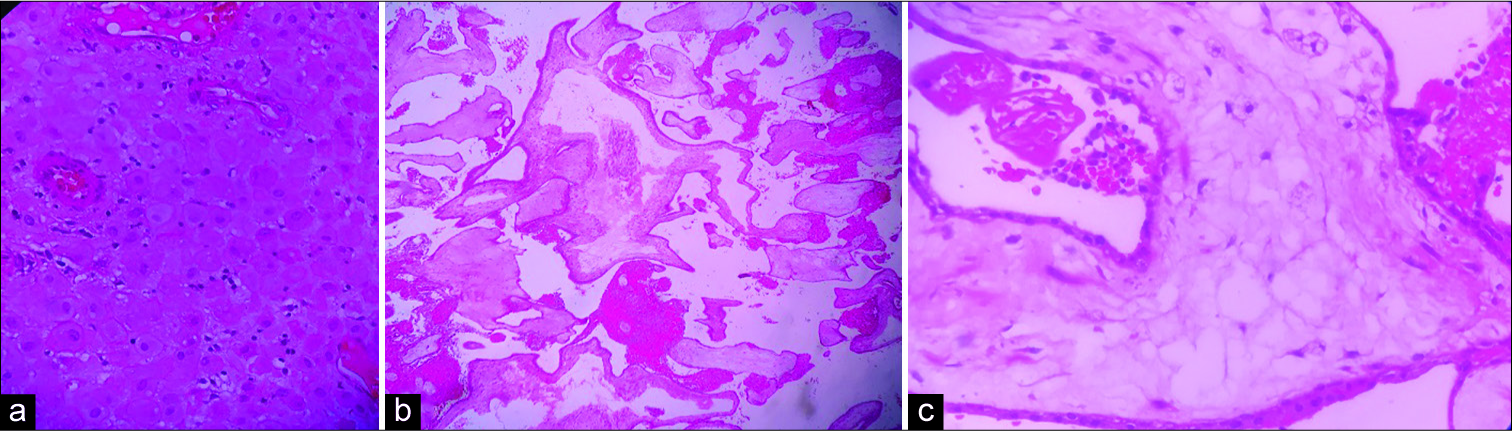
The microscopic features and the immunohistochemical profile revealed a heterogeneous tumor with hypercellular tissue that contained spindle-shaped cells that were vimentin positive. These findings confirmed the diagnosis of a cerebellar gliosarcoma [
Figure 1:
(a-c) Photomicrographs with H&E staining demonstrating the cytoarchitecture of the tumour with hypercellular and hypocellular myxoid areas. The cellular areas are composed of spindle shaped cells having mildly pleomorphic elongated nuclei. Scattered eosinophilic globules with few microtubules are seen as well.
Postoperative course and repeat MR 1 year later
The patient did well post-surgery for 1 year. However, when the MRI was repeated, it documented a significant recurrent lesion now be measuring 4.1 × 3.3 × 3.7 cm [
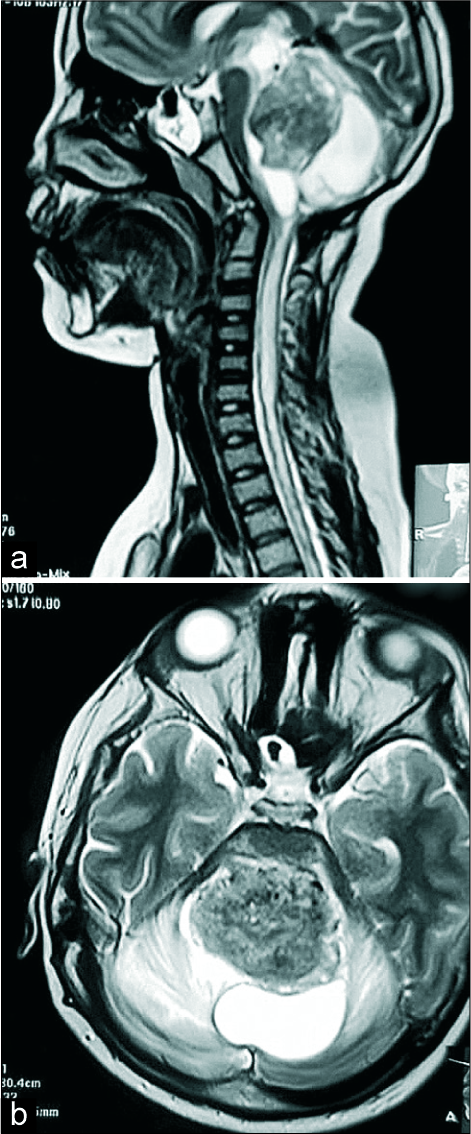
Poor outcome 2 years later without further surgery
The patient next seen 2 years postoperatively. Over the prior 3 months, he had developed progressive quadriparesis and was wheelchair bound for 1 month. Although a follow-up MRI was requested, only a T2 sequence could be obtained due to financial constraints [
DISCUSSION
WHO classification
Gliosarcoma has been classified by the World Health Organization (WHO) as high-grade tumors (Grade IV) resembling glioblastomas. They account for nearly 2% of Grade IV glial neoplasms and have a similar age distribution as glioblastoma.[
Location
Most, if not all, cases of primary gliosarcomas in the literature occur in the supratentorial compartment, very rarely, they involve the cerebellum in adults, and even less frequently, in children.[
Computed tomography (CT) and MR findings of gliosarcoma
CT
CT findings are similar to those for an infiltrating glioblastoma. They may appear as a well-defined hyperdense mass with heterogeneous ring enhancement due to their fibrous component. Central necrosis is less common due to their predilection for peripheral lobe locations. Dural involvement is not uncommon.[
MR
Nitta et al.[
Pathology of gliosarcomas
Pathologically, gliosarcomas are characterized by a biphasic tissue pattern with alternating areas of glial and mesenchymal differentiation.[
Local recurrence
Local recurrence and metastases of gliosarcomas along cerebrospinal fluid pathways are common.[
CONCLUSION
Primary infratentorial gliosarcomas are rare in children and are particularly located within the infratentorial compartment. Although shunting and resection may result in short-term improvement, these lesions typically recur, resulting in devastating neurological deficits and short-term survival.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alatakis S, Stuckey S, Siu K, McLean C. Gliosarcoma with osteosarcomatous differentiation: Review of radiological and pathological features. J Clin Neurosci. 2004. 11: 650-6
2. Han SJ, Yang I, Tihan T, Prados MD, Parsa AT. Primary gliosarcoma: Key clinical and pathologic distinctions from glioblastoma with implications as a unique oncologic entity. J Neurooncol. 2010. 96: 313-20
3. Karremann M, Rausche U, Fleischhack G, Nathrath M, Pietsch T, Kramm CM. Clinical and epidemiological characteristics of pediatric gliosarcomas. J Neurooncol. 2010. 97: 257-65
4. Malde R, Jalali R, Muzumdar D, Shet T, Kurkure P. Gliosarcoma occurring 8 years after treatment for a medulloblastoma. Childs Nerv Syst. 2004. 20: 243-6
5. Neelima R, Abraham M, Kapilamoorthy TR, Hingwala DR. Pediatric gliosarcoma of thalamus. Neurol India. 2012. 60: 674-6
6. Nitta H, Hayase H, Moriyama Y, Yamashima T, Yamashita J. Gliosarcoma of the posterior cranial fossa: MRI findings. Neuroradiology. 1993. 35: 279-80
7. Nsir B, Thai Q, Kassar AZ, Said B, Jemel H. Primary cerebellar gliosarcoma with extracranial metastases: An orphan differential diagnosis. World Neurosurg. 2015. 84: 2076.e13-7
8. Reis RM, Konu-Lebleblicioglu D, Lopes JM, Kleihues P, Ohgaki H. Genetic profile of gliosarcomas. Am J Pathol. 2000. 156: 425-32