- Department of Neurosurgery, Cheikh Zaid International University Hospital, Abulcasis International University of Health Sciences, Rabat, Morocco.
DOI:10.25259/SNI_468_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fahd Derkaoui Hassani, Claire Karekezi, Najia El Abbadi. Rare case of giant pediatric cavernous angioma of the temporal lobe: A case report and review of the literature. 10-Jan-2020;11:7
How to cite this URL: Fahd Derkaoui Hassani, Claire Karekezi, Najia El Abbadi. Rare case of giant pediatric cavernous angioma of the temporal lobe: A case report and review of the literature. 10-Jan-2020;11:7. Available from: https://surgicalneurologyint.com/surgicalint-articles/9836/
Abstract
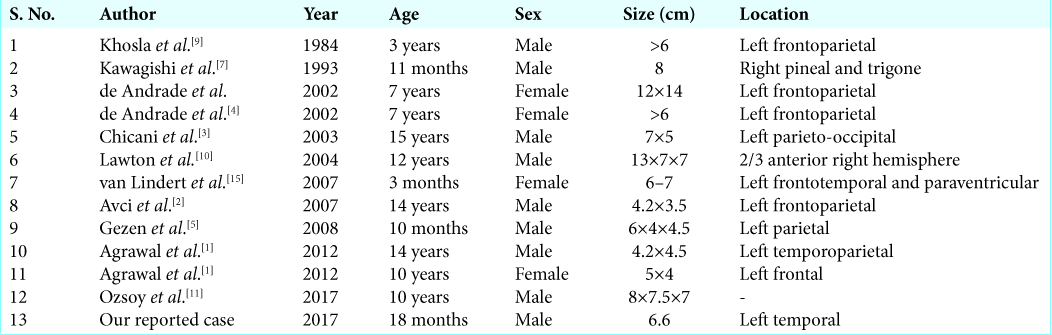
Background: Giant cavernous malformations of the central nervous system are quite rare. They are more common in children and may be misdiagnosed as other intracranial neoplasms. Here, we presented a very rare giant cavernous angioma mimicking a neoplastic temporal lobe lesion in an 18-month-old male.
Case Description: An 18-month-old male presented with two initial seizures. Although the clinical examination was normal, the computed tomography (CT) scan showed a large left temporal mass (66 mm diameter) exerting significant mass effect and midline shift. The brain magnetic resonance (MR) imaging demonstrated a large left temporal heterogeneously enhancing lesion with significant perilesional edema and mass effect. The patient underwent gross total removal of the lesion that proved to be an intracranial cavernous angioma. Postoperatively, he did well, exhibiting no residual neurological deficit, and has remained lesion and seizure-free.
Conclusion: This and 12 other cases in the literature focus on intracranial cavernous angiomas that could have been readily misdiagnosed as tumors. It confirms why obtaining appropriate preoperative MR and CT studies, followed by surgical intervention, is essential to confirm the correct underlying pathology and appropriately and optimally treat the patient.
Keywords: Cavernomas, Cavernous angioma, Giant cavernous malformation, Pediatric patients
INTRODUCTION
Intracranial cavernous malformations (CMs) are benign low-flow vascular lesions that make up to 10–25% of all vascular malformations, 70–80% are supratentorial.[
Most CMs are small and remain asymptomatic for long periods of time. Occasionally, supratentorial CMs will precipitate the new onset of seizures and headaches, while infratentorial CMs more typically lead to acute/progressive neurological deficits.[
Few giant CMs (GCMs) have been reported in the literature and may mimic intracranial neoplasms or other vascular malformations. Here, we present an 18-month-old male with a GCM and reviewed 12 other cases in the literature.
CASE REPORT
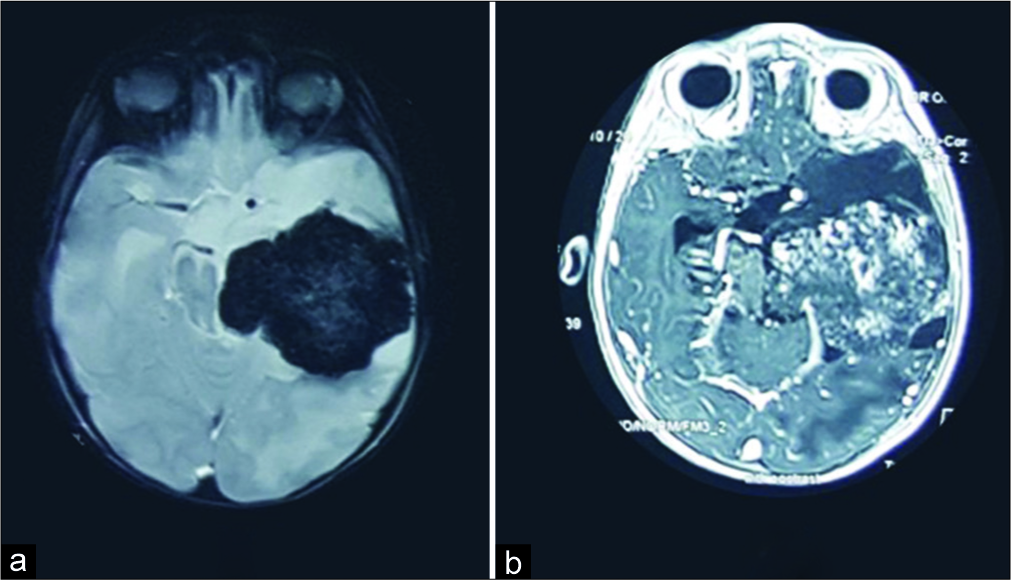
An 18-month-old male presented with the new onset of two seizures. Although the clinical examination was normal, both the computed tomography (CT) and magnetic resonance (MR) studies showed a large left temporal lesion with severe mass effect and midline shift. The enhanced MR further demonstrated heterogeneous enhancement (lesion >66 mm) and perilesional edema [
Figure 1:
Brain magnetic resonance imaging (MRI) of a left temporal giant cavernous angioma (a) MRI gradient spin echo weighted imaging showed a lesion with a diameter over 66 mm a hypo signal on gradient spin echo weighted imaging (b) brain MRI T1-weighted imaging with gadolinium injection showed a heterogeneous enhancement of a left temporal lesion with brain edema.
Surgery
The left temporal craniotomy revealed a large mass with distinct margins from the surrounding tissues accompanied by gliosis. The pathology was consistent with a cavernous angioma. Although the patient did well immediately postoperatively, 3 days later, he developed meningitis that was treated effectively with 3 weeks of antibiotics. Postoperatively, the patient remained neurologically intact without seizures. The subsequent CT studies 3 months later confirmed no recurrent lesion [
DISCUSSION
History
In 2004, Lawton et al. defined a giant cavernous angioma as a lesion with a diameter over 60 mm.[
Jhawar et al.[
Frequency
Cavernous angiomas are vascular benign malformations of the central nervous system.[
Lesion size and clinical presentation
Although these lesions are typically 9–20 mm, giant lesions also have been reported in the literature. In both children and adults, these lesions may first present with focal or generalized seizures followed by intracerebral bleeding and deficits reflecting lesion location. Rarely, pediatric cases of giant cavernomas have been reported in the literature [
CT and MR appearance
Typically, the MR imaging (MRI) appearance of a giant cavernous angioma is a heterogeneous “popcorn-like” mass with/without cysts reflecting various states of degradation of blood.[
Misdiagnosis of giant cavernous angioma
Giant cavernous angioma can be misdiagnosed on CT/MRI, as they mimic other intracranial neoplasms. Therefore, other differential diagnosis include gliomas, oligodendrogliomas, pilocytic astrocytoma, or with hemorrhagic metastasis.[
Surgery
The operation of choice is gross total excision, but this depends on lesion location. Stereotactic radiosurgery might be considered for deep sited lesions, but correlate with poor outcomes.[
Pathology
Giant cavernoma consists of a large ectatic endothelium-lined variable sizes vascular channels without mural muscular or elastic fibers embedded within a matrix of collagenous tissue. There are no neuronal cells or other components. Further, it is surrounded by hemosiderin deposits, gliosis, and sometimes calcification or thrombosis.[
CONCLUSION
Pediatric giant cavernous angioma is a rare intracranial lesion that may be best diagnosed with MR/CT. The best outcomes correlate with surgical excision, but maybe, limited by eloquent tumor location.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agrawal A, Banode P, Shukla S. Giant cavernous hemangiomas of the brain. Asian J Neurosurg. 2012. 7: 220-2
2. Avci E, Oztürk A, Baba F, Karabağ H, Cakir A. Huge cavernoma with massive intracerebral hemorrhage in a child. Turk Neurosurg. 2007. 17: 23-6
3. Chicani CF, Miller NR, Tamargo RJ. Giant cavernous malformation of the occipital lobe. J Neuroophthalmol. 2003. 23: 151-3
4. de Andrade GC, Prandini MN, Braga FM. Giant cavernous angioma: Report of two cases. Arq Neuropsiquiatr. 2002. 60: 481-6
5. Gezen F, Karatas A, Is M, Yildirim U, Aytekin H. Giant cavernous haemangioma in an infant. Br J Neurosurg. 2008. 22: 787-9
6. Jhawar S, Nadkarni T, Goel A. Giant cerebral cavernous hemangiomas: A report of two cases and review of the literature. Turk Neurosurg. 2012. 22: 226-32
7. Kawagishi J, Suzuki M, Kayama T, Yoshimoto T. Huge multilobular cavernous angioma in an infant: Case report. Neurosurgery. 1993. 32: 1028-30
8. Khalil T, Lemaire JJ, Chazal J, Verrelle P. Role of radiosurgery in the management of intracranial cavernomas. Review of the literature. Neurochirurgie. 2007. 53: 238-42
9. Khosla VK, Banerjee AK, Mathuriya SN, Mehta S. Giant cystic cavernoma in a child. Case report. J Neurosurg. 1984. 60: 1297-9
10. Lawton MT, Vates GE, Quinones-Hinojosa A, McDonald WC, Marchuk DA, Young WL. Giant infiltrative cavernous malformation: Clinical presentation, intervention, and genetic analysis: Case report. Neurosurgery. 2004. 55: 979-80
11. Ozsoy KM, Oktay K, Gezercan Y, Cetinalp NE, Olguner SK, Erman T. Giant cavernous malformations in childhood: A case report and review of the literature. Pediatr Neurosurg. 2017. 52: 30-5
12. Parizel MR, Menovsky T, Van Marck V, Lammens M, Parizel PM. Giant cavernous malformations in young adults: Report of two cases, radiological findings and surgical consequences. JBR-BTR. 2014. 97: 274-8
13. Siddiqui AA, Jooma R. Neoplastic growth of cerebral cavernous malformation presenting with impending cerebral herniation: A case report and review of the literature on de novo growth of cavernomas. Surg Neurol. 2001. 56: 42-5
14. Son DW, Lee SW, Choi CH. Giant cavernous malformation: A case report and review of the literature. J Korean Neurosurg Soc. 2008. 43: 198-200
15. van Lindert EJ, Tan TC, Grotenhuis JA, Wesseling P. Giant cavernous hemangiomas: Report of three cases. Neurosurg Rev. 2007. 30: 83-92