- Department of Neurosurgery, EMC Super Speciality Hospital, Amritsar, Punjab, India.
- Department of Neurosurgery, Advanced Neurology and Superspeciality Hospital, Jaipur, Rajasthan, India.
Correspondence Address:
Sandeep Bhardwaj, Department of Neurosurgery, Advanced Neurology and Superspeciality Hospital, Jaipur, Rajasthan, India.
DOI:10.25259/SNI_575_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mukesh Vij1, Sandeep Bhardwaj2. Primary spinal dorsal extramedullary germ cell tumor: A rare case report and literature review. 08-Dec-2021;12:603
How to cite this URL: Mukesh Vij1, Sandeep Bhardwaj2. Primary spinal dorsal extramedullary germ cell tumor: A rare case report and literature review. 08-Dec-2021;12:603. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11270
Abstract
Background: Primary spinal extramedullary germ cell tumor are very rare. Germ cell tumor are similar histologically to germ cells of genital organs and may arise rarely from central and peripheral nervous system.
Case Description: We report a case of 20-year-old male who presented with progressive lower extremity weakness, spasticity, and numbness of legs. Patient was evaluated with magnetic resonance imaging dorsal spine which revealed extramedullary mass in dorsal (D2-D3) level with severe cord compression. Tumor was found to be extramedullary with histopathology consistent with germ cell tumor. Patient was given radiotherapy and chemotherapy postoperatively.
Conclusion: Primary spinal extramedullary germ cell tumors are very rare and are very sensitive to radiation and chemotherapy. Various management and treatment protocols are available across institutions in the world. We recommend adequate decompression of cord with biopsy followed by local radiation and chemotherapy. As these are rare tumors, presenting with significant neurological deficits should always be kept in the differential diagnosis.
Keywords: Dorsal mass, Extramedullary mass, Germ cell tumor
INTRODUCTION
Primary germ cell tumors may arise aberrantly may arise in the central nervous system (CNS) which are mostly similar to germinal tumors of genital organs. They may account for only 1% of all CNS tumors.[
CASE REPORT
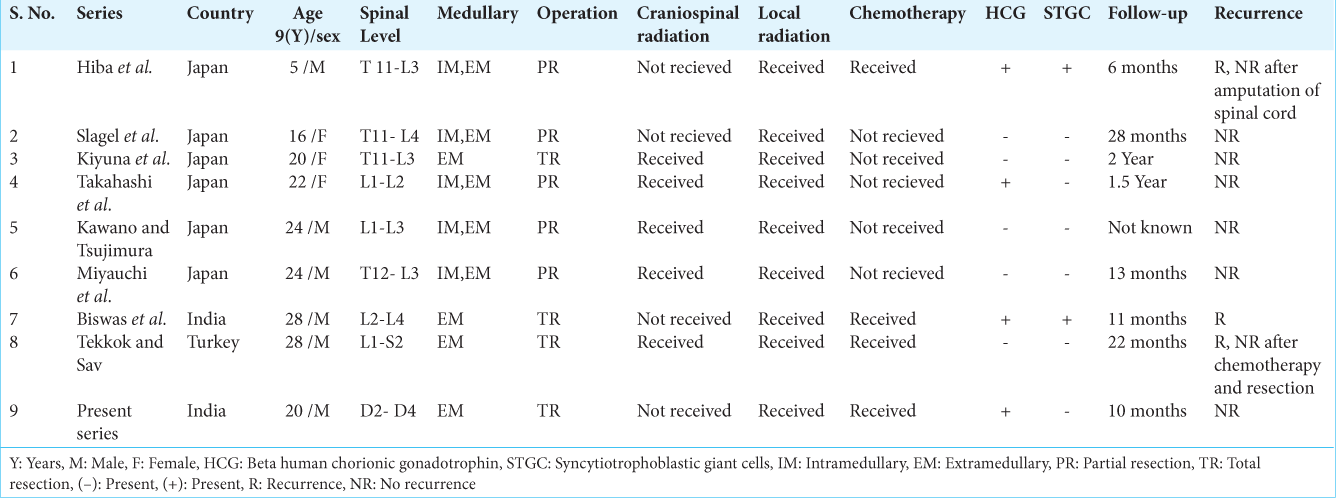
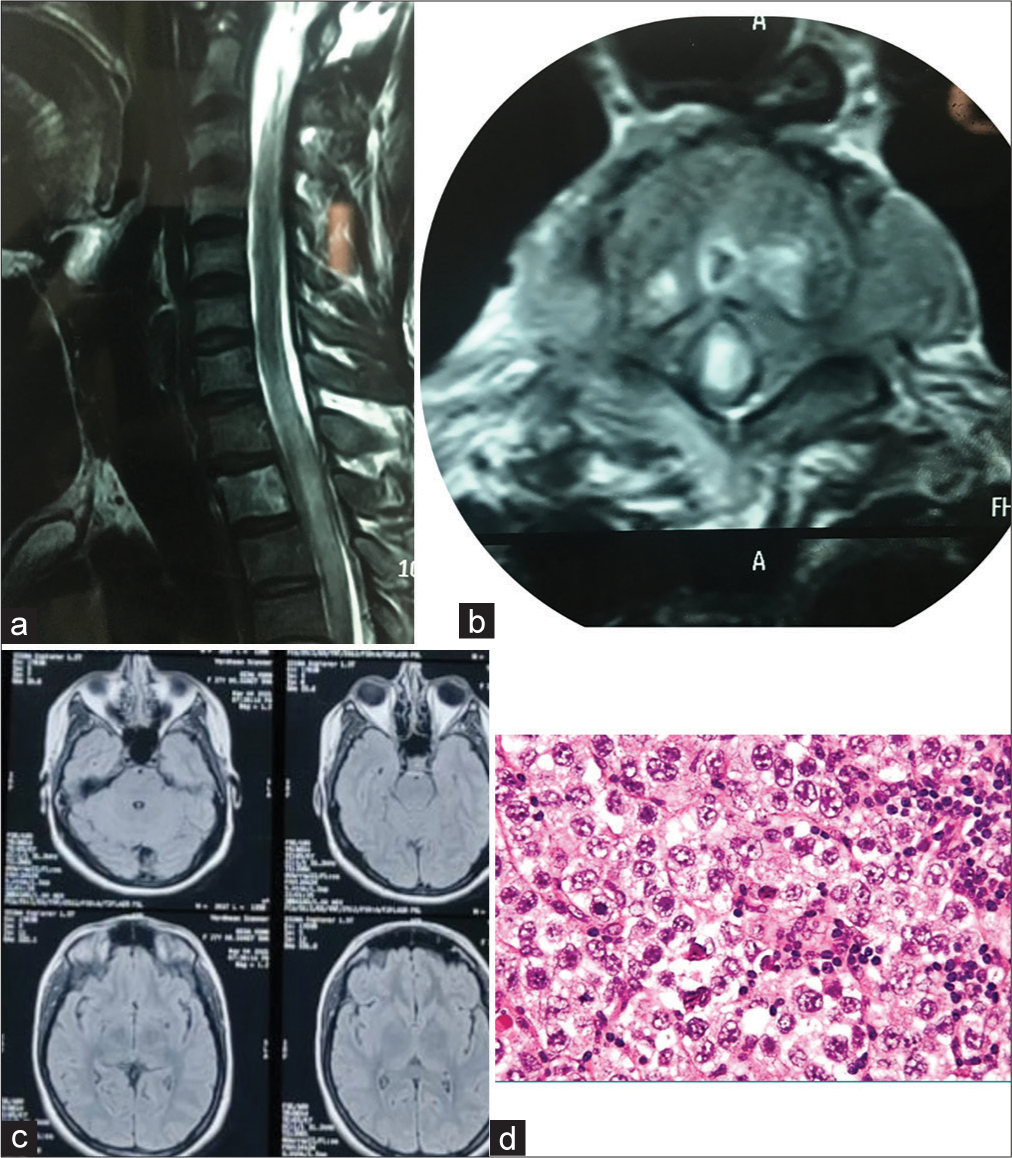
A 20-year-old male presented with difficulty in walking, weakness, and numbness in the lower extremities for the past 3 months. These symptoms slowly progressed over a period of 3 months during which he became almost bedridden. These symptoms progressed to involve bowel and bladder and lost urinary control with constipation. On examination, patient had power of 3/5 both lower limbs with loss of light touch, proprioception with bilateral clonus. Patient was evaluated with magnetic resonance imaging (MRI) dorsal spine with screening of the whole spine [
Figure 1:
(a) Magnetic resonance imaging (MRI) cervical spine (Saggital) image demonstrated extramedullary mass at D2-D3 level with diffuse cord involvement with cord compression (b) MRI cervical spine (Axial) image demonstrated extramedullary mass with involvement of D2 vertebrae involvement. (c) MRI brain was groosly normal. (d) Histopathology (two cell pattern) demonstrated that cells with large nuclei, with clear cytoplasm and defined borders. There were few lymphocytes in stroma.
Patient was operated with D2-D3 laminectomy with excision of mass. Mass was extramedullary, grayish in color, and severely compressing cord. Gross total excision of mass was done. Histopathology demonstrated typical two-cell pattern of germinoma. There were cells with large nuclei, with clear cytoplasm, and defined borders. There were few lymphocytes in the stroma. Immunostaining demonstrated positivity for placental alkaline phosphatase (PLAP) along with positivity for cytokeratin AE1. Histopathology along with immunostaining was in favor of germ cell tumor. Post-operatively patient received local radiation of 45Gy and improved neurologically. Patient was able to walk with support after 3 months and is improving gradually.
DISCUSSION
Primary spinal extramedullary germ cell tumors are very rare. Germ cell tumors account for 1% CNS tumors in Europe and US with 12.5% in East Asia.[
Backache, weakness of limbs, sensory loss, involvement of bowel and bladder are the most common presentations of spinal germ cell tumors. Other symptoms such as precocious puberty, due to high Beta-HCG production can occur.[
On immunohistochemistry, germinomas stain positive for PLAP, c-kit, and OCT4. CNS germinomas secreting serum Beta-HCG have now been termed as germinomas with syncytio-trophoblastic giant cell (STGC). These tumors usually recur and are poor prognostic.[
Surgery
Total resection, partial resection or tumor decompression, and operative biopsy are various surgical options. In the total of nine patients, five underwent partial resection and four patients achieved complete resection [
Radiotherapy
Spinal germ cell tumors are highly radiosensitive.[
Chemotherapy
Spinal germ cell tumors are also highly chemo-sensitive tumors.[
The most common cause of recurrence in spinal germ cell tumors is local recurrence or neuraxial spread.[
CONCLUSION
Primary spinal germ cell tumors are rare, but a very high index of suspicion is required to diagnose these tumors. As these tumors are highly sensitive to radiation and chemotherapy, radical surgery can be avoided in these tumors. Recurrence of these tumors is very rare, which are usually associated with STGC positivity. We recommend safe surgical decompression followed by radiotherapy and chemotherapy. Craniospinal radiation should be used as last resort in recurrence in view of its cognitive and endocrine effects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Balmaceda C. Chemotherapy for intramedullary spinal cord tumours. J Neurooncol. 2000. 47: 293-307
2. Bamberg M, Kortmann RD, Calaminus G, Becker G, Meisner C, Harms D. Radiation therapy for intracranial germinoma: Results of the German cooperative prospective trials MAKEI 83/86/89. J Clin Oncol. 1999. 17: 2585-92
3. Borg M. Germ cell tumours of the central nervous system in children-controversies in radiotherapy. Med Pediatr Oncol. 2003. 40: 367-74
4. Dearnaley DP, A’Hern RP, Whittaker S, Bloom HJ. Pineal and CNS germ cell tumors: Royal Marsden Hospital Experience 1962-87. Int J Radiat Oncol Biol Phys. 1990. 18: 773-81
5. Fine HA, Barker FG, Markert JM, Loeffer JS.editors. Neoplasms of the central nervous system. Cancer Principles and Practice of Oncology. Philadelphia, PA: Lippincott William & Wilkins; 2005. p. 1869-71
6. Haddock MG, Schild S, Scheithauer BW, Schomberg PJ. Radiation therapy for histologically confirmed primary central nervous system germinoma. Int J Radiat Oncol Biol Phys. 1997. 38: 915-23
7. Hanakita S, Takenobu A, Kambe A, Watanabe T, Shin M, Teraoka A. Intramedullary recurrence of germinoma in the spinal cord 15 years after complete remission of a pineal lesion: Case report. J Neurosurg. 2012. 16: 513-5
8. Hisa S, Morinaga S, Kobayashi Y, Ojima M, Chikaoka H, Sasano N. Intramedullary spinal cord germinoma producing HCG and precocious puberty in a boy. Cancer. 1985. 55: 2845-9
9. Inamura T, Nishio S, Ikezaki K, Fukui M. Human chorionic gonadotrophin in CSF, not serum predicts outcome in germinoma. J Neurol Neurosurg Psychiatry. 1999. 66: 654-7
10. Miyanohara O, Takeshima H, Kaji M, Hirano H, Sawamura Y, Kochi M. Diagnostic significance of soluble C-kit in the cerebrospinal fluid of patients with germ cell tumours. J Neurosurg. 2002. 97: 177-83
11. Modak S, Gardner S, Dunkel IJ, Balmaceda C, Rosenblum MK, Miller DC. Thiotepa-based high-dose chemotherapy with autologous stem-cell rescue in patients with recurrent or progressive CNS germ cell tumors. J Clin Oncol. 2004. 22: 1934-43
12. Mostofi FK. Proceedings: Testicular tumors, Epidemiologic, etiologic, and pathologic features. Cancer. 1973. 32: 1186-201
13. Nakata Y, Yagishita A, Arai N. Two patients with intraspinal germinoma associated with Klinefelter’s syndrome: Case report and review of literature. AJNR Am J Neuroradiol. 2006. 27: 1204-10
14. Ogawa K, Yoshii Y, Shikama N, Nakamura K, Uno T, Onishi H. Spinal recurrence from intracranial germinoma: Risk factors and treatment outcome for spinal recurrence. Int J Radiat Oncol Biol Phys. 2008. 72: 1347-54
15. Sawamura Y, de Tribolet N, Ishii N, Abe H. Management of primary intracranial germinomas: Diagnostic surgery or radical resection?. J Neurosurg. 1997. 87: 262-6
16. Ueda A, Tamura K, Miyazaki H, Ishiyama N. A case report of germinoma with syncytiotrophoblastic giant cells [STGC] in the basal ganglia. No Shinkei Geka. 1996. 24: 267-71