- Department of Orthopedic Surgery, University of South Dakota Sanford School of Medicine, Sioux Falls, South Dakota, United States.
- Department of Neurology, University of South Dakota Sanford School of Medicine, Sioux Falls, South Dakota, United States.
Correspondence Address:
Hunter A. O’Connor, Department of Orthopedic Surgery, University of South Dakota Sanford School of Medicine, Sioux Falls, South Dakota, United States.
DOI:10.25259/SNI_30_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hunter A. O’Connor1, Paul F. Thanel1, Shouri K. Dirks2, Abdul R. Alchaki2. Rapid expansion of post traumatic syringomyelia following parathyroidectomy: A case report and review of the literature. 19-May-2023;14:178
How to cite this URL: Hunter A. O’Connor1, Paul F. Thanel1, Shouri K. Dirks2, Abdul R. Alchaki2. Rapid expansion of post traumatic syringomyelia following parathyroidectomy: A case report and review of the literature. 19-May-2023;14:178. Available from: https://surgicalneurologyint.com/surgicalint-articles/12327/
Abstract
Background: Post-traumatic syringomyelia (PTS) is an uncommon complication of spinal cord injury (SCI) characterized by development of a fluid filled cavity in the spinal cord parenchyma. Presentation involves pain, weakness, and abnormal reflexes. There are few known triggers for disease progression. We present a case of symptomatic PTS that appears to have been triggered by parathyroidectomy.
Case Description: A 42-year-old female with a distant history of SCI developed clinical and imaging findings consistent with acute expansion of PTS immediately following parathyroidectomy. Her symptoms included acute numbness, tingling, and pain in both arms. Magnetic resonance imaging (MRI) revealed a syrinx in the cervical and thoracic spinal cord. However, this was initially misdiagnosed as transverse myelitis and was treated as such without resolution of symptoms. Over the following 6 months, the patient experienced progressive weakness. Repeat MRI demonstrated expansion of the syrinx with new involvement of the brain stem. The patient was diagnosed with PTS and referred for outpatient neurosurgery evaluation at a tertiary facility. Treatment was delayed due to problems with housing and scheduling at the outside facility, allowing for continued worsening of her symptoms. The syrinx was surgically drained and a syringo-subarachnoid shunt was placed. Follow-up MRI confirmed correct placement of the shunt as well as resolved syrinx and decreased thecal sac compression. The procedure effectively halted symptom progression but did not resolve all symptoms completely. The patient has regained her ability to perform much of her activities of daily living but remains in a nursing home facility.
Conclusion: There are currently no cases of PTS expansion following non-central nervous system surgery reported in the literature. The reason for PTS expansion following parathyroidectomy in this case is unknown but may highlight the need for extra caution when intubating or positioning a patient with a history of SCI.
Keywords: Myelitis mimic, Post parathyroidectomy complication, Post-traumatic syringomyelia, Syringobulbia
INTRODUCTION
Post traumatic syringomyelia (PTS) is an uncommon complication of spinal cord injury (SCI) characterized by the formation of a cystic fluid filled cavity within the parenchyma of the spinal cord months to years after injury.[
CASE PRESENTATION
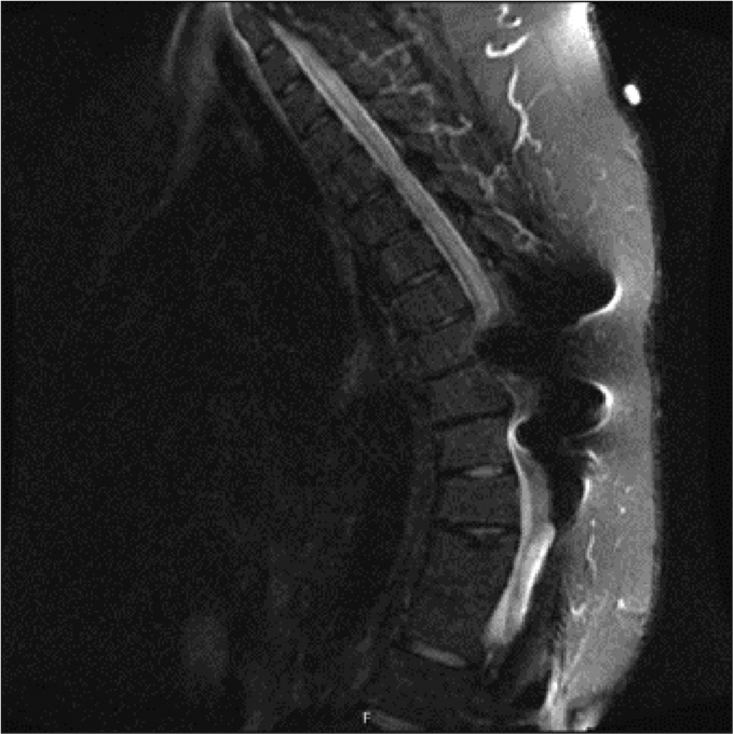
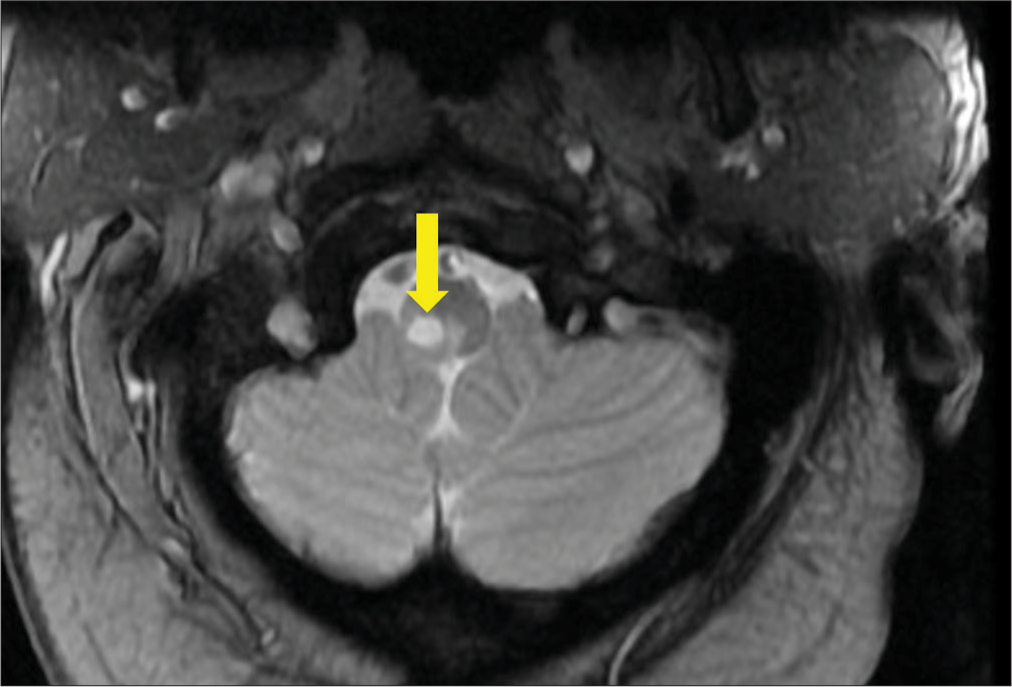
A 42-year-old Native American female presented to University of South Dakota Sanford Medical Center in December of 2020 after developing numbness, tingling, and a sharp shooting pain in both arms immediately following parathyroidectomy for parathyroid adenoma (S = 0). The numbness, tingling, and pain were worse in the right arm and radiated across the upper back and chest. Medical history was significant for a traumatic SCI caused by a motor vehicle collision at the age of 15. Following her injury, she experienced paralysis of her bilateral lower extremities, classified by the American Spinal Injury Association (ASIA) as an ASIA B injury. Her injury required thoracolumbar stabilization with Harrington rods. She had resulting chronic foot drop and was only able to ambulate with a walker. The patient did not report any history of upper extremity symptoms prior to parathyroidectomy. Examination of the patient was significant for morbid obesity with a body mass index (BMI) of 51. She had decreased temperature and light touch sensation in the upper extremities and neck in dermatomes C3 through T10 with preserved proprioception and vibration sense. Hypocalcemia was suspected as a cause of her paresthesias considering her recent parathyroidectomy, but calcium levels were normal. Cervical magnetic resonance imaging (MRI) 2 days after symptoms onset (S+2 days) demonstrated a T2 signal hyperintense area, just to the right of midline, that extended throughout the length of the central cervical spinal cord, consistent with an expanding syrinx [
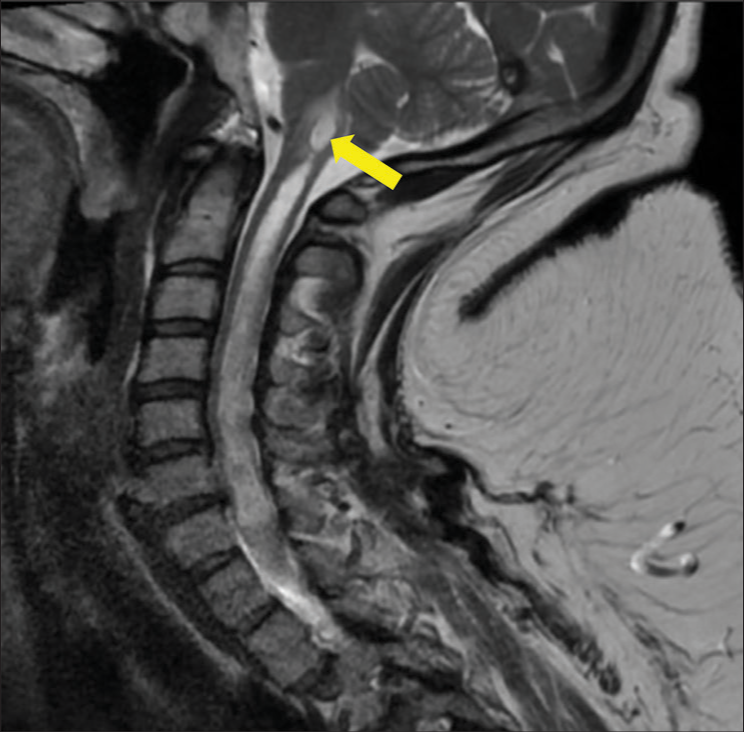
Six months after discharge (S+7 months), the patient presented to our neurology clinic for increasing weakness in the lower extremities, worsening dexterity of her right hand, and more frequent falls. These symptoms had progressed to the point of requiring her to move to an assisted living facility as she was unable to complete her activities of daily livings (ADLs) independently. On examination, there was new pronator drift, decreased right hip flexion strength, and decreased reflexes in the right upper extremity. Based on the patient’s current and previous symptoms along with the previous imaging, we were able to arrive at a diagnosis of PTS, which had previously been missed. Cervical MRI was repeated and showed rostral expansion of the syrinx into the brain stem [
The consulting neurosurgeon at the outside facility did not believe her condition warranted hospital admission and requested that she be seen on an outpatient basis. Due to a combination of difficulty finding temporary housing for the patient that could provide skilled nursing care, and difficulty working the patient into the neurosurgeon’s schedule, the patient’s care was delayed. She was not seen by the neurosurgeon for another 6 weeks (S+9.5 months). During that time period, the patient became progressively weaker, and had more frequent falls. She also developed a hoarse voice, concerning for vocal cord paralysis, and dysphagia with several episodes of choking.
On evaluation at the outside facility the evaluating neurosurgeon concluded that the patient’s symptom severity and rapid progression were indications for surgical drainage of the syrinx. The patient was taken to the operating room, and a C7-T2 laminectomy was performed. After removing the C7 through T2 lamina and entering the dura, the cord was noted to be quite dilated, nearly filling the entire dural tube, and was rotated 90° within the dura. A 2 mm hole was made in the dorsal root entry zone of the cord below the C8 nerve root to insert the shunt. The syrinx cavity was encountered at a depth of <1 mm, and the cord immediately deflated after penetration of the syrinx. A syringo-subarachnoid shunt was placed to allow the syrinx to continuously drain. The surgery and immediate postsurgical period were uncomplicated.
She was discharged back to her previous nursing home 9 days following the operation. The patient was ambulating back at her baseline with a walker. Follow-up 2 months after surgery (S+12 months) noted subjective persistent but not worsened right arm and leg weakness, as well as weakened voice. At this point, the patient was able to complete her ADLs independently although she had assistance at home. It was determined that the surgery stabilized as well as halted the progression of her neurological symptoms but did not reverse them. Cervical MRI 4 months after surgery (S+14 months) showed dramatic reduction in syrinx size, with only a small residual fluid collection, which confirmed that the shunt was patent and functioning [
DISCUSSION
To the best of our knowledge, there are not currently any other reports in the literature of acute progression of PTS following a non-CNS surgery. Usually, the onset of PTS symptoms is unpredictable, and progression does not follow a known trigger.[
The patient in the current case had delayed diagnosis and surgical intervention due to multiple preventable factors including misdiagnosis and logistical issues reaching the outside facility. Earlier surgical intervention likely would have prevented progression of the patient’s neurologic deficits. The patient’s condition was initially misdiagnosed as transverse myelitis due to a radiology misread. The reading radiologist reported that they did not believe the initial MRI imaging represented syringomyelia because the signal was present in the lateral rather than central aspect of the spinal cord. The radiologist’s interpretation is true for the most common form of syringomyelia, the congenital form, but is not true for PTS. Congenital syringomyelia, associated with Chiari malformation, is always contiguous with the central spinal cord. In contrast, PTS is not continuous with the central spinal cord canal and is instead present in the peripheral spinal cord parenchyma.[
Ultimately, it remains unclear why the patient in the current case had acute progression of her syrinx following parathyroid surgery. However, the striking temporal relationship between parathyroidectomy and PTS expansion in this case does suggest an association between the two. This likely highlights the importance of careful positioning and intubation of patients with a history of SCI. This case also illustrates the importance of having a high clinical suspicion for PTS in patient with history of SCI and an acute presentation of neurologic deficits.
CONCLUSION
PTS is an uncommon complication of SCI that can result in significant long-term disability. PTS usually presents with progressive pain, weakness, decreased deep tendon reflexes, and increased spasticity 10–15 years after SCI. Disease progression is usually unpredictable, but this case demonstrates that rapid progression of PTS can occur following non-CNS surgery. This may indicate the need for additional caution when intubating or positioning patients with a history of SCI. PTS presents as a T2 hyperintensity in a non-central portion of the spinal cord parenchyma, and increased awareness of these imaging findings could prevent misdiagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Balmaseda MT, Wunder JA, Gordon C, Cannell CD. Posttraumatic syringomyelia associated with heavy weightlifting exercises: Case report. Arch Phys Med Rehabil. 1988. 69: 970-2
2. Bonfield CM, Levi AD, Arnold PM, Okonkwo DO. Surgical management of post-traumatic syringomyelia. Spine (Phila Pa 1976). 2010. 35: S245-58
3. Brodbelt AR, Stoodley MA. Post-traumatic syringomyelia: A review. J Clin Neurosci. 2003. 10: 401-8
4. Carroll AM, Brackenridge P. Post-traumatic syringomyelia: A review of the cases presenting in a regional spinal injuries unit in the north east of England over a 5-year period. Spine (Phila Pa 1976). 2005. 30: 1206-10
5. Di Lorenzo N, Maleci A, Williams BM. Severe exacerbation of post traumatic syringomyelia after lithotripsy. Case report. Paraplegia. 1994. 32: 694-6
6. Krebs J, Koch HG, Hartmann K, Frotzler A. The characteristics of posttraumatic syringomyelia. Spinal Cord. 2016. 54: 463-6
7. Schurch B, Wichmann W, Rossier AB. Post-traumatic syringomyelia (cystic myelopathy): A prospective study of 449 patients with spinal cord injury. J Neurol Neurosurg Psychiatry. 1996. 60: 61-7
8. Williams B. Post-traumatic syringomyelia, an update. Paraplegia. 1990. 28: 296-313









Antonio Mock
Posted June 3, 2023, 9:48 am
With no MRI previous to any neck surgical procedure, is quite dificcult to say that the present syrinx increase due to the parathiroidectomy.
Any ways, is an intersting case.