- Department of Neurosurgery, Health Sciences Center, Federal University of Espírito Santo, Brazil.
- Department of Pediatric Surgery, Hospital Infantil Nossa Senhora da Glória, Vitória, Espírito Santo, Brazil.
Correspondence Address:
Amanda Silva Guimarães, Department of Neurosurgery, Health Sciences Center, Federal University of Espirito Santo, Vitória, Espírito Santo, Brazil.
DOI:10.25259/SNI_804_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Amanda Silva Guimarães1, Mário Vaz Júnior2, Samuel Paiva Martins2, Walter J. Fagundes-Pereyra1. Rare case of migration and perforation of the urinary bladder by ventriculoperitoneal shunt catheter with intravesical knotted formation: A case report and literature review. 04-Mar-2022;13:75
How to cite this URL: Amanda Silva Guimarães1, Mário Vaz Júnior2, Samuel Paiva Martins2, Walter J. Fagundes-Pereyra1. Rare case of migration and perforation of the urinary bladder by ventriculoperitoneal shunt catheter with intravesical knotted formation: A case report and literature review. 04-Mar-2022;13:75. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11426
Abstract
Background: The most commonly used technique in the management of hydrocephalus is a neurosurgical procedure, known as ventriculoperitoneal shunt (VPS). Several complications of the distal end of a VPS catheter have been described in the literature, although migration and erosive bladder perforation of this shunt are extremely uncommon.
Case Description: We relate a rare pediatric case of a 4-year-old boy, with long-term dysuria, intermittent incontinence, and chronic abdominal pain developed during a myelomeningocele postoperative period, without other symptoms. A bladder fistula with the distal end of the VPS inside the bladder was observed while performing an ultrasound to investigate the urinary tract. Two months before the current surgical approach, the patient, with hydrocephalus and alterations compatible with Chiari malformation, was treated with VPS and subsequently subjected to the third ventriculostomy. The child was unsuccessfully treated with an infraumbilical laparotomy, with section and careful traction of the catheter. A vesicostomy was then performed and the catheter was observed to form an intravesical knot.
Conclusion: The intravesical knot formation is extremely rare and its mechanism of formation is still not well understood. Patients with VPS need adequate medical follow-up to identify possible complications of the shunt.
Keywords: Bladder perforation, Intravesical knot, Migration of the distal Ventriculoperitoneal shunt, Urinary and genital tract disorders, Ventriculoperitoneal shunt
INTRODUCTION
Ventriculoperitoneal shunt (VPS) is the technique most commonly used in the management of hydrocephalus, accounting for 0.6% of all pediatric hospitalizations.[
METHODS
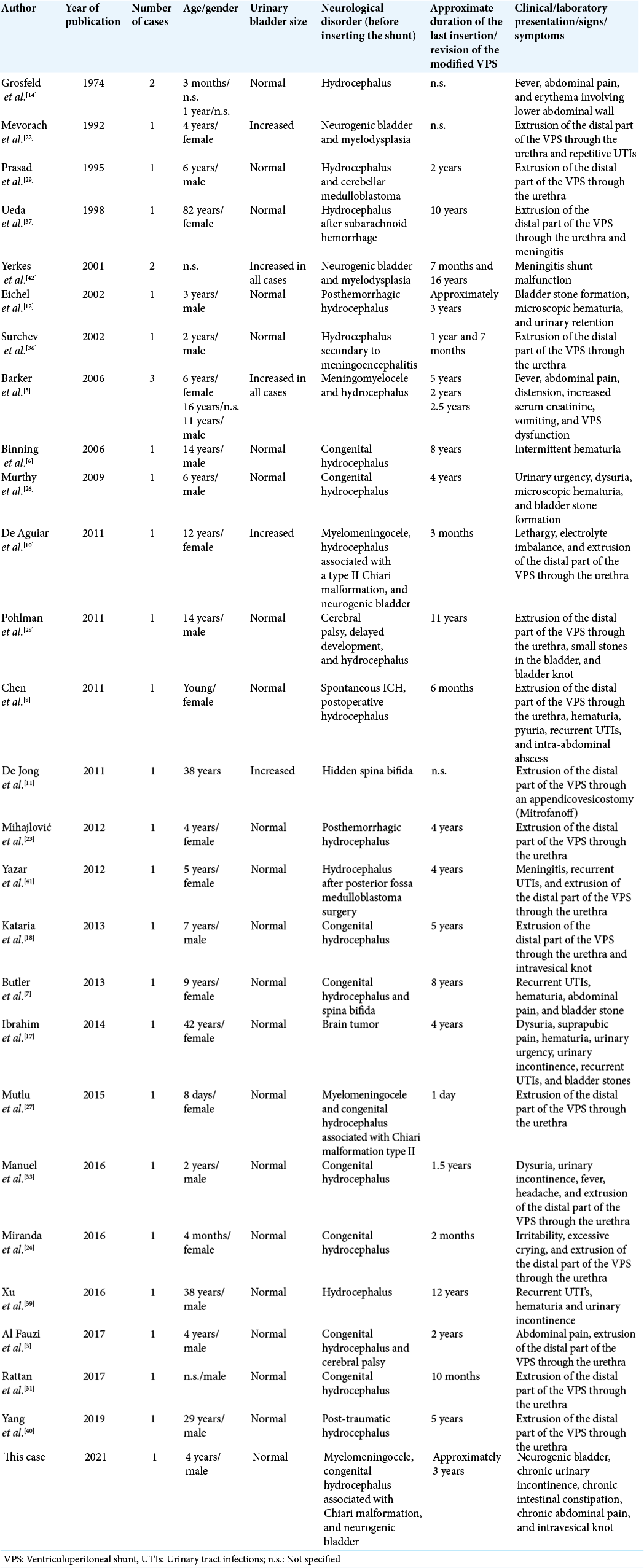
The study data were obtained retrospectively from the analysis and systematic review of the medical record in question and related literature. The Medline, Central, EMBASE, and Google Scholar databases were used to search keywords such as VPS, VPS, migration of the distal end of VPS, bladder perforation, intracorporeal knotting, and intravesical knotting, in articles published until March 30, 2021. The reference lists generated in the search were then filtered manually for relevance and the reports were selected to remove duplicates. One hundred and ninety-one studies on the migration of the distal end of VPS were found and 44 more relevant bibliographic references were used to write this review. The inclusion criteria for the study were the following: patients who, regardless of age, sex, race, bladder size, and etiology of hydrocephalus, had migration of the distal end of VPS into the bladder, with subsequent extrusion through the urethra or not; patients who had an intracorporeal knot formation at the distal end of the VPS; and patients who had stone formation or calcifications at the distal end of the VPS. The following data were extracted from studies that meet the inclusion criteria: name of the first author, year of publication, age and sex of the patient, clinical and laboratory data presentation, cause of hydrocephalus, size of the urinary bladder, interval since the last insertion of the VPS until revision of the altered VPS, and intervention used to conduct each case and the result.
CASE REPORT
A 4-year-old male patient was admitted to Hospital Infantil Nossa Senhora da Glória – Vitória, ES, Brazil, for the correction of a cerebrospinal fluid fistula and removal of the VPS after evidence of bladder fistula and presence of a catheter inside the bladder. On admission, the child presented increased head circumference, neurogenic bladder, long-term dysuria, constipation, and chronic abdominal pain because of myelomeningocele, but no other associated symptoms. The past pathologic history showed that at 10 months of age, the patient underwent surgery to correct myelomeningocele and for implantation of the right VPS because of hydrocephalus associated with Chiari malformation and that at 3 years of age, after the evidence of ventricular dilatation, the left VPS was inserted. It also showed that after 7 months of this last procedure, the child presented signs and symptoms of meningitis, which grew Escherichia coli ESBL in culture of the left VPS catheter tip, being the urine culture also positive for this bacterium. Therefore, he was treated with meropenem, the left VPS catheter was removed and the external ventricular drainage implanted, followed by an endoscopic third ventriculostomy. During an outpatient follow-up with the neurosurgery team, at 4 years of age, asymptomatic, a detailed physical examination was performed, and new imaging tests were requested, which showed effective control of hydrocephalus. During the same follow-up with the nephrology team, routine ultrasonography of the urinary tract and abdominal X-rays was ordered. A bladder fistula with a VPS catheter in the bladder was found, requiring hospitalization for surgery. In this current hospitalization, the patient was approached by the pediatric surgery and neurosurgery teams through infraumbilical laparotomy with a section of the catheter’s distal end and removal of the entire VPS system. After unsuccessfully performing careful tractions to remove the distal portion of the VPS from inside the bladder, they opted for a vesicostomy, at which point was possible to observe the catheter coiled with about eight turns in itself, well intricate and firm, forming an intravesical tangle. No calculus formation was observed and there was no extrusion of the distal catheter through the urethra. He was treated with antibiotic therapy with ceftriaxone and indwelling urinary catheterization for 10 days. The tip of the right VPS catheter was sent for culture, which was negative. The patient follows up on regular outpatient follow-up with neurosurgery and nephrology, progressing uneventfully and without neurological sequelae.
DISCUSSION
The VPS procedure is a well-established treatment modality for hydrocephalus.[
A case of migration of the distal end of the VPS catheter with intravesical knots formation, without body extrusion, or formation of calcification at the migration site is extremely rare, this being the first report found in the literature. Thirty-one cases in the literature [
Perforation of the urinary bladder through the distal portion of the VPS can be observed in both sexes, with 11 (35.48%) cases being female, 14 (45.16%) males, and six not specified in the reports. It has been reported at all ages, being the youngest case at 8 days old and the oldest at 82 years old; however, it has a higher incidence during childhood due to the VPS procedure being more prevalent at this age.
Some previous reports and discussions[
Five (16.2%) patients had the formation of intravesical stones. Considering that the process and time involved in the formation of a stone are long, it can be speculated that the shunt may remain asymptomatic inside the bladder for a long period before the diagnosis.[
Several theories have been proposed to explain the exact mechanism and facilitators for bladder perforation, such as bioreactivity of catheter components, local inflammatory reaction, infection, relatively rigid and sharp tipped catheters, continuous mechanical irritation at a fixed point on the bladder surface, thin wall of this organ in the pediatric age group, iatrogenic placement with inadvertent positioning of the distal end of the VPS, and long abdominal end of the catheter.[
The use of trocars to access the peritoneum for the implantation of the VPS system was associated with an increased risk of perforation of the viscera when compared to open procedures.[
The most prevalent clinical signs and symptoms were the extrusion of the distal part of the VPS through the urethra and those related to the urinary tract such as dysuria, urinary urgency, urinary retention, recurrent urinary tract infections, and abdominal pain. Extrusion of the distal portion of the catheter through the urethra was present in 17 (54.83%) patients. Symptoms related to the urinary tract were present in 11 (35.48%) patients; however, as many of them were chronic, a possible overlap of symptoms due to primary neurological disorder (neural tube defects) with symptoms caused by the intravesical catheter should be considered. It is pertinent, therefore, that patients with VPS with urinary symptoms undergo an ultrasound of the urinary and/or abdominal pathways.
Our patient was asymptomatic on admission, with no signs of catheter extrusion through the urethra on physical examination, with the vesical fistula and the presence of the distal end of the VPS inside the bladder only being evident after the abdominal radiography [
Among the most chosen procedures for surgical approach, there are gentle catheter traction, endoscopic surgery, and exploratory laparotomy.[
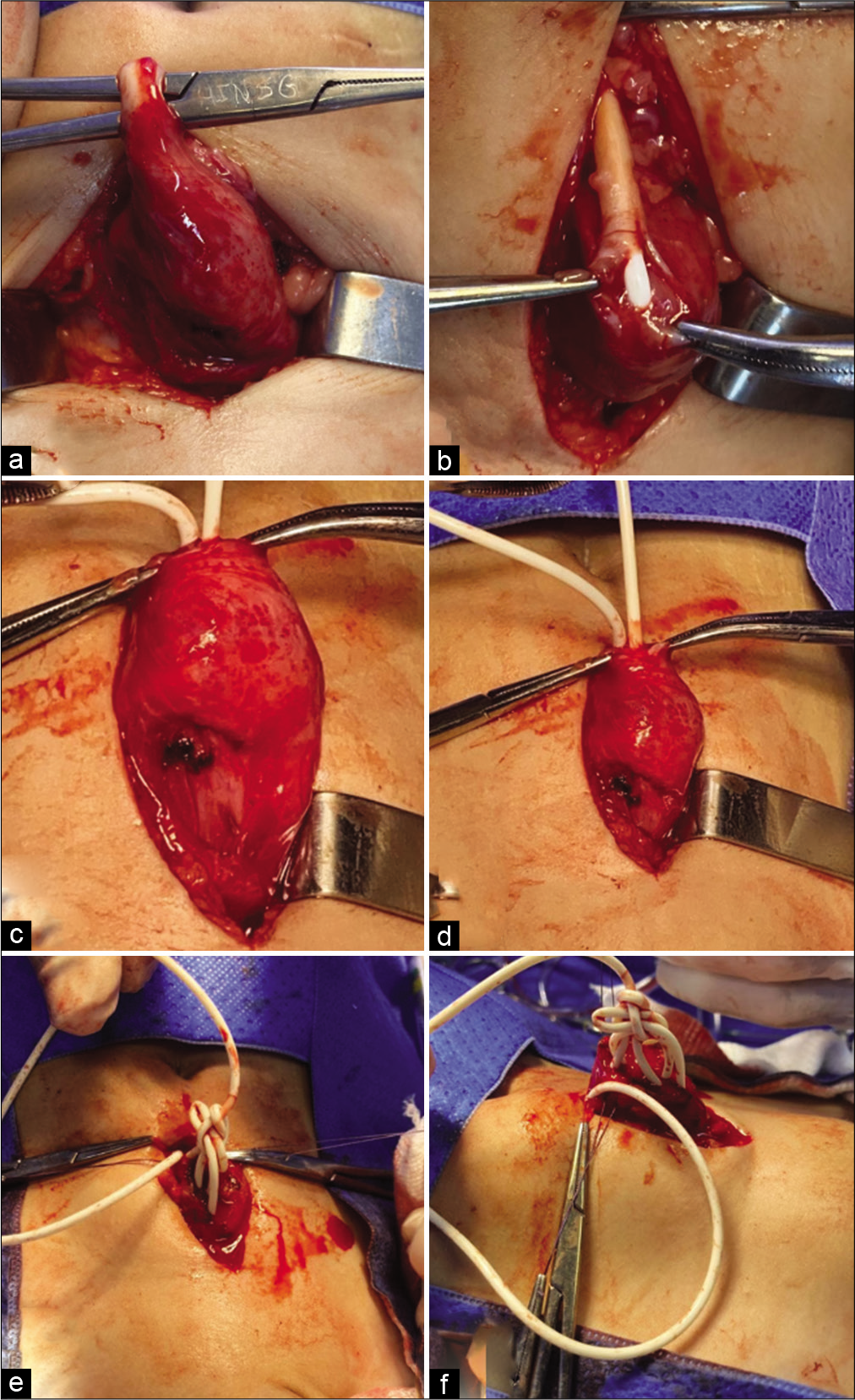
Here, it was decided to perform an exploratory laparotomy followed by successive and careful traction of the catheter that was inserted into the bladder, however, without success. Hence, it was decided to perform a vesicostomy. Finally, when removing the distal end of the catheter from the inside of the urinary bladder, a knot formation was observed [
Figure 3:
Intraoperative images showing the fibrous lining around the distal portion of the VPS that invaded the urinary bladder (a). Local dissection of the fibrous lining that circumcised the VPS catheter, fixing part of it to the urinary bladder (b). Careful traction of the catheter to remove it from the inside of the bladder (c and d). After vesicostomy, the formation of an intravesical ball (e and f) was observed. VPS: Ventriculoperitoneal shunt.
Pohlman et al. (2011) and Kataria et al. (2013) reported two cases that describe two intravesical knot formations. However, in both cases, the clinical presentation was the extrusion of the distal portion of the VPS catheter through the urethra. This case presented only a clinical picture with chronic symptoms characterized by dysuria, urinary incontinence, intestinal constipation, and abdominal pain, symptoms that have been followed for a long time due to a history of myelomeningocele hindering a directed urgent approach. There were no signs and symptoms of meningitis or peritonitis.
The intraoperative findings showed a fibrous lining around the distal portion of the VPS that invaded the bladder [
The possible causes for the formation of the rare and spontaneous intravesical knot that was found could be: effects of retained memory of the catheter, causing it to return to the position it was in the package when supplied; peristaltic bowel movements; increased intra-abdominal pressure; pulsation of cerebrospinal fluid; and pulsations of nearby blood vessels. However, the mechanisms by which the formation of intravesical knot occurs are still not fully understood.[
CONCLUSION
Migration and perforation of the urinary bladder through the distal end of the VPS are quite unusual, unpredictable, and unavoidable conditions. The formation of intravesical knots is extremely rare and its mechanism of formation is still not well understood. Patients with VPS need adequate medical follow-up to identify possible complications of the shunt. Although it is a rare condition, perforation of the urinary bladder by the VPS catheter should be considered as a differential diagnosis in patients who, concurrently with the use of VPS, present urinary symptoms. It is recommended that urinary tract ultrasound and/or abdominal ultrasound are performed in these cases, guiding a more effective immediate management, thus avoiding a late diagnosis that leads to unwanted complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to Mr. Gabriel Bouchabki Destri and Mr. Matheus Figueira for their support in technical editing and linguistic review.
References
1. Agarwal M, Adhana R, Namdev H, Yadav YR, Agrawal T. Transoral extrusion of the ventriculo-peritoneal shunt: A case report and review of literature. J Pediatr Neurosci. 2011. 6: 149-51
2. Agarwal R, Allen A, Green L. Ventriculoperitoneal shunt catheter migration in a patient with breast implants resulting in a peri-implant cerebrospinal fluid pseudocyst. Radiol Case Rep. 2018. 14: 221-5
3. Al Fauzi A, Djatisoesanto W, Wahyuhadi J, Parenrengi MA, Turchan A. A rare case of repeated migration and transurethral extrusion of ventriculoperitoneal shunt. J Pediatr Neurosci. 2017. 12: 96-8
4. Allouh MZ, Al Barbarawi MM, Asfour HA, Said RS. Migration of the distal catheter of the ventriculoperitoneal shunt in hydrocephalus: A comprehensive analytical review from an anatomical perspective. Clin Anat. 2017. 30: 821-30
5. Barker GM, Läckgren G, Stenberg A, Arnell K. Distal shunt obstruction in children with myelomeningocele after bladder perforation. J Urol. 2006. 176: 1726-8
6. Binning MJ, Ragel BT, Walker ML, Kestle JR. Retained peritoneal shunt tubing causing hematuria: Case illustration. J Neurosurg. 2006. 104: 434
7. Butler L, Keys C, Lam JP. Bladder calculus formation on the tip of a migrated disused ventriculoperitoneal shunt. J Pediatr Surg. 2013. 48: E1-3
8. Chen TH, Lin MS, Kung WM, Hung KS, Chiang YH, Chen CH. Combined ventriculoperitoneal shunt blockage, viscus perforation with migration into urethra, presenting with repeated UTI. Ann R Coll Surg Engl. 2011. 93: 151-3
9. Chugh A, Gotecha S, Amle G, Patil A, Punia P, Kotecha M. Abnormal migration and extrusion of abdominal end of ventriculoperitoneal shunt: An experience of eight cases. J Pediatr Neurosci. 2018. 13: 317-21
10. de Aguiar GB, Mizrahi C, Aquino JH, Tavares CM, Telles C, Nigri F. Urethral extrusion of a peritoenal catheter in a patient with neobladder: A rare complication of shunt insertion. Neuropediatrics. 2011. 42: 124-7
11. de Jong L, van der AA, de Ridder D, van Calenbergh F. Extrusion of ventriculoperitoneal shunt catheter through an appendicovesicostomy. Br J Neurosurg. 2011. 25: 115-6
12. Eichel L, Allende R, Mevorach RA, Hulbert WC, Rabinowitz R. Bladder calculus formation and urinary retention secondary to perforation of a normal bladder by a ventriculoperitoneal shunt. Urology. 2002. 60: 344
13. Glatstein MM, Roth J, Scolnik D, Haham A, Rimon A, Koren L. Late presentation of massive pleural effusion from intrathoracic migration of a ventriculoperitoneal shunt catheter: Case report and review of the literature. Pediatr Emerg Care. 2012. 28: 180-2
14. Grosfeld JL, Cooney DR, Smith J, Campbell RL. Intraabdominal complications following ventriculoperitoneal shunt procedures. Pediatrics. 1974. 54: 791-6
15. Hermann EJ, Zimmermann M, Marquardt G. Ventriculoperitoneal shunt migration into the pulmonary artery. Acta Neurochir (Wien). 2009. 151: 647-52
16. Houten JK, Smith S, Schwartz AY. Vaginal migration of ventriculoperitoneal shunt catheter and cerebrospinal fluid leak as a complication of hysterectomy. World Neurosurg. 2017. 104: 1046.e13-4
17. Ibrahim AK. Urinary bladder stone complicating ventriculovesical shunt. Sultan Qaboos Univ Med J. 2014. 14: e142-4
18. Kataria R, Sinha VD, Chopra S, Gupta A, Vyas N. Urinary bladder perforation, intra-corporeal knotting, and per-urethral extrusion of ventriculoperitoneal shunt in a single patient: Case report and review of literature. Childs Nerv Syst. 2013. 29: 693-7
19. Khalatbari H, Parisi MT. Management of hydrocephalus in children: Anatomic imaging appearances of CSF shunts and their complications. AJR Am J Roentgenol. 2021. 216: 187-99
20. Kim D, Kim HY, Jin SC, Lee S. Disappearance of a distal shunt catheter: A case report of an unusual cause of shunt malfunction. Korean J Neurotrauma. 2020. 16: 79-84
21. Low SW, Sein L, Yeo TT, Chou N. Migration of the abdominal catheter of a ventriculoperitoneal shunt into the mouth: A rare presentation. Malays J Med Sci. 2010. 17: 64-7
22. Mevorach RA, Hulbert WC, Merguerian PA, Rabinowitz R. Perforation and intravesical erosion of a ventriculoperitoneal shunt in a child with an augmentation cystoplasty. J Urol. 1992. 147: 433-4
23. Mihajlović M, Tasić G, Raičević M, Mrdak M, Petrović B, Radlović V. Asymptomatic perforation of large bowel and urinary bladder as a complication of ventriculoperitoneal shunt: Report of two cases. Srp Arh Celok Lek. 2012. 140: 211-5
24. Miranda ME, de Sousa MB, Tatsuo ES, Quites LV, Giannetti AV. Bladder perforation by ventriculoperitoneal shunt. Childs Nerv Syst. 2016. 32: 2321-6
25. Mohammadi A, Hedayatiasl A, Ghasemi-Rad M. Scrotal migration of a ventriculoperitoneal shunt: A case report and review of literature. Med Ultrason. 2012. 14: 158-60
26. Murthy KV, Reddy S, Prasad DV. Perforation of the distal end of the ventriculoperitoneal shunt into the bladder with calculus formation. Pediatr Neurosurg. 2009. 45: 53-5
27. Mutlu M, Kader S, Aslan Y, Yazar U, Imamoglu M. An acute complication of ventriculoperitoneal shunt with bladder perforation and extrusion through the urethra in a newborn: Case report and review of the literature. Pediatr Neurosurg. 2015. 50: 264-9
28. Pohlman GD, Wilcox DT, Hankinson TC. Erosive bladder perforation as a complication of ventriculoperitoneal shunt with extrusion from the urethral meatus: Case report and literature review. Pediatr Neurosurg. 2011. 47: 223-6
29. Prasad VS, Krishna AM, Gupta PK. Extrusion of peritoneal catheter of ventriculoperitoneal shunt through the urethra. Br J Neurosurg. 1995. 9: 209-10
30. Ralston A, Johnson A, Ziemer G, Frim DM. Transcardiac migration of ventriculoperitoneal shunt requiring open cardiac surgery: Case report and review of the literature. Childs Nerv Syst. 2017. 32: 703-7
31. Rattan KN, Hooda R, Khursheed A, Gupta S. Extrusion of peritoneal end of ventriculoperitoneal shunt through urethra in an infant: A rare complication. Ped Urol Case Rep. 2017. 4: 395-8
32. Riccardello GJ, Barr LK, Bassani L. Bowel perforation presenting with acute abdominal pain and subcutaneous emphysema in a 14-year-old girl with an abandoned distal peritoneal shunt catheter: Case report. J Neurosurg Pediatr. 2016. 18: 325-8
33. See MC, Chua ME, Dy JS. A rare cause of pediatric urinary incontinence: Ventriculoperitoneal shunt with bladder perforation. Pediatr Urol Case Rep. 2016. 3: 76-83
34. Sharifian A, Abdollahi A, Maddah G, Anaraki F, Alvandipour M, Sahebi MA. Spontaneous transanal protrusion of ventriculoperitoneal catheter: A case report. Acta Med Iran. 2013. 51: 135-8
35. Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JR. Hospital care for children with hydrocephalus in the United States: Utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr. 2008. 1: 131-7
36. Surchev J, Georgiev K, Enchev Y, Avramov R. Extremely rare complications in cerebrospinal fluid shunt operations. J Neurosurg Sci. 2002. 46: 100-2
37. Ueda Y, Kakino S, Hashimoto O, Imoto K. Perforation of the bladder by a peritoneal catheter: An unusual late complication of ventriculo-peritoneal shunt. No Shinkei Geka. 1998. 26: 413-6
38. Vivek K, Tarun G, Gaurav J. Urinary bladder perforation and per-urethral extrusion of lumbo-peritoneal shunt in a patient: Case report and review literature. J Spine Neurosurg. 2015. 4: 1-3
39. Xu S, Sheng W, Qiu Y, Wang J. An unusual complication of ventriculoperitoneal shunt: Urinary bladder stone case report and literature review. Iran Red Crescent Med J. 2016. 18: e26049
40. Yang X, Liang R, Zhang Y. An unusual complication of ventriculoperitoneal shunt with bladder perforation and extrusion through the urethra orifice in an adult male patient. Int J Neurosci. 2019. 129: 101-2
41. Yazar U, Kanat A, Akca N, Gazioglu G, Arda IS, Kazdal H. Urethral protrusion of the abdominal catheter of ventriculoperitoneal shunt: Case report of extremely rare complication. J Pediatr Neurosci. 2012. 7: 111-3
42. Yerkes EB, Rink RC, Cain MP, Leurssen TG, Casale AJ. Shunt infection and malfunction after augmentation cystoplasty. J Urol. 2001. 165: 2262-4
43. Yilmaz MB, Egemen E, Tonge M, Kaymaz M. Transoral protrusion of a peritoneal catheter due to gastric perforation 10 years after a ventriculoperitoneal shunting: Case report and review of the literature. Turk Neurosurg. 2013. 23: 285-8