- Department of Neurosurgery, Montefiore Medical Center, University Hospital for Albert Einstein College of Medicine, Bronx, NY, USA
- Department of Plastics Surgery, University of New Mexico, 1 University of New Mexico, Albuquerque, NM, USA
- Department of Neurosurgery, Brown University, Providence, RI 02903, USA
- Department of Radiology, Montefiore Medical Center, University Hospital for Albert Einstein College of Medicine, Bronx, NY 10467, USA
Correspondence Address:
David Joseph Altschul
Department of Neurosurgery, Montefiore Medical Center, University Hospital for Albert Einstein College of Medicine, Bronx, NY, USA
DOI:10.4103/sni.sni_396_18
Copyright: © 2019 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Rose Fluss, Avra Laarakker, Jonathan Nakhla, Allan Brook, David Joseph Altschul. Prolonged delayed vasospasm in the setting of nonaneurysmal intraventricular hemorrhage. 11-Mar-2019;10:29
How to cite this URL: Rose Fluss, Avra Laarakker, Jonathan Nakhla, Allan Brook, David Joseph Altschul. Prolonged delayed vasospasm in the setting of nonaneurysmal intraventricular hemorrhage. 11-Mar-2019;10:29. Available from: http://surgicalneurologyint.com/surgicalint-articles/9255/
Abstract
Background:Though still thought to be rare, in recent years, vasospasm as a result of primary intraventricular hemorrhage (IVH) has been increasingly recognized in patients with spontaneous primary intraventricular hemorrhage, of various etiologies. Unlike vasospasm in aneurysmal subarachnoid hemorrhage (SAH), which has a well-defined time frame of 3–21 days, such a window is poorly defined for primary spontaneous intraventricular hemorrhage from other vascular etiologies.
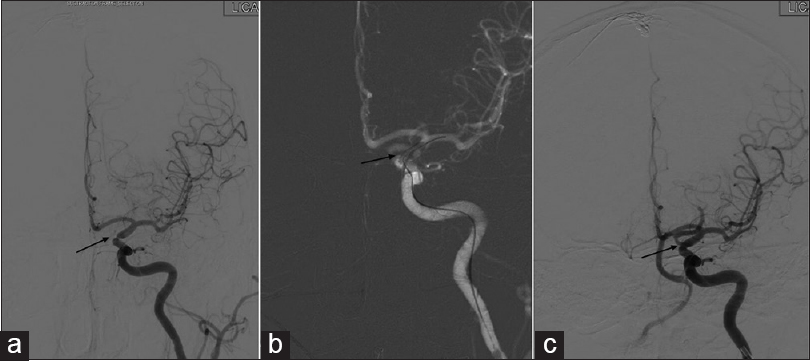
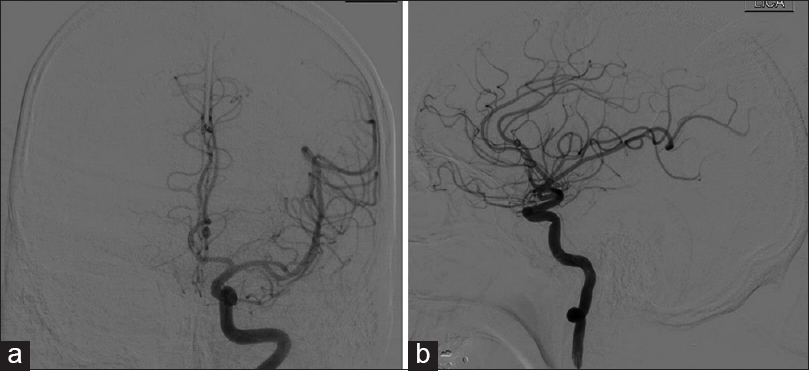
Case Description:We report on two cases of prolonged delayed proximal intracranial cerebral vasospasm occurring 29 and 22 days after the initial presentation.
Conclusion:To our knowledge, this is the first report of such delayed vasospasm in spontaneous primary intraventricular hemorrhage secondary to a dural arteriovenous fistula and cavernous malformation. Our two cases of vasospasm in patients with nontraumatic nonaneurysmal SAH with IVH presented outside the expected time period of 21 days. It is important to recognize that symptomatic vasospasm secondary to intraventricular hemorrhage is a rare but devastating complication that can have serious deleterious consequences if gone unrecognized and untreated.
Keywords: Delayed cerebral ischemia, delayed cerebral vasospasm, intraventricular hemorrhage
BACKGROUND
Though still thought to be rare, in recent years, vasospasm of vascular origin with intraventricular hemorrhage (IVH) has been increasingly recognized in patients with spontaneous primary intraventricular hemorrhage, of various etiologies.[
CASE DESCRIPTION
Patient 1
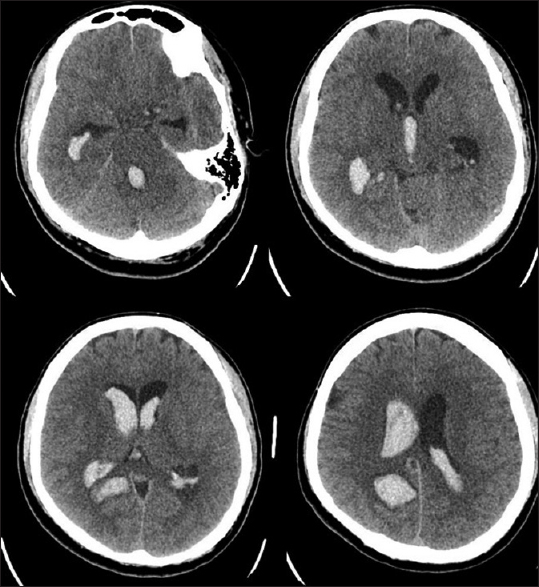
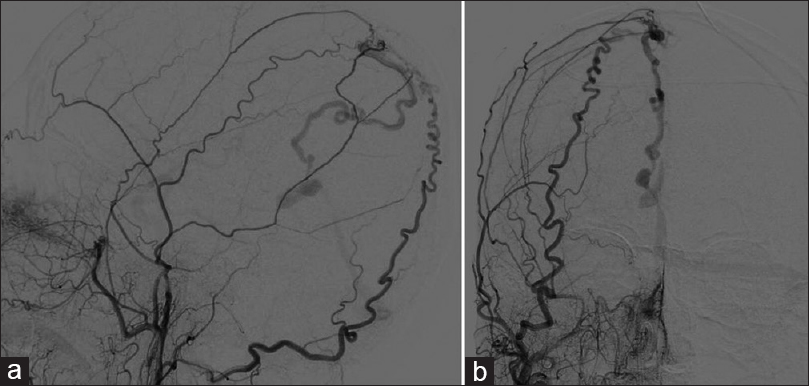
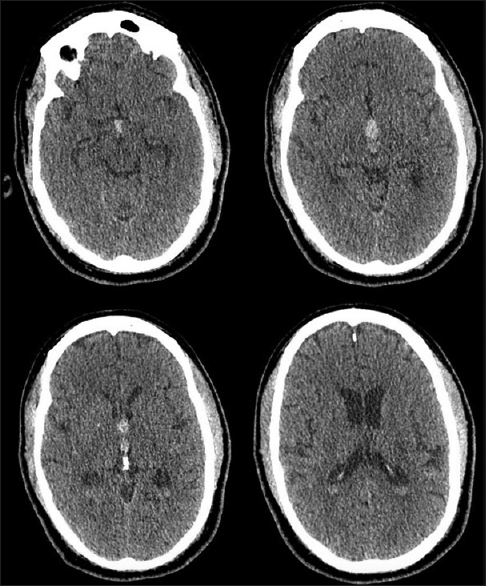
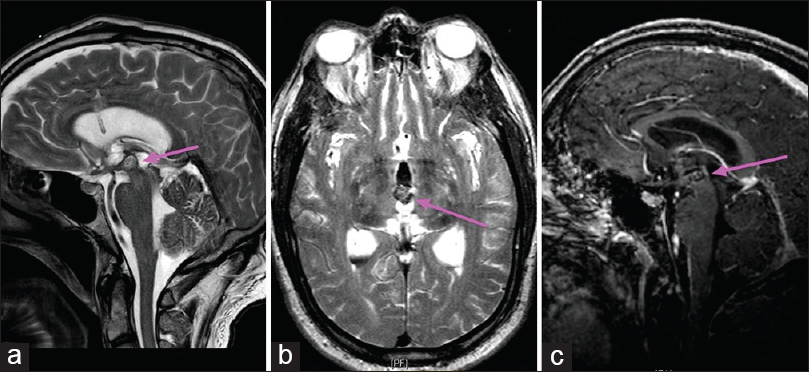
A 47-year-old man was presented with acute onset of nausea, light-headedness, palpitations, and fatigue. His mental status deteriorated but his neurological exam was otherwise nonfocal. Computed tomography (CT) [
Patient 2
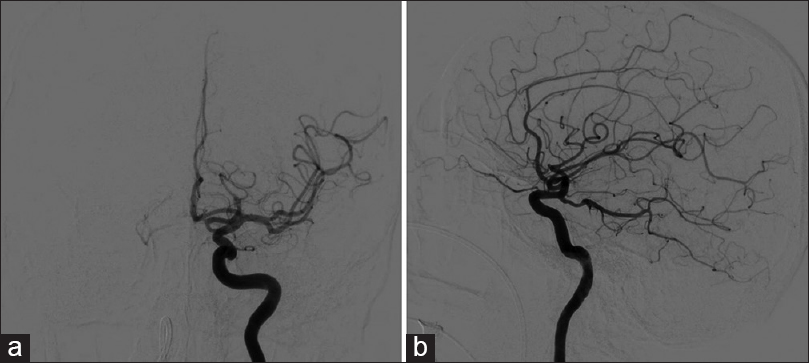
The patient is a 66-year-old right-handed man with a remote history of idiopathic intraventricular hemorrhage 6 years prior to presentation at our clinic. He was presented to the ER with severe headaches and was found to again have an intraventricular hemorrhage on CT scan [
CONCLUSION
We described above two rare cases of patients with IVH with symptomatic vasospasm occurring outside the anticipated window for vasospasm. The proposed mechanism for delayed vasospasm is thought to be recirculation of IVH into the subarachnoid space as opposed to vasospasm due to the direct presence of blood in the subarachnoid space. Since the process of recirculation takes time to occur, the actual time for vasospasm presentation is directly related to the time it takes for blood to enter the subarachnoid space. When accounting for this time delay, the vasospasm actually occurs within the normal timeframe. We speculate that due to this process of recirculation, the window of concern for vasospasm is both delayed and prolonged, as was seen in our two patients. The understanding of resorption and clearance of IVH is poorly described, but time of clearance would presumably be longer and may contribute to the delayed effect on the intracranial arteries in the subarachnoid space. Additionally, large volumes of blood would also have prolonged clearance time and thus prolong the exposure of blood, blood breakdown products, and inflammatory cytokines to the blood vessels leading to delayed vasospasm. It is important to recognize that symptomatic vasospasm secondary to intraventricular hemorrhage is a rare but devastating complication that can have serious deleterious consequences if remained unrecognized and untreated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dull C, Torbey MT. Cerebral vasospasm associated with intraventricular hemorrhage. Neurocrit Care. 2005. 3: 150-2
2. Gerard E, Frontera JA, Wright CB. Vasospasm and cerebral infarction following isolated intraventricular hemorrhage. Neurocrit Care. 2007. 7: 257-9
3. Kobayashi M, Takayama H, Mihara B, Kawase T. Severe vasospasm caused by repeated intraventricular haemorrhage from small arteriovenous malformation. Acta Neurochir (Wien). 2002. 144: 405-6
4. Kothbauer K, Schroth G, Seiler RW, Do D-D. Severe symptomatic vasospasm after rupture of an arteriovenous malformation. Am J Neuroradiol. 1995. 16: 1073-5
5. Macdonald RL. Delayed neurological deterioration after subarachnoid haemorrhage. Nat Rev Neurol. 2014. 10: 44-58
6. Park BS, Won YS, Choi CS, Kim BM. Severe symptomatic vasospasm following intraventricular hemorrhage from arteriovenous fistula. J Korean Neurosurg Soc. 2009. 45: 300-2
7. Yanaka K, Hyodo A, Tsuchida Y, Yoshii Y, Nose T. Symptomatic cerebral vasospasm after intraventricular hemorrhage from ruptured arteriovenous malformation. Surg Neurol. 1992. 38: 63-7
8. Yokobori S, Watanabe A, Nakae R, Onda H, Fuse A, Kushimoto S. Cerebral vasospasms after intraventricular hemorrhage from an arteriovenous malformation-case report. Neurol Med Chir (Tokyo). 2010. 50: 320-3