- Department of Neurological Surgery, University of Wisconsin Hospitals and Clinics, Madison, Wisconsin, United States.
Correspondence Address:
Simon Gashaw Ammanuel, Department of Neurological Surgery, University of Wisconsin Hospitals and Clinics, Madison, Wisconsin, United States.
DOI:10.25259/SNI_1073_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Simon Gashaw Ammanuel, Paul S. Page, Garret P. Greeneway, Nathaniel P. Brooks. Primary spinal infections: A retrospective review of instrumentation use and graft selection. 23-Dec-2022;13:590
How to cite this URL: Simon Gashaw Ammanuel, Paul S. Page, Garret P. Greeneway, Nathaniel P. Brooks. Primary spinal infections: A retrospective review of instrumentation use and graft selection. 23-Dec-2022;13:590. Available from: https://surgicalneurologyint.com/surgicalint-articles/12073/
Abstract
Background: The use of instrumentation in the setting of primary spinal infections is controversial. While the instrumentation is often required in the presence of progressive deformity due to spinal osteomyelitis (SO), discitis (SD), or spinal epidural abscesses (SEA), many surgeons are concerned about instrumentation increasing the risk of infection recurrence and/or persistence warranting reoperation.
Methods: We retrospectively reviewed the need for reoperations for persistent infections in 119 patients who presented with primary spinal infections. They were treated with decompressions with/without non-instrumented fusion (70 patients) versus decompressions with instrumented fusions (49 patients).
Results: The use of primary spinal instrumentation in the presence of infection (SO/SD/SEA) did not increase the requirement for repeated surgery due to recurrent/residual infection when compared to those undergoing decompressions with/without non-instrumented fusions. Of 49 patients who initially required instrumentation, 6 (12.5%) required reoperations for recurrent or residual infection. For the 71 undergoing index decompressions for infection with/without non-instrumented fusion, 9 (12.7%), or nearly an identical percentage, required reoperations for recurrent/residual infection (P = 0.93).
Conclusion: The use of instrumentation in the treatment of primary spinal infections in a small sample of just 49 patients did not increase the risk for persistent infection warranting reoperations versus 70 patients undergoing initial decompressions with/without non-instrumented fusions.
Keywords: Discitis, Epidural abscess, Osteomyelitis
INTRODUCTION
Primary spinal infections occur in 1/100,000 persons annually.[
MATERIALS AND METHODS
Two authors retrospectively reviewed 49 patients (2000–2020) who required spinal instrumentation (all Titanium) versus 71 undergoing decompressions with/without non-instrumented fusions for the treatment of spinal osteomyelitis (SO), discitis (SC), and spinal epidural abscesses (SEA). The primary outcome we focused on was the need for repeated spinal surgery to address recurrent/persistent postoperative infection within 1 year of the index surgery.
Statistical evaluation
Categorial variables were assessed using Chi-squared analysis and continuous variables were assessed using the students two sample t-test. Analysis of variance (ANOVA) was utilized for comparison of multiple categorical variables.
RESULTS
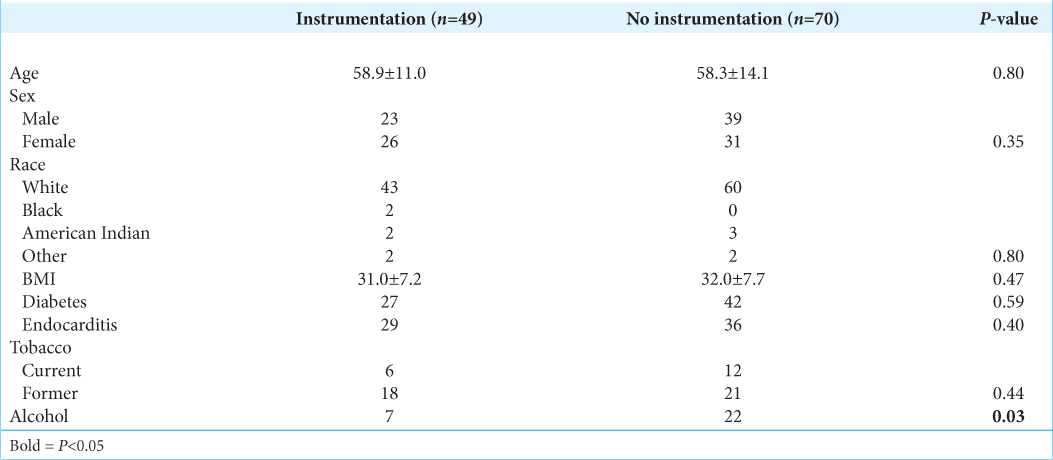
The 119 patients who required surgical intervention averaged age of 58.1 ± 13.7 years of age, and underwent either decompressions with instrumented fusions (49 patients) or decompressions with or without non-instrumented fusions. There were no significant differences in multiple variables for those receiving instrumentation, except alcohol use which was significantly greater in the latter group (P = 0.03) [
Instrumentation did not increase reoperation rates
The use of instrumentation in the presence of a primary spinal infection for SO/SD/SEA did not increase the reoperation rates for recurrent/residual infection: 6/49 (12.0%) undergoing primary instrumented fusions required reoperations versus 9/70 (13.0%) undergoing decompressions with/without non-instrumented fusions (P = 0.87).
DISCUSSION
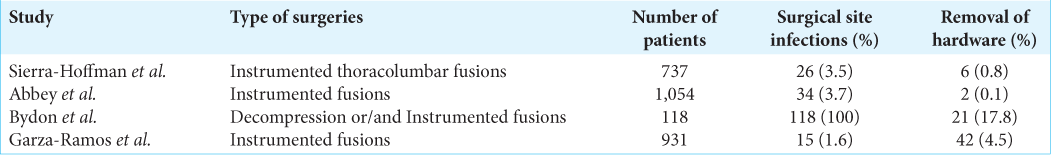
In the presence of active infection, the use of foreign bodies including spinal instrumentation is generally avoided due to the potential for it to serve as a nidus for recurrent infection.[
CONCLUSION
The use of spinal instrumentation for the treatment of primary spinal infections in 49 patients did not increase the risk of persistent/recurrent infection when compared with 71 patients undergoing decompressions with/without non-instrumented fusions.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abbey DM, Turner DM, Warson JS, Wirt TC, Scalley RD. Treatment of postoperative wound infections following spinal fusion with instrumentation. J Spinal Disord. 1995. 8: 278-83
2. Bydon M, De la Garza-Ramos R, Macki M, Naumann M, Sciubba DM, Wolinsky JP. Spinal instrumentation in patients with primary spinal infections does not lead to greater recurrent infection rates: An analysis of 118 cases. World Neurosurg. 2014. 82: e807-14
3. De la Garza-Ramos R, Bydon M, Macki M, Abt NB, Rhee J, Gokaslan ZL. Instrumented fusion in the setting of primary spinal infection. J Neurosurg Sci. 2017. 61: 64-76
4. Eismont FJ, Bohlman HH, Soni PL, Goldberg VM, Freehafer AA. Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg Am. 1983. 65: 19-29
5. Kemp HB, Jackson JW, Jeremiah JD, Hall AJ. Pyogenic infections occurring primarily in intervertebral discs. J Bone Joint Surg Br Vol. 1973. 55: 698-714
6. Lamagni T. Epidemiology and burden of prosthetic joint infections. J Antimicrob Chemother. 2014. 69: i5-10
7. Schimmer RC, Jeanneret C, Nunley PD, Jeanneret B. Osteomyelitis of the cervical spine: A potentially dramatic disease. J Spinal Disord Tech. 2002. 15: 110-7
8. Sierra-Hoffman M, Jinadatha C, Carpenter JL, Rahm M. Postoperative instrumented spine infections: A retrospective review. South Med J. 2010. 103: 25-30